Fig. 1.
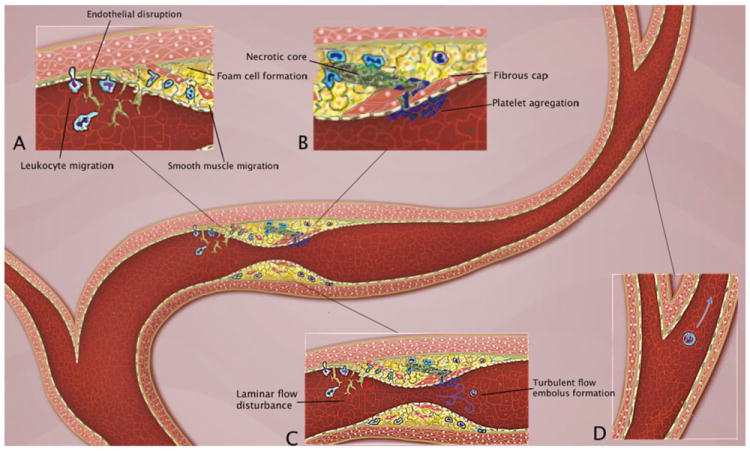
Pathophysiology of intracranial atherosclerosis. A The endothelial injury and increased permeability induced by factors such as hypertension and smoking generates adhesion of monocytes and lymphocytes to the disrupted vessel lining, followed by migration beneath the endothelial surface and cellular aggregation in the subendothelial tissue. Macrophages take up lipid, forming foam cells, and these and other macrophages are activated and cytokines and growth factors are released, leading to smooth muscle cell migration and proliferation. B There is formation of a fibrous cap that covers a mixture of leukocytes, lipid, and necrotic tissue. Eventually the fibrous cap ruptures and ulcerates generating platelet aggregation and embolus formation. C The early endothelial injury generates disturbances of the laminar flow, which creates flow separation and oscillatory shear stress. This precipitates a cycle of further endothelial and arterial wall damage. Stenosis of the vessel lumen, in concert with embolus generation, produces strokes in a complementary occurrence of hypoperfusion and embolism (D)
