Abstract
Objective
The objective of this study was to evaluate the outcomes of patients after carotid endarterectomy (CEA) who developed postoperative hypertension or hypotension requiring the administration of intravenous vasoactive medication (IVMED).
Methods
We examined consecutive, primary elective CEA performed by 128 surgeons within the Vascular Study Group of New England (VSGNE) database (2003-2010) and compared outcomes of patients who required postoperative IVMED to treat hyper- or hypotension with those who did not. Outcomes included perioperative death, stroke, myocardial infarction (MI), congestive heart failure (CHF), hospital length of stay, and 1-year stroke or death. Propensity score matching was performed to facilitate risk-adjusted comparisons. Multivariable regression models were used to compare the association between IVMED and outcomes in unmatched and matched samples. Factors associated with use of IVMED in postoperative hypertension and hypotension were evaluated, and predictive performance of multivariable models was examined using receiver operating characteristic (ROC) curves.
Results
Of 7677 elective CEAs identified, 23% received IVMED for treatment of either postoperative hypertension (11%) or hypotension (12%). Preoperative neurological symptomatic status (20%) was similar across cohorts. In the crude sample, the use of IVMED to treat postoperative hypertension was associated with increased 30-day mortality (0.7% vs 0.1%; P < .001), stroke (1.9% vs 1%; P = .018), MI (2.4% vs 0.5%; P < .001), and CHF (1.9% vs 0.5%; P < .001). The use of IVMED to treat postoperative hypotension was also associated with increased perioperative mortality (0.8% vs 0.1%; P < .001), stroke (3.2% vs 1.0%; P < .001), MI (2.7% vs 0.5%; P < .001), and CHF (1.7% vs 0.5%; P < .001), as well as 1-year death (5.1% vs 2.9%; P < .001) or stroke (4.2% vs 2.1%; P < .001). Hospital length of stay was significantly longer among patients who needed IVMED for postoperative hypertension (2.8 ± 4.7 days vs 1.7 ± 5.5 days; P < .001) and hypotension (2.8 ± 5.9 days vs 1.7 ± 5.5 days; P < .001). In multivariable analysis, IVMED for postoperative hyper-tension was associated with increased MI, stroke, or death (odds ratio, 2.6; 95% confidence interval [CI], 1.6-4.1; P < .001). Similarly, IVMED for postoperative hypotension was associated with increased MI, stroke, or death (odds ratio, 3.2; 95% CI, 2.1-5.0; P < .001), as well as increased 1-year stroke or death (hazard ratio, 1.6; 95% CI, 1.2-2.2; P = .003). Smoking, coronary artery disease, and clopidogrel (ROC, 0.59) were associated with postoperative hypertension requiring IVMED, whereas conventional endarterectomy and general anesthesia were associated with postoperative hypotension requiring IVMED (ROC, 0.58). The unitization of IVMED varied between 11% and 38% across VSGNE, and center effect did not affect outcomes.
Conclusions
Postoperative hypertension requiring IVMED after CEA is associated with increased perioperative mortality, stroke, and cardiac complications, whereas significant postoperative hypotension is associated with increased perioperative mortality, cardiac, or stroke complications, as well as increased 1-year death or stroke following CEA. The utilization of IVMED varied across centers and, as such, further investigation into this practice needs to occur in order to improve outcomes of these at-risk patients.
Carotid endarterectomy (CEA) is effective in preventing stroke in the setting of symptomatic1-3 and asymptomatic atherosclerotic carotid artery stenosis.4,5 Blood pressure fluctuation after CEA is common and is thought to be related to alteration in baroreceptor function due to surgical dissection and possible effect of carotid cross-clamping.6-9 Significant hypertension has been reported in up to 56%6-8 and hypotension in up to 40% of patients undergoing CEA.10,11
Hemodynamic instability after CEA often requires the use of intravenous vasoactive medication (IVMED) and may lead to prolonged intensive care unit and hospital stay.9,11,12 Hypertension may potentially lead to wound hematoma, cardiac and cerebral complications, and exacerbate the sequelae of cerebral hyperperfusion syndrome.7,8 Hypotension, likewise, may cause decreased myocardial and cerebral perfusion that may result in myocardial infarction (MI) and ischemic stroke.13 Despite these concerns, the short- and long-term clinical effects of postoperative hemodynamic changes remain uncertain.7,8,10,11,13 Some authors have reported increased mortality and complication rates in patients after CEA who developed postoperative hemodynamic changes,7,8,10,11 while others observed no differences in outcomes.10,13 Using a large clinical database, we sought to evaluate the clinical course of patients who developed significant postoperative hypertension or hypotension following CEA.
METHODS
Patients
Using the Vascular Study Group of New England (VSGNE) database, we evaluated patients who underwent primary CEA. The VSGNE is a regional cooperative quality improvement initiative organized in 2002 to prospectively study patients treated with vascular interventions aiming to improve regional outcomes in vascular surgery. The details of this registry have been published previously,14 and additional information is available at www.vsgne.org. The Institutional Review Board at Boston University School of Medicine has approved the use of deidentified data for this study.
We queried the database for those patients who experienced postoperative hypertension or hypotension and were treated with IVMED after primary CEA. The study cohort included consecutive primary elective CEA performed by 128 surgeons practicing at 30 academic and community hospitals. Of the 8711 CEAs performed between 2003 and 2010, we excluded nonelective CEA (n = 969), those missing information for postoperative IVMED (n = 8), and those who received postoperative IVMED for both hypertension and hypotension (n = 57).
Outcome and variable definitions
We reviewed the demographics, pre-existing medical comorbidities, and operative details for these patients. More than 100 demographic and clinical variables were collected prospectively for each procedure and entered into the VSGNE database.14 Definitions of medical comorbidities in VSGNE have been previously published.14 We defined clinically significant postoperative hypertension or hypotension as the need for the administration of IVMED such as phenylephrine, dopamine, nitroglycerine, or nitroprusside either intermittently or as a continuous infusion in the postoperative period following CEA. Patients who received only intraoperative vasoactive agents were not included. The exact vasoactive medication used, the dosage, duration of treatment, and exact triggers for administration were not recorded in the database.
Main outcomes included perioperative death, MI, congestive heart failure (CHF), stroke (combination of ipsilateral and contralateral stroke), hospital length of stay (LOS), and a composite outcome of MI, stroke, or death. In addition, we also evaluated 1-year outcomes of survival and stroke. MI was defined in the database as new electrocardiographic ST and T wave changes on electrocardiogram, troponin elevation, or documentation by echocardiogram or other imaging modality. CHF was defined as new pulmonary edema documented by chest radiograph and requiring treatment or monitoring in the intensive care unit (www.vsgne.org).
Statistical analysis
Outcomes were compared based on administration of IVMED to treat either postoperative hypertension or hypotension after CEA. Baseline characteristics were compared between patients who received IVMED for postoperative hypertension with those who did not receive IVMED for treatment of either postoperative hypertension or hypotension using χ2 test for categorical variables and Student t-test for continuous variables. Similar analyses were performed comparing patients who received IVMED for postoperative hypotension with those who did not.
Additional analyses were performed using propensity score matching to select patients for comparison between these groups. The two propensity-matched cohorts included 621 patients who underwent CEA who received IVMED for postoperative hypertension with 2484 CEA patients who did not; and 629 CEA patients who required IVMED for postoperative hypotension with 2516 CEA patients who did not. Propensity scores were calculated based on the following factors that were significant in bivariate analysis in these two different groups of patients; IVMED for postoperative hypertension: age, smoking, hypertension, coronary artery disease (CAD), diabetes, preoperative beta blocker use, and type of procedure (conventional CEA vs eversion CEA); Use of IVMED for postoperative hypotension: CAD, chronic obstructive pulmonary disease (COPD), beta-blocker use, type of procedure, and type of anesthesia used. These scores were used to select two pairs of evenly matched groups using 1 to 4 ratios for comparison.
Separate multivariable analyses were performed for the crude study sample and the propensity-score-matched cohorts. Factors identified in previous VSGNE studies to be associated with cardiac complications after CEA (age, smoking, diabetes, CAD, COPD, abnormal stress test, beta-blocker use, and creatinine >1.8 mg/dL)15 and stroke or death (age >80, hypertension, ipsilateral carotid stenosis, contralateral carotid stenosis >70%, symptom status)16 were incorporated into the multivariable models. To account for the possible effect of individual practice pattern on postoperative outcomes, the utilization of IVMED was compared with χ2 test in all centers performing CEA in VSGNE. Additionally, generalized estimating equations analyses accounting for possible within-center correlation of subjects were performed for the main outcome measures: MI, stroke, and a composite outcome of MI, stroke, or death in the crude CEA sample.
Multivariable logistic regression models were used to examine the risk factors associated with the need of treatment with IVMED for postoperative hypertension or hypotension. Factors that were thought to be clinically associated with use of the medications and those found to be significant in bivariable analysis with P < .2 were entered into the initial prediction models. Then, using the backward elimination procedure with alpha level to remain in the model at .5, the more parsimonious models were constructed. The predictive performance of the models was examined using area under receiver operating characteristic (ROC) curves. Analysis was performed using SAS 9.2 software (SAS Institute, Cary, NC).
RESULTS
Characteristics of the crude cohort
The study cohort included 7677 consecutive primary elective CEA in 7096 patients. IVMED were required in 11% (824) of CEA to treat postoperative hypertension and in 12% (942) of CEA to treat postoperative hypotension. Seventy seven percent (5911) of CEAs were not associated with the administration of IVMED to treat either hypertension or hypotension. Demographic characteristics and preoperative medications of the crude cohort are listed in Table I. Overall, 20% of patients were treated for symptomatic carotid artery stenosis, 89% underwent conventional CEA, and 89% of procedures were performed under general anesthesia. Intraoperative carotid shunt and patch were used in 45% and 86% of procedures, respectively.
Table I.
Demographic, clinical, and procedural variables of patients treated with intravenous vasoactive medications (IVMED) for hypertension and hypotension
| Characteristic | No medications (n = 5911) | Hypertension medications (n = 824) | P value | Hypotention medications (n = 942) | P value |
|---|---|---|---|---|---|
| Demographics | |||||
| Age, years | 69.6 ± 9.2 | 68.7 ± 9.4 | .011 | 69.7 ± 9.3 | .724 |
| Gender | |||||
| Male | 3529 (59.7) | 502 (60.9) | .503 | 530 (56.3) | .046 |
| Female | 2382 (40.3) | 322 (39.1) | 412 (43.7) | ||
| Race | |||||
| White | 5833 (99.6) | 798 (98.2) | <.001 | 934 (99.7) | .636 |
| Smoking | |||||
| Never | 1193 (20.2) | 146 (17.7) | .002 | 174 (18.5) | .474 |
| Prior | 2976 (50.4) | 386 (46.8) | 481 (51.2) | ||
| Current | 1736 (29.4) | 292 (35.4) | 285 (30.3) | ||
| Medical history | |||||
| Hypertension | 5211 (88.2) | 713 (86.6) | .204 | 837 (88.9) | .546 |
| CAD | 1886 (31.9) | 315 (38.2) | <.001 | 329 (34.9) | .067 |
| CHF | 447 (7.6) | 76 (9.2) | .095 | 81 (8.6) | .268 |
| COPD | 1311 (22.2) | 193 (23.4) | .423 | 238 (25.3) | .036 |
| Diabetes | 1822 (30.8) | 282 (34.2) | .049 | 300 (31.8) | .530 |
| ASA | 5168 (87.4) | 716 (87) | .718 | 812 (86.3) | .324 |
| Clopidogrel | 943 (16) | 165 (20) | .003 | 142 (15.1) | .498 |
| Beta-blockers | |||||
| Chronic >30 days | 3414 (57.8) | 450 (54.6) | .199 | 561 (59.6) | .076 |
| One to 30 days | 1259 (21.3) | 194 (23.5) | 213 (22.6) | ||
| None | 1237 (20.9) | 180 (21.8) | 167 (17.7) | ||
| Symptomatic | 1181 (20) | 171 (20.8) | .607 | 199 (21.1) | .418 |
| Procedure | |||||
| Type of surgery | |||||
| Conventional | 5306 (89.8) | 773 (93.8) | <.001 | 799 (84.9) | <.001 |
| Eversion | 604 (10.2) | 51 (6.2) | 142 (15.1) | ||
| Anesthesia | |||||
| Local/regional | 712 (12) | 102 (12.4) | .783 | 74 (7.9) | <.001 |
| General | 5199 (88) | 722 (87.6) | 868 (92.1) | ||
| Shunt | 2681 (45.4) | 395 (48) | .154 | 418 (44.4) | .574 |
| Patch | 5121 (86.6) | 741 (90) | .006 | 764 (81.1) | <.001 |
ASA, Aspirin; CAD, coronary artery disease; CHF, congestive heart failure; COPD, chronic obstructive pulmonary disease.
Continuous data are presented as mean ± standard deviation and categoric data as number (%).
Compared with normotensive patients, those with postoperative hypertension requiring IVMED were younger, had a higher rate of history of CAD and diabetes, and were more likely to be treated with clopidogrel. In addition, they were more likely to undergo conventional endarterectomy and have a patch placed. There were no differences with respect to a history of hypertension, CHF, beta-blocker treatment, indication of surgery, and type of anesthesia (Table I).
Patients who received IVMED for postoperative hypotension, in comparison with normotensive patients, were more likely to have a history of COPD, undergo conventional endarterectomy, and have general anesthesia. Age, history of hypertension or CAD, beta-blocker treatment, and neurological symptomatic status were similar between groups (Table I).
Outcomes of patients requiring IV medication for postoperative hypertension
Bivariable analysis found that patients with postoperative hypertension requiring IVMED had higher in-hospital mortality compared with those without hemodynamic instability (0.7% vs 0.1%; P < .001). Rates of perioperative MI and CHF were higher in those with postoperative hypertension requiring IVMED (2.4% vs 0.5%; P < .001, and 1.9% vs 0.5%; P < .001, respectively). Ipsilateral stroke (1.5% vs 0.7%; P = .025) and overall stroke rates (1.9% vs 1.0%; P = .018) were also higher in these patients. Finally, patients who required IVMED for postoperative hypertension had longer total hospital LOS than those without hemodynamic instability (2.8 ± 4.7 days vs 1.7 ± 5.5 days; P < .001). There were no differences in 1-year mortality (3.5% vs 2.9%; P = .35) or stroke rates (2.8% vs 2.1%; P = .19; Table II).
Table II.
Postoperative and 1-year outcomes of patients treated with intravenous vasoactive medications (IVMED) for hypertension and hypotension
| Characteristic | No medications (n = 5911) | Hypertension medications (n = 824) | P value | Hypotension medications (n = 942) | P value |
|---|---|---|---|---|---|
| Postoperative outcomes | |||||
| Hospital mortality | 5 (0.1) | 6 (0.7) | <.001 | 8 (0.8) | <.001 |
| MI | 32 (0.5) | 20 (2.4) | <.001 | 25 (2.7) | <.001 |
| CHF | 30 (0.5) | 16 (1.9) | <.001 | 16 (1.7) | <.001 |
| Ipsilateral stroke | 42 (0.7) | 12 (1.5) | .025 | 24 (2.5) | <.001 |
| Contralateral stroke | 20 (0.3) | 4 (0.5) | .507 | 7 (0.7) | .066 |
| Stroke | 60 (1) | 16 (1.9) | .018 | 30 (3.2) | <.001 |
| MI/stroke/death | 92 (1.6) | 36 (4.4) | <.001 | 52 (5.5) | <.001 |
| Hospital LOS, days | 1.7 ± 5.5 | 2.8 ± 4.7 | <.001 | 2.8 ± 5.9 | <.001 |
| One-year outcomes | |||||
| Death | 173 (2.9) | 29 (3.5) | .350 | 48 (5.1) | <.001 |
| Stroke | 123 (2.1) | 23 (2.8) | .190 | 40 (4.2) | <.001 |
| Stroke or death | 291 (4.9) | 49 (5.9) | .209 | 82 (8.7) | <.001 |
CHF, Congestive heart failure; LOS, length of stay; MI, myocardial infarction; SD, standard deviation.
Continuous data are presented as mean ± standard deviation and categoric data as number (%).
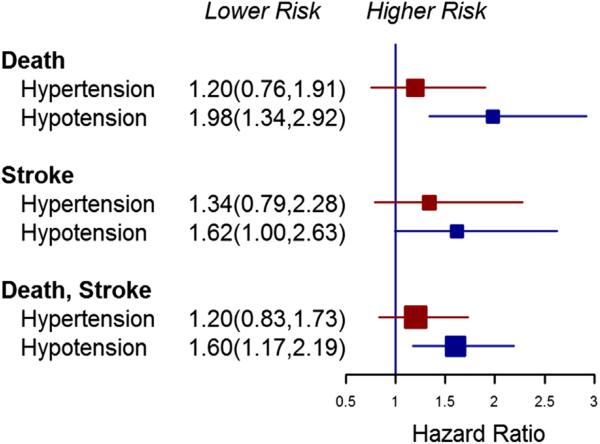
On multivariable analysis, significant postoperative hypertension requiring IVMED following CEA was independently associated with increased risk of postoperative MI (odds ratio [OR], 3.8; 95% confidence interval [CI], 2.0-7.5; P < .001), stroke (OR, 1.9; 95% CI, 1.0-3.6; P = .054), and higher composite MI, stroke, and death rate (OR, 2.6; 95% CI, 1.6-4.1; P < .001). One-year outcomes were however not significantly different for these patients (Figs 1 and 2). Hospital LOS was significantly longer in patients who suffered postoperative hypertension requiring IVMED (means ratio, 1.7; 95% CI, 1.6-1.8; P < .0001).
Fig 1.
Multivariable analysis of the effect of clinically significant post-carotid endarterectomy (CEA) hypertension and hypotension on perioperative outcomes (crude sample). MI, Myocardial infarction.
Fig 2.
Multivariable analysis of the effect of clinically significant post-carotid endarterectomy (CEA) hypertension and hypotension on 1-year outcomes (crude sample).
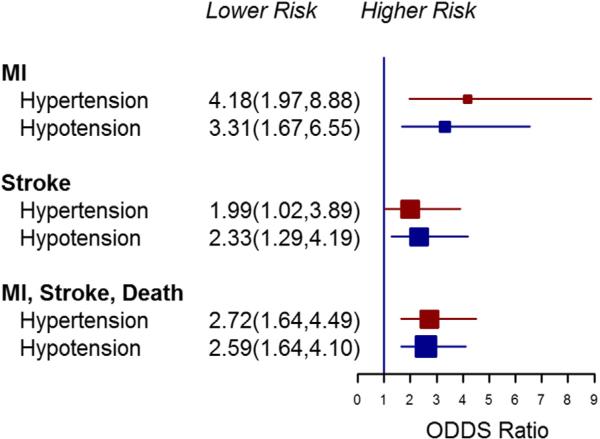
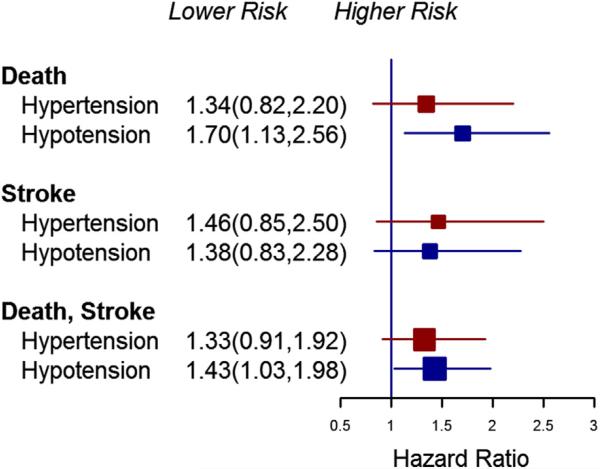
Propensity score matching was used as a secondary risk-adjusted comparison between cohorts of patients treated with IVMED for postoperative hypertension and those without hemodynamic instability. Significant differences noted on bivariable analyses including age, smoking status, CAD, diabetes, type of procedure, and anesthesia type were successfully adjusted (Supplementary Table I, online only). Perioperative mortality, MI, CHF, stroke, and hospital LOS remained significantly higher on bivariable analyses for patients who required IVMED for significant postoperative hypertension (Supplementary Table II, online only). Multivariable analyses of the propensity-matched cohorts confirmed an independent association between significant postoperative hypertension requiring IVMED and perioperative MI, stroke, the composite end point of MI, stroke, or death (Fig 3), and LOS (means ratio, 1.7; 95% CI, 1.6-1.8; Fig 4).
Fig 3.
Multivariable analysis of the effect of clinically significant post-carotid endarterectomy (CEA) hypertension and hypotension on perioperative outcomes (propensity-matched sample). MI, Myocardial infarction.
Fig 4.
Multivariable analysis of the effect of clinically significant post-carotid endarterectomy (CEA) hypertension and hypotension on 1-year outcomes (propensity-matched sample).
Outcomes of patients requiring IV medication for postoperative hypotension
Patients with postoperative hypotension requiring IVMED had higher hospital mortality compared with those without hemodynamic instability (0.8% vs 0.1%; P < .001). Perioperative MI (2.7% vs 0.5%; P < .001) and CHF rates (1.7% vs 0.5%; P < .001) were significantly higher in the hypotension cohort. Ipsilateral stroke (2.5% vs 0.7%; P < .001) and overall stroke rates (3.2% vs 1.0%; P < .001) were also higher in these patients. Hospital LOS was significantly longer in those with IVMED used to treat postoperative hypotension (2.8 ± 5.9 days vs 1.7 ± 5.5 days; P < .001). Lastly, patients with postoperative hypotension requiring IVMED had higher mortality (5.1% vs 2.9%; P < .001) and stroke (4.2% vs 2.1%; P < .001) rates at 1-year follow-up (Table II).
On multivariable analysis, clinically significant postoperative hypotension treated with IVMED was independently associated with increased risk of postoperative MI (OR, 4.3; 95% CI, 2.3-8.2; P < .001), stroke (OR, 2.8; 95% CI, 1.6-4.9; P < .001), and higher composite MI, stroke, or death rate (OR, 3.2; 95% CI, 2.1-5.0; P < .001; Fig 1). Hospital LOS was significantly longer in patients who suffered postoperative hypotension (means ratio, 1.7; 95% CI, 1.6-1.8; P < .0001) requiring IVMED. Significant postoperative hypotension requiring IVMED was also independently associated with death (OR, 2.0; 95% CI, 1.3-2.9; P < .001), stroke (OR, 1.6; 95% CI, 1.0-2.6; P = .052), and stroke or death (OR, 1.6; 95% CI, 1.2-2.2; P = .003) at 1 year (Fig 2).
Similarly significant differences noted on bivariable analyses were successfully adjusted in propensity-matched postoperative hypotension (Supplementary Table I, online only) analyses. Perioperative mortality, MI, CHF, stroke, and hospital LOS were significantly higher on bivariable analyses for patients who required IVMED for significant postoperative hypotension (Supplementary Table II, online only). Multivariable analyses of the propensity-matched cohorts confirmed an independent association between significant postoperative hypotension requiring IVMED with perioperative MI, stroke, the composite end point of MI, stroke, or death (Fig 3), and LOS (means ratio, 1.7; 95% CI, 1.6-1.8) as well as an increased 1-year mortality and stroke (Fig 4).
Factors associated with postoperative hypertension or hypotension requiring IVMED
The following factors were associated with postoperative clinically significant hypertension requiring IVMED; current smoking (OR, 1.3; 95% CI, 1.0-1.7; P = .035), history of CAD (OR, 1.3; 95% CI, 1.0-1.5; P = .022), and clopidogrel (OR, 1.4; 95% CI, 1.1-1.7; P = .006). Eversion endarterectomy (OR, 0.7; 95% CI, 0.5-0.9; P = .007) and use of local or regional anesthesia (OR, 0.5; 95% CI, 0.4-0.8; P < .001) were inversely associated with postoperative clinically significant hypotension requiring IVMED. The area under the ROC curve for the model of factors associated with significant postoperative hypertension was 0.59 (Supplementary Fig, online only). The area under the ROC curve was 0.58 for the model of factors associated with significant postoperative hypotension (Supplementary Fig, online only).
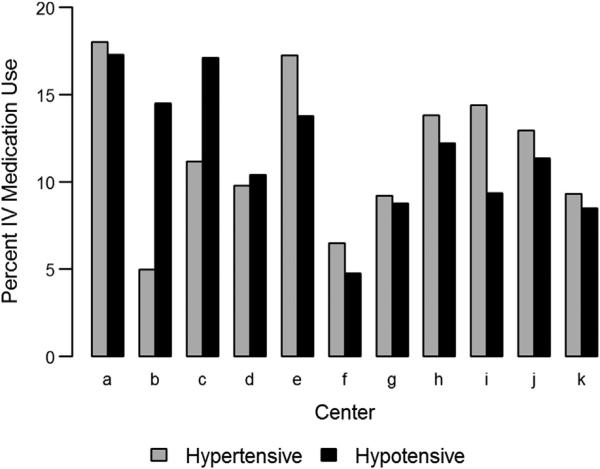
Center variation in the use of IVMED
We examined center variation in the rate of IVMED utilization for treatment of postoperative hypertension or hypotension and noted that the practice pattern varied among centers in New England (P < .001; Fig 5). The overall rate of IVMED use for either postoperative hypertension or hypotension following CEA ranged from 11% to 38%. When center effect was considered in multivariable analyses, the independent association of significant postoperative hypertension or hypotension requiring IVMED on perioperative MI, stroke, and composite MI, stroke, or death remained significant (data not shown).
Fig 5.
Utilization of intravenous vasoactive medications (IVMED) for hypertension or hypotension in centers performing more than 100 carotid endarterectomies (CEAs) per year.
DISCUSSION
Postoperative hypertension and hypotension are well-recognized phenomena after CEA. In this study, up to 27% of CEA patients experienced significant postoperative hypertension or hypotension requiring treatment with IVMED. Patients who required IVMED for postoperative hypertension were younger and more likely to have CAD or diabetes. They had a higher perioperative morbidity and mortality. There was no correlation between postoperative clinically significant hypertension requiring IVMED and 1-year outcomes. Patients who required treatment for postoperative hypotension were more likely to have COPD, undergo conventional endarterectomy, and receive general anesthesia. They suffered increased perioperative morbidity and mortality as well as increased 1-year mortality and stroke rates. Patients with postoperative clinically significant hemodynamic changes requiring treatment with IVMED had significantly longer hospital LOS.
Significant postoperative hypertension was reported in 9% to 56% of patients after CEA.6-8,10,17 The criteria used to define significant postoperative hypertension within these studies varied. Due to the limitation of our dataset, we were not able to determine the exact blood pressure criteria for initiation or discontinuation of vasoactive treatment in our patients. Rather, we classified patients with clinically significant postoperative hypertension as those who required any treatment with IVMED. Given this definition, our rate of postoperative hypertension requiring IVMED was 11%, which is similar to the rate observed by Wong et al (9%) who defined systolic blood pressure greater than 220 mm Hg as significant hypertension.10
Multivariable analysis was used in this study to minimize the effects of potential confounders on postoperative outcomes. To improve the accuracy of the model, factors that were previously found to be significant for development of cardiac complications, stroke, or death using the VSGNE dataset were incorporated into the analysis.15,16 Further risk-adjusted evaluation was performed using propensity score matching to select patients for comparison. Both analyses noted an increased perioperative complication rate in patients with clinically significant postoperative hypertension requiring IVMED treatment. Other studies have also noted higher complication rates, including postoperative neurological deterioration7,18,19 and stroke or death8,10 in patients with postoperative hypertension after CEA. In addition to neurological complications and death, Wong et al noted a nonsignificant statistical association between postoperative hypertension and MI in their study. In contrast, we found that significant hypertension requiring treatment was associated with an up to a threefold increase in the rate of postoperative MI. We believe that ours is the first study to describe increased cardiac complications in patients with clinically significant hypertension after CEA. Although it is not clear whether significant hypertension is a marker or cause of increased perioperative complications following CEA, it appears that this phenomenon does not affect 1-year survival or neurological outcomes.
While postoperative hypotension has been reported in 12% to 40% of CEA,10,11,13 its significance remains unclear.10,13 Some studies have reported increased mortality and MI11 among such patients, while others have claimed postoperative hypotension after CEA to be a transient and benign condition.13 In our study, we defined clinically significant hypotension as the use of IVMED to treat postoperative hypotension. We found that 16% of our CEA cohort had clinically significant postoperative hypotension by this definition, within the range of other reported studies where blood pressure was measured.10,11,13 These patients suffered worse perioperative outcomes including increased risk of MI, stroke, and death. One-year survival was decreased, and 1-year stroke rate was increased. Park et al also reported increased perioperative mortality, MI, and hospital LOS with clinically significant hypotension11 using criteria of >40 mm Hg drop in systolic blood pressure or a systolic blood pressure <90 mm Hg sustained for longer than 1 hour after carotid intervention. We similarly observed longer LOS in patients with clinically significant postoperative hypertension and hypotension.
There are multiple proposed mechanisms for blood pressure fluctuation after CEA. Hypertension or hypotension can occur as a consequence of baroreceptor dysfunction.6,20,21 Hypertension can occur secondary to iatrogenic denervation,20 diminished baroreflex activity,22 or decreased carotid sinus sensitivity.23 Other proposed mechanisms of postoperative hypertension invoke increased production of cerebral renin24,25 or catecholamines.25,26 Sustained hypotension can occur when distortion of baroreceptors in the carotid bulb causes a decrease in sympathetic activity with subsequent peripheral vasodilatation.27
Previous studies have identified certain factors to be associated with significant hemodynamic fluctuation after CEA. Wong et al demonstrated preoperative hypertension, renal insufficiency, neurological instability, and cardiac dysrhythmia to be associated with postoperative hypertension.10 Variables including age more than 65 years old, black race, and intraoperative shunts were also found to be associated with postoperative hypertension following CEA.8,28 Predictors of clinically significant hypotension after carotid intervention included preoperative nitrate use and smoking.11 In our study, factors associated with clinically significant postoperative hypertension requiring IVMED were history of CAD, smoking, and clopidogrel. No association between preoperative hypertension and postoperative hypertension requiring IVMED was found in this study. We also noted association of clopidogrel with postoperative hypertension requiring treatment. The reason for this is unclear; however, a possible explanation is that a higher number of patients with CAD were treated with clopidogrel. Factors identified to be associated with clinically significant postoperative hypotension requiring IVMED were conventional endarterectomy and general anesthesia. Similar to other studies,29,30 we had noted that local regional anesthesia during CEA is less likely to cause postoperative hypotension requiring treatment. The accuracy for these predictive models was fairly poor, judging by area under the ROC curve of less than 0.6. This is an important observation. Our data suggests that preoperative clinical factors are not helpful in predicting which patients are at risk, and therefore, all patients should be closely monitored during the perioperative period following CEA.
A number of operative techniques were suggested to minimize extreme blood pressure fluctuations after CEA including nerve-sparing dissection31 and carotid sinus nerve blockage with local anesthesia.17 Due to the limitation of the VSGNE database, we were not able to assess whether these techniques were used in our patients. A few studies have suggested that eversion endarterectomy increases the risk of post-CEA hypertension.32-34 In our study, eversion endarterectomy was not a factor associated with clinically significant postoperative hypertension requiring IVMED but was associated with a decreased need for treatment for postoperative hypotension when compared with conventional endarterectomy. It is possible that denervation of the carotid bulb during eversion endartectomy may contribute to this finding.35
The threshold for treatment for postoperative blood pressure was variable among the institutions and surgeons participating in the VSGNE, and this likely reflects the true practice patterns in the different centers outside VSGNE. The description of what is considered to be significant hyper- or hypotension after CEA in the literature is also variable,7,8,10,11,13,18,19 and general consensus is lacking. Although we did not find any association of center effect on IVMED utilization and outcomes of these patients, steps can be taken to address these practice variations, which might lead to improvement in the outcomes of these at-risk patients following CEA.
There are a number of important limitations to our study. First, ours is an observational study of a prospectively collected database and is not a randomized controlled trial. Although we attempted to adjust for differences between patients using multivariable analysis of the crude study sample and propensity score matching for risk-adjusted comparisons, there may still be potential confounders that were not accounted for. Second, we did not have information regarding the exact type of IVMED used, the dosage, or timing of infusion. Due to limitation of the dataset, we could not determine the exact method of blood pressure measurement and whether invasive methods were used during each procedure. Another important shortcoming was our inability to determine the specific blood pressure criteria used for initiating and terminating these vasoactive medications. Finally, we cannot determine whether the use of IVMED after CEA caused or resulted from the increased adverse outcomes reported, such as MI, because we do not know the timing of the IVMED with respect to these outcomes.
Despite these limitations, the utility of the VSGNE database has been validated through other studies,16,36,37 and its strength lies in its comprehensive repository of specific variables collected and its regular adjudication process. Using this prospectively maintained database, we were able to evaluate a large cohort of CEA patients and study potential associations of significant hemodynamic changes needing treatment with perioperative and 1-year outcomes.
CONCLUSIONS
Postoperative hypertension and hypotension requiring IVMED are associated with an increased perioperative mortality rate, as well as increased rates of stroke or cardiac complications following CEA. In addition, postoperative hypotension is associated with increased 1-year stroke or death rates. Significant postoperative hemodynamic changes after CEA are also associated with longer hospital LOS. Factors that reliably predict development of significant post-CEA hemodynamic instability were not identified. Although this study is hypothesis-generating, it indicates that the need for IVMED after CEA is not benign, and that such patients deserve careful medical management to potentially avoid significant complications.
Supplementary Material
Footnotes
Author conflict of interest: none.
Presented at the Thirty-seventh Annual Meeting of the Southern Association for Vascular Surgery, Paradise Island, Bahamas, January 23-25, 2013.
Additional material for this article may be found online at www.jvascsurg.org.
The editors and reviewers of this article have no relevant financial relationships to disclose per the JVS policy that requires reviewers to decline review of any manuscript for which they may have a conflict of interest.
AUTHOR CONTRIBUTIONS
Conception and design: TT, ME, JK, RE, PG, JC, AF Analysis and interpretation: TT, ME, JK, RE, GD, PG, JC, AF Data collection: TT, GD Writing the article: TT Critical revision of the article: TT, ME, JK, RE, GD, PG, JC, AF Final approval of the article: TT, AF Statistical analysis: TT, GD, PG, JC, AF Obtained funding: Not applicable Overall responsibility: TT, AF
The authors acknowledge the assistance of Naomi Hamburg, MD, and Denis Rybin, MS, with data analysis and interpretation, as well as with critical revision of the article.
REFERENCES
- 1.North American Symptomatic Carotid Endarterectomy Trial collaborators Beneficial effect of carotid endarterectomy in symptomatic patients with high-grade carotid stenosis. N Engl J Med. 1991;325:445–53. doi: 10.1056/NEJM199108153250701. [DOI] [PubMed] [Google Scholar]
- 2.Barnett HJM, Taylor WD, Eliasziw M, Fox A, Ferguson G, Haynes BR, et al. Benefit of carotid endarterectomy in patients with symptomatic moderate or severe stenosis. N Engl J Med. 1998;339:1415–25. doi: 10.1056/NEJM199811123392002. [DOI] [PubMed] [Google Scholar]
- 3.European Carotid Surgery Trialists’ Collaborative Group Randomised trial of endarterectomy for recently symptomatic carotid stenosis: final results of the MRC European Carotid Surgery Trial (ECST). Lancet. 1998;351:1379–87. [PubMed] [Google Scholar]
- 4.Roubin GS, New G, Iyer SS, Vitek J, Al-Mubarak N, Liu M, et al. Endarterectomy for asymptomatic carotid artery stenosis. JAMA. 1995;273:1421–8. [PubMed] [Google Scholar]
- 5.Halliday A, Mansfield A, Marro J, Peto C, Peto R, Potter J, et al. MRC Asymptomatic Carotid Surgery Trial (ACST) Collaborative Group Prevention of disabling and fatal strokes by successful carotid endarterectomy in patients without recent neurological symptoms: randomized controlled trial. Lancet. 2004;363:1491–502. doi: 10.1016/S0140-6736(04)16146-1. [DOI] [PubMed] [Google Scholar]
- 6.Bove EL, Fry WJ, Gross WS, Stanley JC. Hypotension and hypertension as consequences of baroreceptor dysfunction following carotid endarterectomy. Surgery. 1979;86:633–7. [PubMed] [Google Scholar]
- 7.Lehv MS, Salzman EW, Silen W. Hypertension complicating carotid endarterectomy. Stroke. 1970;1:307–13. doi: 10.1161/01.str.1.5.307. [DOI] [PubMed] [Google Scholar]
- 8.Towne JB, Gernhard VM. The relationship of postoperative hyper-tension to complications following carotid endarterectomy. Surgery. 1980;88:575–80. [PubMed] [Google Scholar]
- 9.Stoneham MD, Thompson JP. Arterial pressure management and carotid endarterectomy. Br J Anaesth. 2009;102:442–52. doi: 10.1093/bja/aep012. [DOI] [PubMed] [Google Scholar]
- 10.Wong JH, Findlay JM, Suarez-Almazor ME. Hemodynamic instability after carotid endarterectomy: risk factors and associations with operative complications. Neurosurgery. 1997;41:35–41. doi: 10.1097/00006123-199707000-00009. discussion: 41-3. [DOI] [PubMed] [Google Scholar]
- 11.Park BD, Divinagracia T, Madej O, McPhelimy C, Piccirillo B, Dahn MS, et al. Predictors of clinically significant postprocedure hypotension after carotid endarterectomy and carotid angioplasty and stenting. J Vasc Surg. 2009;50:526–33. doi: 10.1016/j.jvs.2009.05.005. [DOI] [PubMed] [Google Scholar]
- 12.Ross SD, Tribble CG, Parrino PE, Shockey KS, Kerin JA, Kron IL. Intensive care is cost-effective in carotid endarterectomy. Cardiovasc Surg. 2000;8:41–6. doi: 10.1016/s0967-2109(99)00081-2. [DOI] [PubMed] [Google Scholar]
- 13.Gibbs BF. Temporary hypotension following endarterectomy for severe carotid stenosis: should we treat it? Vasc Endovasc Surg. 2003;37:33–8. doi: 10.1177/153857440303700105. [DOI] [PubMed] [Google Scholar]
- 14.Cronenwett JL, Liksoky DS, Russell MT, Eldrup-Jorgensen J, Stanley AC, Nolan BW. VSGNNE. A regional registry for quality assurance and improvement: the Vascular Study Group of Northern New England (VSGNNE). J Vasc Surg. 2007;46:1093–102. doi: 10.1016/j.jvs.2007.08.012. [DOI] [PubMed] [Google Scholar]
- 15.Bertges DJ, Goodney PP, Zhao YY, Schanzer A, Nolan BW, Likosky DS, et al. Vascular Study Group of New England. The Vascular Study Group of New England Cardiac Risk Index (VSGCRI) predicts cardiac complications more accurately than the Revised Cardiac Risk Index in vascular surgery patients. J Vasc Surg. 2010;52:674–83. doi: 10.1016/j.jvs.2010.03.031. [DOI] [PubMed] [Google Scholar]
- 16.Goodney PP, Likosky DS, Cronenwell JL. Vascular Study Group of Northern New England. Factors associated with stroke or death aftger carotid endarterectomy in Northern New England. J Vasc Surg. 2008;48:1139–45. doi: 10.1016/j.jvs.2008.05.013. [DOI] [PubMed] [Google Scholar]
- 17.Tang TY, Walsh SR, Gillard JH, Varty K, Boyle JR, Gaunt ME. Carotid sinus nerve blockade to reduce blood pressure instability following carotid endarterectomy: a systemic review and meta-analysis. Eur J Vasc Surg. 2007;34:304–11. doi: 10.1016/j.ejvs.2007.02.024. [DOI] [PubMed] [Google Scholar]
- 18.Asiddao CB, Donegan JH, Whitesell RC, Kalbfieisch JH. Factors associated with perioperative complications during carotid endarterectomy. Anesth Analg. 1982;61:631–7. [PubMed] [Google Scholar]
- 19.Hans SS, Glower JL. The relationship of cardiac and neurological complications to blood pressure changes following carotid endarterectomy. Am Surg. 1995;61:356–9. [PubMed] [Google Scholar]
- 20.Sigaudo-Roussel D, Evans DH, Naylor AR, Panerai RB, London NL, Bell P, et al. Deterioration in carotid baroreflex during carotid endarterectomy. J Vasc Surg. 2002;36:793–8. [PubMed] [Google Scholar]
- 21.Tarlov E, Schmidek H, Scott M, Wepsic JG, Ojeman RG. Reflex hypotension following carotid endarterectomy: mechanism and management. J Neurosurg. 1973;39:323–7. doi: 10.3171/jns.1973.39.3.0323. [DOI] [PubMed] [Google Scholar]
- 22.Nouraei SA, Al-Rawi PG, Sigaudo-Roussel D, Giussani DA, Gaunt ME. Carotid endarterectomy impairs blood pressure homeostasis by reducing physiologic baroreflex reserve. J Vasc Surg. 2005;41:631–7. doi: 10.1016/j.jvs.2005.01.009. [DOI] [PubMed] [Google Scholar]
- 23.Appenzeller O, Descarries L. Circulatory reflexes in patients with cerebrovascular disease. N Eng J Med. 1964;271:820–3. doi: 10.1056/NEJM196410152711604. [DOI] [PubMed] [Google Scholar]
- 24.Smith BL. Hypertension following carotid endarterectomy: the role of cerebral renin production. J Vasc Surg. 1984;1:623–7. [PubMed] [Google Scholar]
- 25.Hans SS, Prakash S, Hans P, Glover JL. The role of renin and catecholamine production in postcarotid endarterectomy hypertension. Surg Gunecol Obstet. 1992;174:201–4. [PubMed] [Google Scholar]
- 26.Ahn SS, Marcus DR, Moore WS. Post-carotid endarterectomy hyper-tension: association with elevated cranial norepinephrine. J Vasc Surg. 1989;9:351–60. doi: 10.1067/mva.1989.vs0090351. [DOI] [PubMed] [Google Scholar]
- 27.Fardo DJ, Hankins WT, Houskamp W, Robson L. The hemodynamic effects of local anesthestic injection into the carotid body during carotid endarterectomy. Am Surg. 1999;65:648–51. [PubMed] [Google Scholar]
- 28.Benzel EC, Hoppens KD. Factors associated with postoperative hypertension complicating carotid endarterectomy. Acta Neurochir (Wien) 1991;112:8–12. doi: 10.1007/BF01402447. [DOI] [PubMed] [Google Scholar]
- 29.Rerkasem K, Rothwell PM. Local versus general anesthesia for carotid endarterectomy. Cochrane Database Syst Rev. 2008;4:CD000126. doi: 10.1002/14651858.CD000126.pub3. [DOI] [PubMed] [Google Scholar]
- 30.GALA Trial Collaborative Group General anaesthesia versus local anaesthesia for carotid surgery (GALA): a multicenter, randomized controlled trial. Lancet. 2008;372:2132–42. doi: 10.1016/S0140-6736(08)61699-2. [DOI] [PubMed] [Google Scholar]
- 31.Cafferata HT, Merchant RF, DePalma RG. Avoidance of postcarotid endarterectomy hypertension. Ann Surg. 1982;4:465–71. doi: 10.1097/00000658-198210000-00010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mehta M, Rahmani O, Dietzek AM, Mecenas J, Scher LA, Friedman SG, et al. Eversion technique increased the risk for post-carotid endarterectomy hypertension. J Vasc Surg. 2001;34:839–45. doi: 10.1067/mva.2001.118817. [DOI] [PubMed] [Google Scholar]
- 33.Demirel S, Attigah N, Bruijnen H, Hakimi M, Macek L, Böckler D. Eversion carotid endarterectomy is associated with impaired postoperative hemodynamic stability compared with the conventional technique. Ann Vasc Surg. 2012;26:755–65. doi: 10.1016/j.avsg.2011.12.015. [DOI] [PubMed] [Google Scholar]
- 34.Demirel S, Bruijnen H, Attigah N, Hakimi M, Böckler D. The effect of eversion and conventional-patch technique in carotid surgery on postoperative hypertension. J Vasc Surg. 2011;54:80–6. doi: 10.1016/j.jvs.2010.11.106. [DOI] [PubMed] [Google Scholar]
- 35.Demirel S, Macek L, Bruijnen H, Kakimi M, Böckler D, Attigah N. Eversion carotid endarterectomy is associated with decreased baroreceptor sensitivity compared to conventional technique. Eur J Vasc Endovasc Surg. 2012;44:1–8. doi: 10.1016/j.ejvs.2012.04.009. [DOI] [PubMed] [Google Scholar]
- 36.Stone DH, Nolan BW, Schanzer A, Goodney PP, Cambria RA, Likosky DS, et al. the Vascular Study Group of Northern New England Protamine reduces bleeding complications associated with carotid endarterectomy without increasing the risk of stroke. J Vasc Surg. 2010;51:559–64. doi: 10.1016/j.jvs.2009.10.078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Farber A, Tan TW, Rybin D, Kalish JA, Hamburg NM, Doros G, et al. Vascular Study Group of New England Intraoperative use of dextran is associated with cardiac complications after carotid endarterectomy. J Vasc Surg. 2013;57:635–41. doi: 10.1016/j.jvs.2012.09.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.