Abstract
Background
The clinical signs of adrenal cortical insufficiency (incidence, ca. 25 per million per year; prevalence, ca. 400 per million) are nonspecific, and misdiagnoses are therefore common. Glucocorticoid substitution therapy has been in use for 50 years but is not a wholly adequate treatment. Our understanding of this disease remains incomplete in many ways.
Methods
We selectively searched the Medline database for publications on adrenal cortical insufficiency, with particular attention to studies from the year 2000 onward (search terms: “adrenal insufficiency” or “Addison‘s disease” or “hypopituitarism”).
Results
Hydrocortisone substitution therapy is often given in doses of 10–25 mg/day, timed according to the circadian rhythm. Gastrointestinal and other, febrile infections account for 30–50% of life-threatening adrenocortical crises. Such crises affect 8 of 100 persons with adrenal cortical insufficiency per year and must be treated by the immediate administration of glucocorticoids and fluids. When persons with adrenal cortical insufficiency are acutely ill or are otherwise under unusual stress, they may need additional amounts of hydrocortisone, often in the range of 5–10 mg but occasionally as high as 200 mg. The sustained administration of excessive amounts of steroid can shorten patients lives by several years. Inappropriate substitution therapy can cause other major medical conditions, such as metabolic syndrome and osteoporosis.
Conclusion
Important measures for the prevention of adrenocortical crises include improved care by treating physicians, education of patients and their families, the provision of emergency identifying documents, and the prescription of glucocorticoid emergency kits.
Primary adrenal cortical insufficiency, known as adrenal insufficiency (AI) or Addisons disease, is rare with a prevalence of approximately 100/1 million/year (1, 2). The incidence of primary AI is approximately 5/1 million/year and has been rising in recent years (1– 3) (e1). Autoimmune-mediated adrenalitis accounts for over 80% of cases in industrialized countries (2). Most patients are young to middle-aged, with more females than males affected. However, this disease affects patients of all ages and in patients under 30 years there is no sex disparity (e2).
Irreversible damage to the adrenal cortex leads to insufficient production of glucocorticoids, mineralocorticoids, and androgens. Over the course of their illness, nearly 60% of patients with autoimmune-mediated AI will be diagnosed with further autoimmune diseases as part of a polyglandular autoimmune syndrome (table 1).
Table 1. Causes of adrenal cortical insufficiency.
| Causes | Notes |
| Primary adrenal cortical insufficiency (AI) | |
| Isolated autoimmune adrenalitis | Autoimmune adrenalitis = most common cause of primary AI in Western countries (>80%), of which 30-40% as isolated disease, 21-Hydroxylase antibody often positive |
| Polyglandular autoimmune syndrome Type 1 |
Hypoparathyroidism, chronic mucocutaneous candidiasis, other autoimmune diseases, lymphomas (rare), mutation in the AIRE gene, autosomal recessive |
| Polyglandular autoimmune syndrome Type 2 |
Hypo/hyperthyroid, premature ovarian failure,vitiligo, type 1 diabetes mellitus, pernicious anemia, association with HLA-DR3 (approximately 60% of patients with autoimmune adrenalitis) |
| Infections | Tuberculosis (most common cause in developing countries), CMV, HIV, Mycosis (e.g. histoplasmosis) |
| Bilateral adrenal hemorrhage | Meningococcal sepsis, primary antiphospholipid syndrome, septic shock |
| Extensive adrenal metastases | e.g. renal, lung, breast, gastric, or colon carcinomas, lymphoma |
| Bilateral adrenalectomy | – |
| Drugs | e.g. mitotane, etomidate, ketoconazole, fluconazole can cause AI. Rifampicin, phenytoin, barbiturate, carbamazepine accelerate cortisol metabolism |
| Adrenogenital syndrome (AGS) | congenital enzyme defect of steroid biosynthesis (21a-hydroxylase [95%], 11 b-hydroxylase, and others), autosomal recessive, salt deficiency (75%), virilization in girls |
| Adrenoleukodystrophy | neurological disturbances (frequent), hypogonadism, X-linked recessive trait, mutation in the X-ALD gene, accumula tion of long chain fatty acids (>C24) |
| Familial glucocorticoid resistance | – |
| Familial glucocorticoid deficiency | genetic ACTH insensitivity, type 1-3 FGD |
| Congenital adrenal hypoplasia | Hypogonadotropic hypogonadism, X-linked mutation in the DAX-1 gene |
| Triple A syndrome | Achalasia, alacrima, neurological disturbances, autosomal recessive mutation in the triple-A gene |
| Secondary adrenal cortical insufficiency | |
| Tumors of the pituitary and hypothalamus regions |
e.g., pituitary adenoma, Rathke‘s cyst, craniopharyngioma, meningioma, metastases |
| Pituitary / hypothalamic surgery | – |
| Radiation to the pituitary and hypothalamus regions |
– |
| Pituitary infarction / Sheehan syndrome | – |
| Autoimmune hypophysitis | lymphocytic, IgG4 associated, drug associated (e.g. ipilimumab, tremelimumab), xanthomatous |
| Granulomatous disease | Sarcoidosis, histiocytosis X, Wegeners granulomatosis |
| Infections | Abcess, tuberculous meningitis |
| Traumatic brain injury | – |
| Genetic causes | e.g. mutations in PROP-1, LHX-4, HESX1, TPIT, POMC genes |
| Isolated ACTH deficiency | Autoimmune, mutations in PC-1, POMC, or TPIT genes |
| Tertiary adrenal cortical Insufficiency | |
| Chronic glucocorticoid therapy | – |
| Endogenous Cushings disease | – |
| Isolated CRH deficiency | – |
CRH, corticotropin releasing hormone; CMV, cytomegalovirus; HIV, human immunodeficiency virus; ACTH, adrenocorticotropic hormone
The secondary form of adrenal cortical insufficiency is caused by a dysfunction at the level of the pituitary (incidence: 20/1 million/year; prevalence 400/1 million). The main causes are the displacement of corticotropic cells by pituitary macroadenomas or traumatic injury (table 1) (4, e3). A deficiency of adrenocorticotropic hormone (ACTH) blocks the stimulation of cortisol production. The adrenal cortex atrophies, and cortisol secretion dwindles. Due to the variety of causes, there is no peak incidence according to age or sex.
By far, the most common cause of adrenal cortical insufficiency is pharmacotherapy with synthetic glucocorticoids (0.5 to 2% of the population) (5). Such therapy can lead to suppression of the hypothalamic-pituitary-adrenal axis (HPA axis) with atrophy of the corticotropic cells of the pituitary gland and the adrenal cortex (tertiary adrenal cortical insufficiency). High-dose steroid therapy (20–30 mg prednisolone equivalent) can lead to suppression of the regulatory cycle after just a few days (6, e4). In general, the risk of adrenal cortical insufficiency increases with the dose and duration of therapy. Depot preparations and evening administration of higher glucocorticoid doses also increase the risk. Adrenocorticosuppression is difficult to predict in individual cases, hence all patients, even those receiving low-dose glucocorticoid therapy, must be generally considered at risk for the development of adrenal cortical insufficiency (7).
The current article aims to provide new insight into the management of patients with adrenal cortical insufficiency. A selective literature search of Medline was performed with special focus on recent studies published since the year 2000 (search words: “adrenal insufficiency“ or „Addisons disease“ or „hypopituitarism”). The search yielded 451 articles, and relevant articles were selected.
Clinical information and diagnosis
The typical symptoms of adrenal cortical insufficiency are presented in table 2 (8). In cases of secondary adrenal cortical insufficiency, depending on the underlying condition, there is often complete hypopituitarism with additional signs of growth, sexual, or thyroid hormone dysfunction.
Table 2. Symptoms and laboratory changes in adrenal cortical insufficiency (AI).
| Hormone | Symptoms |
|
ACTH (POMC) stimulation (primary AI) |
Hyperpigmentation |
|
ACTH (POMC) suppression (secondary/tertiary AI) |
Pale complexion |
| Glucocorticoid deficiency | Fatigue and decreased performance |
| Appetite / Weight loss | |
| Nausea, vomiting, and abdominal pain | |
| Myalgias and joint pain | |
| Orthostatic hypotension | |
| Anemia, lymphocytosis, eosinophilia | |
| Hypoglycemia / hypoglycemic tendency | |
| Hyponatremia (no inhibition of ADH secretion) | |
| Hypercalcemia | |
| Slight TSH increase | |
|
Mineralocorticoid deficiency (primary AI) |
Hypotonia, hypovolemia, creatinine increase, orthostatic dysregulation |
| Hyponatremia | |
| Hyperkalemia | |
| Salt hunger | |
| Androgen deficiency | Loss of axillary and pubic hair (females) |
| Dry skin (females) | |
| Depression, loss of libido (females) |
ACTH, adrenocorticotropic hormone; ADH, antidiuretic hormone; POMC, proopiomelanocortin; TSH, thyroid stimulating hormone
The diagnosis of adrenal cortical insufficiency is made by the combination of low morning blood cortisol level (<100 nmol/L; 3.6 µg/dL) and/or an insufficient cortisol increase to less than 500 nmol/L (<18 µg/dL) after intravenous administration of 250µg ACTH1–24. The insulin tolerance test (ITT) is considered the gold standard (cortisol increase >500 nmol/L is considered normal); however, its implementation is more arduous. In terms of using basal hormone levels to make a diagnosis, ACTH levels are elevated in primary adrenal cortical insufficiency while levels are low or low-normal in secondary AI (1). The majority of patients with autoimmune mediated primary adrenal insufficiency show evidence of 21-hydroxylase antibodies in the serum (e5); however, this test can be foregone since a positive result has no therapeutic consequence.
In terms of imaging, the gold standard to diagnose secondary adrenal cortical insufficiency is magnetic resonance imaging of the pituitary and hypothalamus regions with contrast in 2 mm cuts. In addition, an ophthalmologic investigation to rule out chiasmal syndrome is advisable in cases of macroadenoma (>1 cm).
Problems can emerge after long-term pharmacotherapy with glucocorticoids or after treatment for endogenous hypercortisolism, even in cases of apparently sufficient endogenous cortisol production or glucocorticoid replacement. Symptoms mimic those of adrenal cortical insufficiency and are referred to as steroid withdrawal syndrome (e6) (box 1). The etiology remains unclear; however, relative glucocorticoid resistance mediated through a reduction of glucocorticoid receptors is suspected. The evaluation of endogenous cortisol production is only indicated when test results would have therapeutic consequences, e.g., before discontinuation of therapy or prior to planned surgery. To avoid distorted results, the clinician should ensure a sufficient time interval between testing and the last glucocorticoid administration (at least 4 to 5 plasma half-lives of the glucocorticoid administered, i.e. with hydrocortisone at least 18, and better 24 hours), as well as a sufficiently reduced daily dose (<15 to 20 mg hydrocortisone or <3 to 4 mg prednisolone per day). The tests administered are those listed above.
Box 1. Common triggering factors for adrenal crisis and frequency by percent*.
Gastrointestinal infection (22–33%)
Other febrile infections (17–24%)
Surgery (7–16%)
Intense physical activity (7–8%)
Psychological stress (4–6%)
*according to (18)
Hormone replacement therapy
Glucocorticoids
Academic research in the area of glucocorticoid replacement demonstrates a low level of evidence (placebo-controlled trials are impossible because patients die without replacement). However, a great deal of evidence is available from clinical practice.
Physiological cortisol profile and the effects of cortisol—Glucocorticoids have pleomorphic effects on metabolism, including an increase in blood glucose, protein catabolism, activation of bony metabolism with a net reduction of bone mass, and immunomodulatory effects. Acute events such as physical or emotional stress, inflammatory diseases, or injuries can rapidly multiply cortisol levels. Basal secretion is subject to a circadian rhythm, with peak levels in the early morning and a secretion nadir around midnight. These physiologic regulatory mechanisms (9) complicate both the interpretation of basal cortisol values for diagnostic endocrinology and also replacement therapy, which must ideally be adapted to individual circumstances as well as the time of day (10).
History and glucocorticoids used to date for the treatment of adrenal cortical insufficiency—Although Thomas Addison characterized the clinical picture of his namesake disease or primary adrenal cortical insufficiency already in 1855 (e7), it was not until 1936 with the discovery of cortisol by Kendall, Wintersteiner, and Reichenstein and the subsequent chemical synthesis of the hormone that the foundations for replacement therapy were laid.
Current glucocorticoid replacement therapy, dosage, and clinical monitoring—The standard daily replacement dose is between 10 and 25 mg of conventional hydrocortisone (= cortisol). To reproduce the circadian rhythm it is divided into two or three separate doses with approximately two thirds of the entire dose given in the morning (e.g., 10–5–5–0 or 15–5–0–0 mg). Patients with secondary adrenal cortical insufficiency often need slightly lower doses than patients with primary AI. Replacement therapy with prednisolone is also an option. Because of its more extended and powerful action, prednisolone is taken in a single morning dose of 3 to 5 mg, as the biological potency is some six times that of hydrocortisone (e8). The dosing of glucocorticoids as hormone replacement therapy cannot be monitored through hormonal or biochemical parameters. The foundations of therapy supervision are based instead on specific patient history (quality of life, capabilities, inabilities, recurrence and frequency of adrenal crises) and clinical parameters (weight monitoring, development of Cushingoid symptoms, bone density measurements) (4, 10).
Adjustment for stress, illness, and surgery—When adrenal cortical insufficiency is present, the rapid cortisol increase in response to illness and stress occurring physiologically fails to take place. Thus, the replacement dose must be temporarily increased by 10 to 25 mg. The following recommendations are empirically documented: additional intake of 5 to 10 mg hydrocortisone for prolonged physical activity or increased psychological stress (10). In cases of infection, fever, or minor surgical procedures, the daily dose should be increased to 30 to 75 mg (twice or three times the customary dose) (4, 10). For surgery, childbirth, or intensive treatment, the recommended dose is 100 to 200 mg per day, and for sepsis, 200 to 300 mg per day. During the third trimester of pregnancy, the daily dose should be increased to 25 to 35 mg (11). The dose should also be increased in cases of manifest hyperthyroidism (1). In septic ICU patients with previously healthy adrenals, a hydrocortisone dose (initial 100 mg, followed by 10 mg/hr for at least 7 days) is recommended on the assumption of a relative cortisol deficiency only in cases of septic shock refractory to volume or catecholamine administration (12) (e9).
Interaction with other medications/therapies: By affecting the key enzyme of cortisol metabolism, CYP3A4, various medications and foods can influence hydrocortisone effects by augmenting (e.g., ritonavir, diltiazem, fluoxetine, grapefruit, licorice) or diminishing (e.g., antiepileptics, barbiturates, rifampicin, exenatide) its effect (13) (e10). Hydrocortisone can also decrease the anticoagulation effects of coumarin derivatives as well as increase blood levels of cyclosporine (13). In patients with type 1 diabetes mellitus, it is important to account for the effects of cortisol on glucose metabolism. To avoid nocturnal hypoglycemia, low-dose administration of hydrocortisone in the evening can be useful (14).
Mineralocorticoid therapy—Mineralocorticoid replacement is needed on a regular basis only in patients with primary adrenal cortical insufficiency. Replacement is with fludrocortisone, given in a single dose between 0.05 and 0.1 mg. Treatment is monitored using blood pressure (target: normal values), electrolytes (target: normalized serum Na and K values), and renin concentration (target: upper normal range) measurement. A reduction of the fludrocortisone dose in cases of hypertension, and an increase in dose during pregnancy and extremely hot weather should be considered (1, 10).
Therapy with dihydroepiandrosterone (DHEA)—In both primary and secondary adrenal cortical insufficiency there is a deficiency of DHEA. DHEA acts indirectly through bioconversion into androgens, and directly with DHEA-mediated neurosteroidal and immunomodulatory effects (e11). Clinical studies have shown a positive influence of DHEA on mood, sexuality, and health-related quality of life; however, meta-analysis attributes this only moderate value (15). An oral morning dose of 25 to 50 mg DHEA in women with adrenal cortical insufficiency brings serum androgen levels up into the normal female range (16, 17). Positive effects and clinical signs, e.g., regrowth of secondary hair or improved skin moisture, should only be expected after months of therapy and show high inter-individual variation. Treatment monitoring consists of determining the serum DHEA S-levels and serum androgens. DHEA administration must be decided on an individual basis, and succeeds only when despite optimal adjustment of glucocorticoid replacement a persistent marked limitation of general health or libido is present. The patient should also be informed that this is an off-licence therapy, which is not reimbursed by statutory health insurance companies in Germany.
Shortcomings of current therapy
Morbidity
Adrenal crisis—Acute adrenal crisis is a life-threatening condition, which will affect approximately one in 13 patients over the course of each year (18) (for causes, cf. Box 1). Despite established glucocorticoid replacement therapy, adrenal crisis remains one of the most common causes of death among patients with chronic adrenal cortical insufficiency (19). The symptoms of adrenal crisis include fatigue, nausea and vomiting, and hypotension and are thus non-specific, which can lead to misdiagnosis. However, the prognosis of acute adrenal crisis is critically dependent on rapid parenteral administration of hydrocortisone (or other glucocorticoids) by the attending physician, regardless of the underlying illness. Not administering corticosteroids in a crisis situation, e.g., out of concern for potential immunosuppression in cases of infection, is medical malpractice. The most important element of crisis prevention and management is the intensive and continuing instruction of patients and the people surrounding them.
Treatment for acute adrenal crisis is immediate replacement of glucocorticoids (100 mg hydrocortisone IV followed by another infusion of 100 to 200 mg hydrocortisone over 24 hours) and fluids. Depending on the triggering event, additional treatment appropriate to the situation, e.g., antibiotic therapy, is also necessary. Immediate initiation of therapy may under no circumstances be delayed while waiting for laboratory results.
Osteoporosis—High glucocorticoid replacement doses over 25 to 30 mg hydrocortisone per day provoke bony changes, i.e. osteoporosis (20). As doses are lowered (<25 mg hydrocortisone per day), so are the case numbers of osteoporosis (21). Synthetic steroids such as prednisolone, because of their higher potency (e8), appear to have more substantial effects on bone (21).
Metabolic cardiovascular risk factors—The physiologic circadian rhythm of cortisol affects fluctuations in glucose tolerance at various times of the day. In secondary adrenal cortical insufficiency, the dose amount of daily glucocorticoid replacement correlates with increased body mass index, high cholesterol and triglyceride levels, and an increased prevalence of diabetes mellitus (22, 23). Hydrocortisone administration after 5 pm induces greater insulin resistance than morning administration (9).
Quality of Life—In patients with adrenal cortical insufficiency, quality of life is significantly restricted compared to that of the healthy general population (24). However, this seems not to depend on the type of glucocorticoid taken or the frequency of hydrocortisone dosing (25, 26). Instead, it appears that dose quantity and the non-physiological timing in administration of the glucocorticoid are responsible (27).
Mortality
Inadequate steroid adjustment in stressful situations as well as chronic over-dosing lead to a 1.5 to 2-fold increase in mortality (reduced life expectancy in females approximately three years and in males approximately 11 years [19]). Leading causes of death are adrenal crisis (at least 25%), infections, cardiovascular disease, and malignancy (28, 29). There is particular risk for patients diagnosed under the age of 40 and for patients with concomitant type 1 diabetes mellitus (19, 28).
Patients with secondary adrenal cortical insufficiency also show an increased mortality rate, which appears to be produced by cardiovascular events (30– 32). Hydrocortisone replacement doses >25 mg in particular lead to increased mortality (33).
Improvements in current therapy
Prevention of adrenal crises
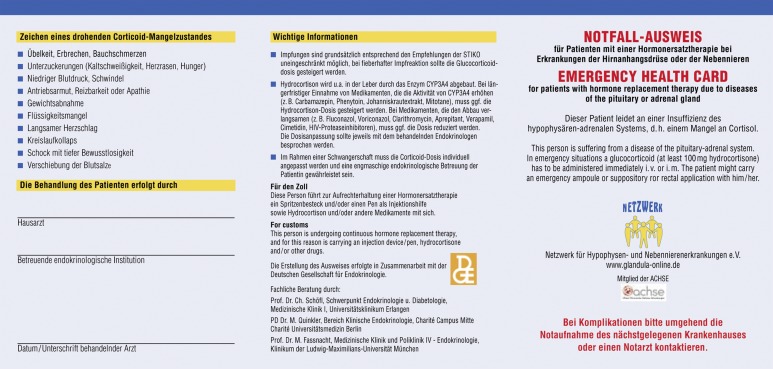
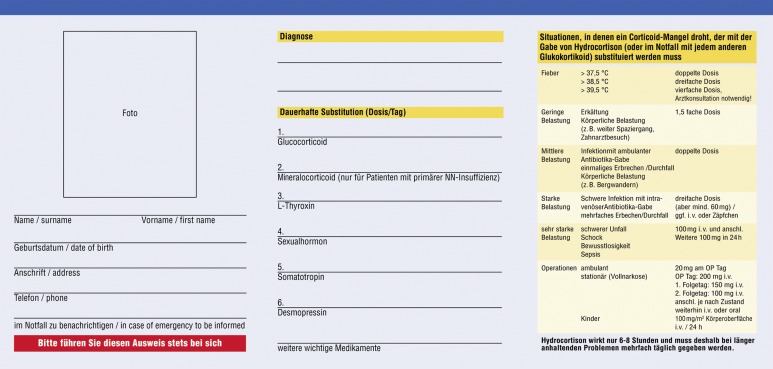
The information, explanation, and continuing instruction of patients and members of their household regarding the disease and treatment as well as recognition of adrenal crisis are essential (10, 34). Appropriate behavior and self-adjustment of replacement dosage contribute to prevention and management of emergency situations. The most common mistake is waiting in the case of infection and the belated increase in hydrocortisone replacement. In addition, many physicians do not recognize the presentation of an adrenal crisis. In a critical situation, any glucocorticoid in any form of application may be administered (oral, rectal, intravenous, or intramuscular). Every patient should have an emergency identification card (eFigure 1) available on which emergency instructions and contact details of an experienced endocrinologist are listed (box 2). A European emergency card is now available (eFigure 2). Each patient should also be equipped with an “emergency kit,” and receive appropriate instructions regarding its use (box 2) (10, 35).
eFigure 1.
Box 2. Strategies to prevent adrenal crisis*.
Emergency identification card
-
Continuing education of patient and family
Dose adjustment in stressful situations / discussion of typical stress situations (fever, trauma, surgery)
Vomiting and diarrhea as urgent indications for parenteral glucocorticoid administration
Symptoms of acute adrenal insufficiency
Prescribing a hydrocortisone “emergency kit“ (e.g., 100 mg hydrocortisone 21-hemisuccinate as ampoules and glucocorticoid suppositories, e.g., 100 mg prednisolone suppositories)
Instruction in self-injecting hydrocortisone
See also www.endokrinologie.net/krankheiten-glukokortikoide.php (German website), the section „Nebenniere, Steroide und Hypertonie“ (adrenal, steroids, and hypertension) of the German Society for Endocrinology (DGE)
eFigure 2.
New medications
Although none of the available glucocorticoid preparations can fully mimic the circadian rhythm of cortisol, there are some new developments.
Delayed release preparations
Hydrocortisone with modified release (5 and 20 mg tablets)—This new form of hydrocortisone replacement has been approved in several European countries (including Germany) since the end of 2012 for the treatment of adrenal cortical insufficiency in adults. It consists of an outer shell with rapid-release hydrocortisone surrounding a core with a delayed-release preparation. It is taken in a single dose daily in the morning. In the randomized controlled licensing study for approval, use of the extended-release form significantly improved quality of life, blood pressure, and metabolic profiles (36).
Prednisone with modified Release (1, 2, and 5 mg tablets)—This delayed-release prednisone tablet is taken evenings around 10 pm and begins to work around 3 am. The preparation is approved for patients with rheumatoid arthritis. In a small, open label study, this tablet produced improvements in morning fatigue and complaints compared to conventional preparations of prednisolone taken at 8 am by patients with adrenal cortical insufficiency (37).
Hydrocortisone with delayed release—This delayed-action hydrocortisone tablet is also taken in the evening and acts in the early morning hours (38, 39); however, it is still in development.
Hydrocortisone pump therapy—The continuous administration of hydrocortisone by a pump significantly improved quality of life for seven patients in a pilot study. A larger study is currently planned in Norway. Through pump therapy, hydrocortisone administration closely approximates the physiological profile (27, 40).
Key Messages.
Adrenocortical insufficiency is a rare but life-threatening disease with various causes.
Hydrocortisone is the first choice for glucocorticoid replacement, in which a rigid treatment schedule should be rejected for a flexible day-to-day modification (e.g., ±5 mg hydrocortisone).
Complications occur because of replacement doses set too low (adrenal crises) or too high (metabolic syndrome, osteoporosis). Monitoring of therapy is performed primarily according to clinical criteria.
Infectious diseases are the main risk for the development of adrenal crisis, and they must be treated early and vigorously. In cases of diarrhea and vomiting, immediate parenteral administration of 100 mg hydrocortisone is necessary.
Continuing instruction of patients and relatives is essential. Patients should be supplied with an emergency identification card and an emergency kit.
eFigure 3.
Acknowledgments
Translated from the original German by Sarah P. Halberg MD.
Footnotes
Conflict of interest statement:
All involved authors are participating in a register study sponsored by Viropharma Inc.
Prof. Quinkler works as a consultant for Viropharma Inc. He received reimbursement of conference participation fees, travel and accommodation costs, as well as fees for the preparation of scientific meetings from Viropharma.
Prof. Beuschlein received reimbursement of travel and accommodation costs from Viropharma, and he received fees for the preparation of scientific meetings for Viropharma.
Dr. Hahner works as a consultant for Viropharma Inc. She received reimbursement for travel and accommodation costs, as well as fees for the preparation of scientific meetings for Viropharma.
Dr. Meyer received reimbursement for conference, travel, and accommodation costs from Lilly and Ipsen.
Prof. Schöfl received fees for consulting from Viropharma.
Prof. Stalle declares that aside from participating in the sponsored register study, there are no conflicts of interest.
References
- 1.Arlt W, Allolio B. Adrenal insufficiency. Lancet. 2003;361:1881–1893. doi: 10.1016/S0140-6736(03)13492-7. [DOI] [PubMed] [Google Scholar]
- 2.Betterle C, Morlin L. Autoimmune Addison‘s disease. Endocr Dev. 2011;20:161–172. doi: 10.1159/000321239. [DOI] [PubMed] [Google Scholar]
- 3.Lovas K, Husebye ES. High prevalence and increasing incidence of Addison‘s disease in western Norway. Clin Endocrinol (Oxf) 2002;56:787–791. doi: 10.1046/j.1365-2265.2002.t01-1-01552.x. [DOI] [PubMed] [Google Scholar]
- 4.Grossman AB. Clinical Review: The diagnosis and management of central hypoadrenalism. J Clin Endocrinol Metab. 2010;95:4855–4863. doi: 10.1210/jc.2010-0982. [DOI] [PubMed] [Google Scholar]
- 5.Henzen C, Suter A, Lerch E, Urbinelli R, Schorno XH, Briner VA. Suppression and recovery of adrenal response after short-term, high-dose glucocorticoid treatment. Lancet. 2000;355:542–545. doi: 10.1016/S0140-6736(99)06290-X. [DOI] [PubMed] [Google Scholar]
- 6.Schlaghecke R, Kornely E, Santen RT, Ridderskamp P. The effect of long-term glucocorticoid therapy on pituitary-adrenal responses to exogenous corticotropin-releasing hormone. N Engl J Med. 1992;326:226–230. doi: 10.1056/NEJM199201233260403. [DOI] [PubMed] [Google Scholar]
- 7.Dinsen S, Baslund B, Klose M, et al. Why glucocorticoid withdrawal may sometimes be as dangerous as the treatment itself. Eur J Intern Med. 2013:S0953–S6205. doi: 10.1016/j.ejim.2013.05.014. [DOI] [PubMed] [Google Scholar]
- 8.Bleicken B, Hahner S, Ventz M, Quinkler M. Delayed diagnosis of adrenal insufficiency is common: a cross-sectional study in 216 patients. Am J Med Sci. 2010;339:525–531. doi: 10.1097/MAJ.0b013e3181db6b7a. [DOI] [PubMed] [Google Scholar]
- 9.Plat L, Leproult R, L‘Hermite-Baleriaux M, Fery F, Mockel J, Polonsky KS, Van CE. Metabolic effects of short-term elevations of plasma cortisol are more pronounced in the evening than in the morning. J Clin Endocrinol Metab. 1999;84:3082–3092. doi: 10.1210/jcem.84.9.5978. [DOI] [PubMed] [Google Scholar]
- 10.Quinkler M, Hahner S. What is the best long-term management strategy for patients with primary adrenal insufficiency? Clin Endocrinol (Oxf) 2012;76:21–25. doi: 10.1111/j.1365-2265.2011.04103.x. [DOI] [PubMed] [Google Scholar]
- 11.Lebbe M, Arlt W. What is the best diagnostic and therapeutic management strategy for an Addison patient during pregnancy? Clin Endocrinol (Oxf) 2013;78:497–502. doi: 10.1111/cen.12097. [DOI] [PubMed] [Google Scholar]
- 12.Dellinger RP, Levy MM, Rhodes A, et al. Surviving Sepsis Campaign: international guidelines for management of severe sepsis and septic shock, 2012. Intensive Care Med. 2013;39:165–228. doi: 10.1007/s00134-012-2769-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Debono M, Ross RJ, Newell-Price J. Inadequacies of glucocorticoid replacement and improvements by physiological circadian therapy. Eur J Endocrinol. 2009;160:719–729. doi: 10.1530/EJE-08-0874. [DOI] [PubMed] [Google Scholar]
- 14.Meyer G, Hackemann A, Reusch J, Badenhoop K. Nocturnal hypoglycemia identified by a continuous glucose monitoring system in patients with primary adrenal insufficiency (Addison‘s Disease) Diabetes Technol Ther. 2012;14:386–388. doi: 10.1089/dia.2011.0158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Alkatib AA, Cosma M, Elamin MB, et al. A systematic review and meta-analysis of randomized placebo-controlled trials of DHEA treatment effects on quality of life in women with adrenal insufficiency. J Clin Endocrinol Metab. 2009;94:3676–3681. doi: 10.1210/jc.2009-0672. [DOI] [PubMed] [Google Scholar]
- 16.Hahner S, Allolio B. Dehydroepiandrosterone to Enhance Physical Performance: Myth and Reality. Endocrinol Metab Clin North Am. 2010;39:127–139. doi: 10.1016/j.ecl.2009.10.008. [DOI] [PubMed] [Google Scholar]
- 17.Hahner S, Allolio B. Therapeutic management of adrenal insufficiency. Best Pract Res Clin Endocrinol Metab. 2009;23:167–179. doi: 10.1016/j.beem.2008.09.009. [DOI] [PubMed] [Google Scholar]
- 18.Hahner S, Loeffler M, Bleicken B, et al. Epidemiology of adrenal crisis in chronic adrenal insufficiency - the need for new prevention strategies. Eur J Endocrinol. 2010;162:597–602. doi: 10.1530/EJE-09-0884. [DOI] [PubMed] [Google Scholar]
- 19.Erichsen MM, Lovas K, Fougner KJ, et al. Normal overall mortality rate in Addison‘s disease, but young patients are at risk of premature death. Eur J Endocrinol. 2009;160:233–237. doi: 10.1530/EJE-08-0550. [DOI] [PubMed] [Google Scholar]
- 20.Lovas K, Gjesdal CG, Christensen M, et al. Glucocorticoid replacement therapy and pharmacogenetics in Addison‘s disease: effects on bone. Eur J Endocrinol. 2009;160:993–1002. doi: 10.1530/EJE-08-0880. [DOI] [PubMed] [Google Scholar]
- 21.Koetz KR, Ventz M, Diederich S, Quinkler M. Bone mineral density is not significantly reduced in adult patients on low-dose glucocorticoid replacement therapy. J Clin Endocrinol Metab. 2012;97:85–92. doi: 10.1210/jc.2011-2036. [DOI] [PubMed] [Google Scholar]
- 22.Dullaart RP, Schols JL, van der SG, Zelissen PM, Sluiter WJ, van Beek AP. Glucocorticoid replacement is associated with hypertriglyceridemia, elevated glucose and higher non-HDL cholesterol, and may diminish the association of HDL cholesterol with the -629C > A CETP promoter polymorphism in growth hormone-receiving hypopituitary patients. Clin Endocrinol (Oxf) 2008;69:359–366. doi: 10.1111/j.1365-2265.2008.03196.x. [DOI] [PubMed] [Google Scholar]
- 23.Filipsson H, Monson JP, Koltowska-Haggstrom M, Mattsson A, Johannsson G. The impact of glucocorticoid replacement regimens on metabolic outcome and comorbidity in hypopituitary patients. J Clin Endocrinol Metab. 2006;91:3954–3961. doi: 10.1210/jc.2006-0524. [DOI] [PubMed] [Google Scholar]
- 24.Hahner S, Loeffler M, Fassnacht M, et al. Impaired subjective health status in 256 patients with adrenal insufficiency on standard therapy based on cross-sectional analysis. J Clin Endocrinol Metab. 2007;92:3912–3922. doi: 10.1210/jc.2007-0685. [DOI] [PubMed] [Google Scholar]
- 25.Bleicken B, Hahner S, Loeffler M, Ventz M, Allolio B, Quinkler M. Impaired subjective health status in chronic adrenal insufficiency: impact of different glucocorticoid replacement regimens. Eur J Endocrinol. 2008;159:811–817. doi: 10.1530/EJE-08-0578. [DOI] [PubMed] [Google Scholar]
- 26.Bleicken B, Hahner S, Loeffler M, et al. Influence of hydrocortisone dosage scheme on health-related quality of life in patients with adrenal insufficiency. Clin Endocrinol (Oxf) 2010;72:297–304. doi: 10.1111/j.1365-2265.2009.03596.x. [DOI] [PubMed] [Google Scholar]
- 27.Lovas K, Husebye ES. Continuous subcutaneous hydrocortisone infusion in Addison‘s disease. Eur J Endocrinol. 2007;157:109–112. doi: 10.1530/EJE-07-0052. [DOI] [PubMed] [Google Scholar]
- 28.Bergthorsdottir R, Leonsson-Zachrisson M, Oden A, Johannsson G. Premature mortality in patients with Addison‘s disease: a population-based study. J Clin Endocrinol Metab. 2006;91:4849–4853. doi: 10.1210/jc.2006-0076. [DOI] [PubMed] [Google Scholar]
- 29.Smans LC, Souverein PC, Leufkens HG, Hoepelman AI, Zelissen PM. Increased use of antimicrobial agents and hospital admission for infections in patients with primary adrenal insufficiency: a cohort study. Eur J Endocrinol. 2013;168:609–614. doi: 10.1530/EJE-12-0879. [DOI] [PubMed] [Google Scholar]
- 30.Rosen T, Bengtsson BA. Premature mortality due to cardiovascular disease in hypopituitarism. Lancet. 1990;336:285–288. doi: 10.1016/0140-6736(90)91812-o. [DOI] [PubMed] [Google Scholar]
- 31.Gaillard RC, Mattsson AF, Akerblad AC, et al. Overall and cause-specific mortality in GH-deficient adults on GH replacement. Eur J Endocrinol. 2012;166:1069–1077. doi: 10.1530/EJE-11-1028. [DOI] [PubMed] [Google Scholar]
- 32.Sherlock M, Ayuk J, Tomlinson JW, et al. Mortality in patients with pituitary disease. Endocr Rev. 2010;31:301–342. doi: 10.1210/er.2009-0033. [DOI] [PubMed] [Google Scholar]
- 33.Sherlock M, Reulen RC, Alonso AA, et al. ACTH deficiency, higher doses of hydrocortisone replacement, and radiotherapy are independent predictors of mortality in patients with acromegaly. J Clin Endocrinol Metab. 2009;94:4216–4223. doi: 10.1210/jc.2009-1097. [DOI] [PubMed] [Google Scholar]
- 34.Repping-Wuts HJ, Stikkelbroeck NM, Noordzij A, Kerstens M, Hermus AR. A glucocorticoid education group meeting: an effective strategy for improving self-management to prevent adrenal crisis. Eur J Endocrinol. 2013;169:17–22. doi: 10.1530/EJE-12-1094. [DOI] [PubMed] [Google Scholar]
- 35.Hahner S, Burger-Stritt S, Allolio B. Subcutaneous hydrocortisone administration for emergency use in adrenal insufficiency. Eur J Endocrinol. 2013;169:147–154. doi: 10.1530/EJE-12-1057. [DOI] [PubMed] [Google Scholar]
- 36.Johannsson G, Nilsson AG, Bergthorsdottir R, et al. Improved cortisol exposure-time profile and outcome in patients with adrenal insufficiency: a prospective randomized trial of a novel hydrocortisone dual-release formulation. J Clin Endocrinol Metab. 2012;97:473–481. doi: 10.1210/jc.2011-1926. [DOI] [PubMed] [Google Scholar]
- 37.Langenheim J, Ventz M, Hinz A, Quinkler M. Modified-release prednisone decreases complaints and fatigue compared to standard prednisolone in patients with adrenal insufficiency. Horm Metab Res. 2013;45:96–101. doi: 10.1055/s-0032-1316293. [DOI] [PubMed] [Google Scholar]
- 38.Newell-Price J, Whiteman M, Rostami-Hodjegan A, Darzy K, Shalet S, Tucker GT, Ross RJ. Modified-release hydrocortisone for circadian therapy: a proof-of-principle study in dexamethasone-suppressed normal volunteers. Clin Endocrinol (Oxf) 2008;68:130–135. doi: 10.1111/j.1365-2265.2007.03011.x. [DOI] [PubMed] [Google Scholar]
- 39.Debono M, Ghobadi C, Rostami-Hodjegan A, et al. Modified-release hydrocortisone to provide circadian cortisol profiles. J Clin Endocrinol Metab. 2009;94:1548–1554. doi: 10.1210/jc.2008-2380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Merza Z, Rostami-Hodjegan A, Memmott A, et al. Circadian hydrocortisone infusions in patients with adrenal insufficiency and congenital adrenal hyperplasia. Clin Endocrinol (Oxf) 2006;65:45–50. doi: 10.1111/j.1365-2265.2006.02544.x. [DOI] [PubMed] [Google Scholar]
- E1.Willis AC, Vince FP. The prevalence of Addison‘s disease in Coventry, UK. Postgrad Med J. 1997;73:286–288. doi: 10.1136/pgmj.73.859.286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E2.Myhre AG, Undlien DE, Lovas K, et al. Autoimmune adrenocortical failure in Norway autoantibodies and human leukocyte antigen class II associations related to clinical features. J Clin Endocrinol Metab. 2002;87:618–623. doi: 10.1210/jcem.87.2.8192. [DOI] [PubMed] [Google Scholar]
- E3.Reimondo G, Bovio S, Allasino B, Terzolo M, Angeli A. Secondary hypoadrenalism. Pituitary. 2008;11:147–154. doi: 10.1007/s11102-008-0108-4. [DOI] [PubMed] [Google Scholar]
- E4.Axelrod L. Glucocorticoid therapy. Medicine (Baltimore) 1976;55:39–65. doi: 10.1097/00005792-197601000-00003. [DOI] [PubMed] [Google Scholar]
- E5.Husebye E, Lovas K. Pathogenesis of primary adrenal insufficiency. Best Pract Res Clin Endocrinol Metab. 2009;23:147–157. doi: 10.1016/j.beem.2008.09.004. [DOI] [PubMed] [Google Scholar]
- E6.Schofl C, von zur MA. Vermeidung unerwünschter Wirkungen einer Glukokortikoidtherapie [Preventing adverse side-effects of glucocorticoid therapy] Internist. 1997;38:371–378. doi: 10.1007/s001080050050. [DOI] [PubMed] [Google Scholar]
- E7.Addison T. London: Samuel Highley; 1855. On the constitutional and local effects of disease of the supra-renal capsules. [Google Scholar]
- E8.Caldato MC, Fernandes VT, Kater CE. One-year clinical evaluation of single morning dose prednisolone therapy for 21-hydroxylase deficiency. Arq Bras Endocrinol Metabol. 2004;48:705–712. doi: 10.1590/s0004-27302004000500017. [DOI] [PubMed] [Google Scholar]
- E9.Marik PE, Pastores SM, Annane D, et al. Recommendations for the diagnosis and management of corticosteroid insufficiency in critically ill adult patients: consensus statements from an international task force by the American College of Critical Care Medicine. Crit Care Med. 2008;36:1937–1949. doi: 10.1097/CCM.0b013e31817603ba. [DOI] [PubMed] [Google Scholar]
- E10.Fujita Y, Kitamura T, Otsuki M, et al. Exenatide alters absorption of hydrocortisone in a diabetic patient with panhypopituitarism: iatrogenic adrenal insufficiency. Diabetes Care. 2013 doi: 10.2337/dc12-1499. 36 e8. doi: 10.2337/dc12-1499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E11.Hazeldine J, Arlt W, Lord JM. Dehydroepiandrosterone as a regulator of immune cell function. J Steroid Biochem Mol Biol. 2010;120:127–136. doi: 10.1016/j.jsbmb.2009.12.016. [DOI] [PubMed] [Google Scholar]
- E12.Dahlqvist P, Bensing S, Ekwall O, Wahlberg J, Bergthorsdottir R, Hulting AL. [A national medical emergency card for adrenal insufficiency A new warning card for better management and patient safety] Lakartidningen. 2011;108:2226–2227. [PubMed] [Google Scholar]