Abstract
Access to nutritious foods is limited in disenfranchised communities in the United States. Policies are beginning to focus on improving nutritious food access in these contexts; yet, few theories are available to guide this work. We developed a conceptual model of nutritious food access based on the qualitative responses of food consumers in 2 different regions of the American South. Five domains (economic, service delivery, spatial–temporal, social, and personal) and related dimensions of nutritious food access were identified. The conceptual model provides practical guidance to researchers, policy makers, and practitioners working to improve nutritious food access in communities.
Keywords: Food security, community practice, community development, food insecurity, social justice, social policy
INTRODUCTION
Health is produced by a range of determinants ranging from biological and genetic pathways to social conditions and policies (Warnecke et al., 2008). Social determinants of health frameworks draw attention to the interplay among many factors that produce health, in general, and health disparities, in particular, including biological characteristics; individual behaviors; social and community networks; living and working conditions; and socioeconomic, cultural, and environmental conditions (Evans, Barer, & Marmor, 1994; Kindig & Stoddart, 2003; Szreter, 2003; Whitehead & Dahlgren, 1991). Increasingly, these frameworks are shifting the focus of health research and practice to include community-level, in addition to individual-level, interventions (Story, Kaphingst, Robinson-O’Brien, & Glanz, 2008). Interestingly, this movement upstream has been driven by researchers and practitioners from public health, with social workers less engaged in discourse and action within this burgeoning field (Bywaters, 2009).
The social production of health disparities is evident in obesity trends in the United States. Obesity and overweight are defined by the World Health Organization as “abnormal or excessive fat accumulation that may impair health” (World Health Organization, 2013). Obesity is an important health issue because of its relationship with physical health (e.g., diabetes, cancer, heart disease) and mental health (e.g., depression) conditions (e.g., Calle, & Thun, 2004; Hu et al., 2001; McElroy et al., 2004). Moreover, although obesity rates are high and rising in the United States, affecting approximately one in three individuals (Flegal, Carroll, Ogden, & Curtin, 2010; Ogden, Carroll, Curtin, Lamb, & Flegal, 2010), trends are even higher among marginalized populations, including people of color and people with low income (Pan et al., 2009; Wang & Beydoun, 2007). African Americans in the United States have the highest prevalence of obesity (Wang & Beydoun, 2007). The association between socioeconomic status and obesity reveals that people in the highest income categories have lower rates of obesity; however, this relationship is more complex when intersections of race and class are further explored (Wang & Beydoun, 2007).
Another way to examine the social nature of obesity is to explore its relationship with food insecurity and hunger (Franklin et al., 2012). In other words, to explore how excessive body weight is associated with having “limited or uncertain availability of nutritionally adequate and safe foods or limited or uncertain ability to acquire acceptable foods in socially acceptable ways” (National Research Council, 2005, p. 23). Food insecurity is a household-level factor that may result in hunger among individuals. Hunger is defined as “the uneasy or painful sensation caused by a lack of food” (National Research Council, 2005, p. 23). The United States measures food insecurity among households on an annual basis, but does not systematically measure hunger. In 2011, about 15% of U.S. households were food insecure, with higher rates for African American (25%) and Hispanic (26%) households and low-income households (35%; Coleman-Jensen, Nord, Andrews, & Carlson, 2012). A number of studies have found that the odds of being obese or overweight rises with increasing food insecurity, particularly for women (Franklin et al., 2012).
The relationship between obesity and food insecurity has resulted in a new line of research that situates these experiences within community contexts, and looks to community-level solutions for addressing these problems. In 2008, the U.S. Congress commissioned a study to identify “food deserts,” defined as an “area in the United States with limited access to affordable and nutritious food, particularly such an area composed of predominantly lower income neighborhoods and communities” (US Department of Agriculture, 2009, p. 1). Although food insecurity was an interest of the Congress-commissioned study, it was specifically designed to examine how “the relative lack of access to full-service grocery stores and the easier access to fast and convenience foods may be linked to poor diets, and ultimately, to obesity and other diet-related diseases” (US Department of Agricuture, 2009, p. 1, emphasis added). In this Congress-commissioned analysis, nutritious food was defined as fruits, vegetables, whole grains, fat-free or low-fat dairy products, and lean meats, as well as nutrient-dense foods and beverages encouraged in dietary guidelines to promote healthy weight and overall health (US Department of Agricuture, 2010, 2012). This resulted in the identification of 6,529 food desert Census tracts that meet criteria for both low levels of household income and low access to supermarkets or larger grocers (Dutko, Ver Ploeg, & Farrigan, 2012). Census tracts were considered low income if they had either a poverty rate of at least 20% or a median household income that was 80% or less of the metropolitan area’s median family income (for tracts in metropolitan areas) or the statewide median family income (for tracts in nonmetropolitan areas; Dutko et al., 2012). Census tracts were considered low access if at least 500 people and/or 33% of the Census tract population lived one mile or more from a supermarket or large grocery in urban areas and more than 10 miles in rural areas (Dutko et al., 2012). Based on these definitions, 38.3% of all Census tracts in the United States were defined as low income; among these 26.2% also were low-access areas; more food deserts were found in Census tracts in rural (33.8%) versus urban (23.3%) areas (Dutko et al., 2012). Factors associated with food desert Census tracts included concentration of poverty and percent minority population (Dutko et al., 2012).
The systematic identification of food deserts throughout the United States provided evidence that disparities in nutritious food access exist, which fueled recommendations to transform communities to improve access to healthy foods (Khan et al., 2009). This process of community transformation has emphasized establishing or enhancing food retail outlets in communities (Centers for Disease Control and Prevention, 2009; US Department of Health and Human Services, 2010; White House, 2010), a logical response to food desert analyses that identified geographic areas with limited physical access to food stores. Moreover, a focus on increasing physical access to food retail outlets is influenced by the growing field of spatial epidemiology that utilizes geographic information systems to examine food environments and public health (e.g., Liese, Weis, Pluto, Smith, & Lawson, 2007; Moore & Diez Roux, 2006; Morland, Wing, Diez Roux, & Poole, 2002). Yet, recent evidence reveals that people may not be shopping at food stores closest to their home (Drewnowski, Aggarwal, Hurvitz, Monsivais, & Moudon, 2012; Liese, Blake, Bell, Barnes, & Freedman, 2012). Interestingly, an intervention in the United Kingdom involving the development of a supermarket in a food desert resulted in less than half of nearby residents switching to the new store as their “main store” (Wrigley, Warm, & Margetts, 2003). In Columbia, South Carolina, a grocery store was established in a food desert adjacent to a public housing community (Phillips, 2008), but it closed after 1.5 years because of lack of revenue and low usage by nearby residents.
These findings raise questions about nonspatial characteristics influencing nutritious food access. Although there is empirical evidence suggesting that nutritious food access is also related to affordability (e.g., Chung & Myers, 1999; Giskes, Van Lenthe, Brug, Mackenbach, & Turrell, 2007; Morland et al., 2002; Baker, Schootman, Barnidge, & Kelly, 2006) and quality (e.g., Blitstein, Snider, & Evans, 2012; Block & Kouba, 2006; Hendrickson, Smith, & Eikenberry, 2006; Zenk et al., 2006), there is not a unifying conceptual model that outlines the range of factors associated with nutritious food access (Story et al., 2009). The “absence of clear, testable conceptual models” of nutritious food access has been defined as the most important methodological issue related to research on food environments (Oakes, Masse, & Messer, 2009, p. S177). Establishing a conceptual model of nutritious food access is not only important for research, but also for policy and practice. From a research perspective, a conceptual model of nutritious food access would provide guidance to more accurately define and measure relationships between factors related to access to identify the most salient for different populations. Moreover, a model of nutritious food access would provide guidance to policymakers and practitioners as programs are being developed to most effectively increase access to healthy foods in communities.
Our aim in this study was to address this gap by developing a conceptual model of nutritious food access based on the qualitative responses of food consumers in two different regions of the American South. This geographic area was selected because obesity (Pan et al., 2009) and food insecurity (Coleman-Jensen et al., 2012) are higher in these regions. Identifying factors associated with nutritious food access in this region is particularly important for addressing health disparities and promoting health equity. We focused this analysis on access to nutritious foods to align our model with the definition of a food desert purported by the US Department of Agriculture, which emphasizes access to nutritious foods (i.e., fruits, vegetables, whole grains, lean meats) needed to promote healthy weight and overall health (US Department of Agricuture, 2010, 2012).
METHOD
This study was approved by two university review boards. Informed consent was obtained from all study participants. Two sources of qualitative data, in-depth interviews and focus groups, inform the analysis.
Data Collection
In-depth interviews
In-depth interviews were conducted with 17 individuals. The source population for the interviews included adults shopping at youth-center-based farmers’ markets established in low-income communities in Nashville, Tennessee (Freedman, Bell, & Collins, 2011). Purposeful and maximum variation sampling was used to select different types of interviewees (e.g., race, gender, age) (Glaser & Strauss, 1967; Miles & Huberman, 1994; Weiss, 1994). This facilitated representativeness in the data analysis process (Miles & Huberman, 1994). The interviews continued until responses became redundant (Glaser & Strauss, 1967). Recruitment took place at the farmers’ markets through posters and oral communication that described the purpose of the interviews, time commitment, and compensation ($20).
Most interviewees identified as Black/African American (88%), female (71%), and had an annual household income of $39,999 or less (59%). Interviews were conducted June–August 2007. Each participant was interviewed once; interviews lasted between 45 min and 2.5 hr and were conducted by the lead author. Interviews were semistructured, open-ended, one-on-one, and focused on eliciting participants’ perspectives on the relationship between social factors and access to healthy foods (see Freedman, 2009, for questions). All interviews were tape-recorded for transcription. The interview guide was a dynamic document, and new questions were added to the guide as new themes emerged (Weiss, 1994).
Focus groups
Forty-one participants took part in six focus groups (Range = 5–10 participants per group). The source population for the focus groups included adults in rural and urban counties in South Carolina. Purposeful and maximum variation sampling was used to select different types of focus group recruitment sites (e.g., sites serving low v. middle to high income, geographic location; Glaser & Strauss, 1967; Miles & Huberman, 1994; Weiss, 1994). Recruitment of focus group participants occurred at six health centers and one private K–12 school. The school was added to target participants representing higher income strata. Recruitment occurred through posters at the sites describing the purpose of the research, time commitment, and compensation ($40). Food was provided at each focus group.
Most participants identified as Black/African American (59%) or White (37%), female (68%), and had an annual household income of $39,999 or less (56%). The focus groups were conducted November 2009–Feburary 2010, lasted 2 hr, and were facilitated by two trained assistants. All focus groups were tape-recorded for transcription. A semistructured facilitation guide was used to assess food shopping patterns (e.g., How often do you go food shopping?, Do you regularly travel a longer distance to go to specific food stores?), perceptions of the local food environment (e.g., Would you like to see more or different food stores in your community, why or why not?), and factors that made it easier or more difficult to access healthy foods in the community (e.g., describe other places where it was easier or more difficult for you to do your food shopping).
Analysis
A grounded theory approach to analysis was employed (Charmaz, 2001). It began with the development of a codebook based on inductive and iterative analysis of the interview data. Next, three independent coders applied the codebook to a focus group transcript selected at random. This stage of the analytic process included an initial read of the transcript to become exposed to the ideas and concepts and subsequent line-by-line reads to identify text that fit the preliminary codes as well as those that informed the creation of new codes (Charmaz, 2001). Following this review, the team compared their coding patterns and modified the codebook. This same process was then applied to a randomly selected interview transcript. Then, 10 of the transcripts were coded by two independent reviewers to determine the percent agreement in coding practices yielding an agreement rate of 80% or higher for all but two transcripts, which were further discussed until agreement was achieved. The remaining transcripts were coded by one reviewer but were discussed by the entire research team to review coding patterns. The qualitative data analysis software ATLAS.ti was used to manage and organize coding (Scientific Software Development, 2011).
FINDINGS
Results of the inductive analysis reveal five domains and related dimensions of nutritious food access that are summarized in Table 1. Each domain with supporting qualitative text is described in the following.
TABLE 1.
Domains, Dimensions, Definitions, and Example Quotations for Emergent Theory of Nutritious Food Access
| Domain | Dimension | Definition | Example Quotation |
|---|---|---|---|
| Economic access | Household finances | Financial resources of the household available for food purchases | You try and get as much quality as you can or get as much food as you can for the dollar that you have. |
| Food costs | Cost of nutritious foodstuff | There’s things that I would like to try that are healthier. And it’s a little bit more expensive. I’ve found out everything that is healthier for you, cost more. | |
| Store incentives | Coupon or other incentive programs at store | I don’t get food stamps, like a lot of people, and when you have to go in the store and spend cash money you have to figure out how to get the best deal for your money. And then be able to eat good meals, you know what I’m saying, well-balanced meals. So I just go through the papers and find my sales that I like, buy the foods that we like and that’s what I do. And I go through my Sunday paper and clip all the coupons. Lord have mercy, you’d be surprised how much you save with a coupon. | |
| Value | Perception of whether food in store is worth the price | I go to two different stores in that same day. I like [budget grocer] because their can goods are cheap. I love going there ‘cuz their can goods are cheap and their salad dressings and some of their frozen foods are cheap there. And I go to the bigger grocery store—if I can’t make the meat market—for my meats and my fresh vegetables. | |
| Service delivery | Foods sold | Quality and variety of items sold in stores | Ah, so I mean, it’s the quality of what [food] you’re trying to get. You know, as a shopper I always want quality for what I’m spending and product quality to me is the most important thing. I’ll drive farther to save some money but I’d also drive even farther out of my way if the quality of something in one place is not as good. |
| Staff and service | Timeliness, helpfulness, and respectfulness of food service personnel | So many times at [name of grocery store] you come in and there’s a lot of people in the store but you might have only one register [opened]. And so then you come in and try to get in and out … and then you’re sitting there stuck because they don’t have enough people [working]. | |
| Presentation | General organization and layout of a store and customer base | If you feel like you have plenty [of store options], you go where you like the store … where you like what the people look like. And you know, nobody’s looking shady. … You’re not worried about anything, or at least you think you’re safe. | |
| Spatial-temporal access | Boundaries of local food environment | Subjectively determined; area around one’s home regardless of geographic boundaries | If you’re living in a city or in a community it’s a little better definition to it [neighborhood] than if you are living in a rural area. |
| Balanced access | Diversity of food stores available in the local food environment | Balanced: Where I live is very convenient to everything so I live in a great part so there is a [name of warehouse food store] on one side, then on the other side there are grocery stores which are [name of chain supermarket] and [name of organic market]. Imbalanced: Where I live they got a couple little small stores, which I wouldn’t buy dog food from. ‘Cause it would be outdated. |
|
| Travel time | Time to travel to food stores and access to reliable transport | All those little stores is kind of like in a cluster so I’m really not burning up a lot of gas to go from store to store because the stores that I pick, they’ll be all in that same vicinity. | |
| Time costs | Time resources of the household available for food-related activities | Usually I go one place [name of chain grocer]. I know where everything at, so it doesn’t take me long to get what I need and get out. | |
| Social access | Culture | Family, racial, and ethnic foodways and traditions influencing food access | I think that a lot of times, as a race we [African Americans] are afraid to make changes because we don’t want to appear trying to be White or we’re trying to eat White. But when there is an understanding of that African people throughout the diaspora ate the kinds of foods that they ate, then it frees people up to make different choices and understand that they’re really not eating White; they’re eating the way they originally ate. |
| Discrimination | Differential access to foods based on race, class, geographic location, or gender | I don’t want to go with a “race card” but just say, for instance, if I went to [name of chain grocery store] in [minority community], some items there, I would not find. I’m not saying that that store is dirty, but it’s a lot of stuff there that I may go there to look for but I would not find. If I went to [name of same chain grocery store] in [majority White community] … whatever they have advertised in that paper, their cuts of meats are much fresher. They do their meats like daily. You understand what I’m saying? And they pull these items out of the counter if they don’t sell them that day. These items get pulled in the [majority White] store. In the [minority community], they may stay there a couple of days and then they’ll put a ticket on there and say, “We’ve reduced this by a dollar in order to sell that item.” | |
| Relationships | Connections to growers, food service personnel, and/or other customers in food outlets. | I go different places to shop. Sometimes I just go with my people just to be going and then I’ll come back and I might get it or might not get it. | |
| Personal Access | Health status | Aspects of individual and family health or disease that influence food access | I’m on a fixed income, so it’s kinda hard for me sometimes. You know, I have to go that far to get food because I have health problems and I have to eat certain foods. You know, it’s not by my choice that I have to do this. And it’s more expensive and when you’re paying your money, you kinda want the best. Good quality. Freshness. And it’s hard to find. |
| Food and nutrition knowledge | What people know or believe to be true and important about food and eating | I know all this but it still doesn’t change the fact that, because I was in a survival mode, that I ate a lot of canned goods, even though I knew they were high in sodium. I ate a lot of pork, even though I knew that it leads to high blood pressure and, you know, I mean, I was eating a lot of things that I knew were not good for me. I would drink a ton of Kool-Aid. … I still drink Kool-Aid, … I’m struggling to get rid of that one, but, ah, I know all that stuff and I know that it’s not good for you. | |
| Food-related identities and preferences | How a person identifies themselves as an eater or shopper and how personal and family members preferences influence food access. | I feel like I’m a healthier eater than the rest of my family so I influence—because I cook—them being healthy and not knowing it. You know, the turkey or the, I only buy the 93% lean meat. If we do have meat. Like our hamburger. I try to buy the healthiest and I guess I consider you know, really, if my kids, we all want, we probably eat cheeseburgers once every week or two. I still think if I buy the Orida French fries and make 93% lean burgers. That’s so much healthier than going to a restaurant and getting the same thing; you know what I mean. We try, we eat in a lot. We don’t eat out. We eat out probably once a week for a main week. Maybe once a week for lunch and once a week for dinner. So I do cook, like I said, it’s just more of the shortcut ways of eating healthy I guess. |
Economic Access
Economic access included four dimensions: (a) household finances, (b) food costs, (c) store incentive programs, and (d) perceived value of foods in stores.
Household finances
Household finances referred to the financial resources of a household available for food purchases (i.e., funds leftover after paying rent, childcare). Most participants indicated that being on a limited or fixed income constrains access to nutritious foods, which was frequently underscored through statements such as, “When my Food Stamps are gone, that’s it,” or “You try and get as much quality as you can or get as much food as you can for the dollar that you have.” Participants frequently reported cutting back on the purchase of nutritious food products due to financial constraints.
Food costs
Food costs referred to the perceived costs of nutritious foods. There was consensus among the participants that nutritious foodstuff is expensive; it was often described as being “totally priced out of the ballpark.” In particular, fresh fruits and vegetables, lean meats, and whole grain products were considered to be some of the most expensive items in food stores, as the following interviewee highlights: “I have good access to fresh and healthy foods, but it’s not always affordable. I can’t always get what I really want.” Although food stores that sell nutritious products may be geographically near, economic barriers may increase the distance to these stores.
Store incentives
Store incentives referred to coupon or other incentive programs available at food stores. Participants indicated that many stores advertise sales in a weekly paper or flyer; however, some promotions were revealed when a customer entered a store (e.g., bargain bins). Although most participants reported an awareness of incentive programs, their influence on shopping patterns varied. Some reported that they occasionally take advantage of incentives such as “buy 1 get 1 free” or “5 cans for a dollar” during a shopping trip. Bargain shoppers used incentives to make cost comparisons and find the best deals; coupon shoppers” planned their entire shopping routines and meals around sales and incentives. Incentive programs were identified as a method for addressing other economic barriers (e.g., household finances, food costs) to accessing nutritious foods.
Value
Value was defined as the perception of whether the foods available in a store were worth the price. Participants indicated a general awareness of a “good value” for certain food items and reported a willingness to travel farther to frequent stores selling foods at better prices. Value was related to the price of the food as well as the quality.
Service Delivery
Service delivery was related to various aspects of food stores and included three dimensions: (a) quality and variety of foods sold, (b) staff and service, and (c) presentation.
Foods sold
Foods sold referred to the quality and variety of items sold in stores and included both positive (e.g., high quality, good variety), as well as negative attributions (e.g., poor quality, lack of variety). The quality of foods sold in a store was often described as being more important than the spatial convenience and economic access of the store. Many respondents reported traveling long distances (up to 90 miles) to access high quality food—particularly meats and produce—at specialty grocers, meat markets, and farmers’ markets as the following focus group quotation highlights:
I don’t like shopping at the one [grocery store] that’s a little close to me because the meat is never fresh. It seems like it keeps constantly being washed and repacked and I don’t like that so I’d rather drive across town to the meat market before I buy food from my grocery store.
Participants reported that they regularly examined expiration dates, dents in cans, and mold or decay on food to weed out poor quality foods, as well as “meat marbling” and the “crispiness of [lettuce] leaves” to identify high quality foods. There was agreement among participants that “freshness” was paramount to determining the quality of foods sold, and ultimately, food store selection. A few participants planned their shopping trips to coincide with the date of delivery of foods to their store. Many participants reported that locally or home-grown foods were the freshest products available; these were described as tasting better than their nonlocal counterparts. Locally grown foods were also described as being safer to eat and less “scary” (i.e., fewer pesticides and antibiotics) than imported products, as the following interviewee highlights: “If I know it’s local, and it’s grown local, then I’m really confident that it’s good, good for me, and it, you know, later on, I won’t hear something that, you know, I shouldn’t have eaten that.”
The variety of foods sold in a store also was identified as a key feature of access. Many respondents indicated that they preferred shopping at a discount superstore or dollar variety stores because they facilitated “one-stop shopping” with “everything centralized” in one store, as the following focus group quote highlights:
I go to [discount superstore] more frequently because of the convenience. If I need to pick up some supplies for my computer, while I’m in the store, [discount superstore] has it. And some of the clothes, I might also pick up some socks or some underwear.
Another respondent stated, “I hate going to multiple stores. I like to go to one store, get everything I need and go home. If I have to go here, there, and everywhere, to me, that is not a great savings.” Specialty products such as choice cut meats, breads, herbs and spices, and ethnic, organic, gourmet, or health foods were described as food types that influenced food store selection: “My husband’s Latino, so we’ll go over to [other side of town] to get Latin food sometimes, because it’s not carried in major stores.”
Staff and service
Staff and service referred to the timeliness, helpfulness, and respectfulness of food store personnel. Many respondents highlighted the importance of having the right number of staff members available to assist customers. Participants reported that having very few staff members onsite often delayed store visits. Additionally, it was important to have knowledgeable staff members willing and capable of locating products, directing customers, and/or assisting with bagging and transporting groceries. Respondents who were elderly and parents with young children, in particular, mentioned the importance of customer service at food stores:
You might go to [name of chain grocery store] because you know they’re going to help you out with your groceries and treat you well whereas you might not go to the [name of another chain grocery store] that day cause you are going to get no help if you have your kids.
It was also important to have respectful staff members, as the following focus group quotation highlights: “I do not want to spend my money where people are being rude and mean to me.”
Presentation
Presentation referred to the general organization and layout of a store, as well as the customer base. There was a desire for stores that were neat and organized:
I walk into a couple of places [food stores] and it’s like things are thrown around. Things are in the aisle. … You gotta go over here to get one part of what I want, over here to get the other part of what I want. I don’t want to deal with that. If it’s [food store] not organized, I don’t care about it. I lose interest very quickly.
Participants reported that sensory cues such as smell and sight could be used to judge the quality of the food store. In particular, sensory cues triggered by the meat and produce departments were identified as key indicators of quality. Cleanliness was also described as influencing nutritious food access. It was important that the store, as well as the food products, were perceived to be clean, as the following focus group quote highlights: “I look at dust. I look at the overall store or what it looks like and if the whole thing doesn’t look right, that affects me.” Participants also reported a desire for having foods properly placed on the shelves and described cluttered or disorganized food stores as “second class.” Respondents were aware of store remodeling efforts; these efforts positively influenced perceptions of food stores. Additionally, parking options were described as important attributes of the store:
Sometimes parking can really make a difference. You just ride around and around. You can’t find a space and sometimes I’ll get aggravated and go right up the street to [name of another grocery store] cause that’s easy parking space.
Store presentation also included references to perceptions of the customer base. Respondents indicated that they paid attention to the other shoppers in the store and preferred stores with customers that appeared respectful, clean, and neat.
Spatial–temporal Access
The spatial domain included four dimensions: (a) boundaries of local food environments, (b) balanced access to food stores, (c) travel time, and (d) time costs.
Boundaries of local food environments
In this article, we use the term local food environment to define spatial access, because the terms neighborhood and community had different and nebulous meanings for the participants. For instance, when asked to define their neighborhood environment, spatial definitions included distances as short as less than one mile around the home to greater than 30 miles. The concept of neighborhood was less salient for participants from rural areas. In this analysis, local food environment is subjectively determined and refers to the area around one’s home regardless of geographic boundaries.
Balanced access
Balanced access refers to the diversity of food stores available in the local food environment. Local food environments were considered more balanced if they had a mixture of store types (e.g., grocery store, convenience store, dollar store) and less balanced if there was an over-abundance of convenience stores and no access to a larger grocer selling a variety of foods.
Participants living in self-identified balanced food environments were generally satisfied with their food environment: “I go to everything within a mile. Like I said, I pretty much live right here, so, things are within a mile” and “I like to go to [name of chain grocer], and I don’t find myself having to go to three or four different stores just to find what I need. They’ve pretty much got everything centralized right there.” Participants representing the highest income strata reported the most balanced access to food stores in their local food environment.
In general, participants with low levels of income and those from rural areas reported that their local food environment was not balanced because it did not have a full-service grocer. Smaller food stores, convenience stores, and fast food restaurants were identified in the local food environment; however, these stores were not considered suitable for regular food shopping, even if they were used to pick up a few items now and then. An interviewee living in a public housing complex in an urban area described her local food store by stating that it sold “canned goods and cold drinks. They ain’t got vegetables and stuff like that there.” Another interviewee living in a different public housing complex echoed this message by stating, “The corner market is basically a convenience store and I think it’s mostly there for ah, junk food and you know, adults who smoke and drink beer.” An interviewee from a low-income urban community summarized spatial access to nutritious foods by stating that stores in her local food environment have “all that stuff that isn’t good for our bodies, at all.” There was a sense among many of the participants that “there would be no reason I would go … shop at the local convenience store.”
There was interest among most participants in having more balanced access to food stores in the local food environment. Participants specifically referenced a desire for farmers’ markets, meat markets, full-service grocers, and discount superstores. Locating these stores in proximity to the home was identified as a key strategy for increasing access to nutritious foods as the following interviewee highlights: “But if it’s [farmers’ market] right in the neighborhood, we could walk up there, which is a good thing, to walk up there and walk back, and you know, it’s just right there. You can’t miss it.” Imbalanced access to food stores in the local food environment was described as being “inefficient,” requiring participants to travel to several store locations for household food shopping. This inefficiency was exacerbated for participants from rural locations and those without private transportation. A focus group participant from a rural community reported that he frequented, on a weekly basis, a farmers’ market and a supermarket market that were 93 miles apart from one another. Another focus group participant from a rural area reported that she traveled 50 miles roundtrip to access a food store that sold products necessary for her health condition.
Travel time
Travel time referred to the time necessary to travel to food stores and access to reliable transportation. Most people described access in terms of how long it took to get to and from a food outlet either by car, foot, or public transportation. Some talked about choosing shopping areas with multiple stores located close together to save time and gas money. Access to food outlets as close as “within 3 minutes” was described as a positive feature of local food environments. However, many participants explained that getting food usually involved a car ride that took “between 15 and 20 minutes”. Some described a more opportunistic approach to shopping that involved going to “whatever I’m near at the moment” or whatever is on “the same little route to get to my area” and others chose stores because they were “close to home.”
Participants talked about how not having any food outlets within walking distance of the home left people without transportation “out of luck” as the following interviewee highlights:
“Because it’s rough up here … most of the people ain’t got fruits and vegetables and they need it, but the only way to get there [grocery store] is drive, because if they ain’t got no car they probably hitch hike and ride with someone else and go somewhere else to get groceries and stuff like that.
Time costs
Time costs referred to the time resources of the household available for food-related activities including shopping and preparation after taking into account other time needed for other tasks (e.g., paid work, childcare). Participants discussed factors that minimized or maximized time costs, as well as the changing demands for time. To save time, food shopping routines were established including shopping in the same place and getting the same kinds of food items. Some people described themselves as “a creature of habit” when talking about their shopping behaviors and were especially sensitive to any changes to store layout; consistency in store layout was perceived to be a method for saving time. To save time, participants reported that they chose to shop in stores during specific timeframes when they perceived them to be less crowded (e.g., Sunday morning, certain evenings).
Participants highlighted that nutritious food access was influenced by time costs related to service delivery. Not having enough staff people on registers was described as a waste of time. One interviewee emphasized this concern by stating he had to wait 30 min to get through a line because there were not enough employees in the store. Some participants reported that they would be willing to drive farther for stores with shorter lines because this ultimately saved time.
Time costs were also related to food preparation. Participants emphasized the time it takes to cook foods using fresh ingredients, as the following interviewee highlights: “There’s preparation time and so for me a lot of times decisions have been made based on my timeframe for the night, how can I use it to make a meal.” Others reported that “junk food” and other quick foods you could “just pop in your mouth” saved time over “good fruits and vegetables” that were perceived to require more time to prepare.
Participants also discussed how the pace of society has become increasingly faster over time and noted the influence of this pace on nutritious food access. Additionally, time resources both influenced and were influenced by work–family (im)balance. Participants often reported that they “just cook stuff that’s quick” because of competing demands for time, and thus looked for these quick cooking foods when shopping.
Social Access
Social access included three dimensions: (a) culture, (b) discrimination, and (c) relationships.
Culture
Culture referred to familial, racial, and ethnic foodways and traditions influencing nutritious food access. Culture influenced the foods considered acceptable or appropriate for eating, and thus purchased and consumed by the household. Family culture also influenced food preparation, which in turn influenced food shopping as the following interviewee highlights:
I was talking to my sister about greens and I was telling her I made some greens and she said, “Well, what kind of meat did you put in it?” And I was like, “I didn’t put meat in it. I haven’t cooked greens with meat in over 10 years.” She was like, “Can you cook greens with no meat?”
There was a sense that culturally-influenced family food traditions have changed over time. There was a perception that prior generations were more likely to grow their own foods and can and freeze items, limiting the need for food stores, as the following interviewee highlights: “Only thing we had to buy [when I was younger,] … we’d go to the butcher or market and get meats. That’s it, … Everything else came from out of the garden.”
Racial and ethnic cultural traditions were also deemed relevant to nutritious food access. Participants described how culturally defined food rules such as not eating pork or maintaining a vegetarian diet influenced the types of food stores and food items that are accessible. Most of the study participants were African American. Accordingly, the influence of African American culture and history on nutritious food access was frequently mentioned. A few participants harkened current eating patterns among African Americans to the slave trade, as the following interviewee highlights:
So, like, naturally, African descendants ate lots of fresh fruits and vegetables. But with the slave trade and slavery, then there were limits that were placed and there were only certain foods available. And so that’s what was eaten and then that became a part of our [African American] culture. … That’s what we eat.
Additionally, participants described how cultural influences on foods may make them socially inaccessible. Redefining the cultural boundaries of foods was identified as a method for increasing nutritious food access.
Discrimination
Discrimination referred to differential access to foods based on race, class, geographic location, and/or gender. Participants readily acknowledged that nutritious food access differed based on the racial and economic composition of a community. One interviewee described the differences in nutritious food access since she moved to a higher income neighborhood, by stating: “In [name of low-income neighborhood] the vegetables were not, they were not as fresh. In [name of higher income neighborhood], the vegetables seem to be really fresh there … seems to be a greater variety.” A similar analysis was made when participants compared nutritious food access in racial and ethnic minority communities versus predominantly White communities. Focus group participants from rural areas highlighted differences in nutritious food access compared to urban areas as the following quotation highlights:
Country folks got money too, but they [food store developers] not looking at it. They think they can just come in and just put anything in and have second-class stuff. But you know, we work, and you know, we, some of us, make pretty good living. Just like those people that live in the [higher income urban community]. And, why should we be different.
Finally, respondents reported that gender discrimination influenced nutritious food access. For some, this manifested in gender roles with women taking on the bulk of the responsibility for food shopping. For these women, nutritious food access was viewed through a lens that included personal needs, as well as the needs of family members. As the primary food shopper for the family, these women had to balance the time needed for food shopping with a long list of other demands such as childcare, work outside of the home, cooking, and cleaning. Additionally, participants highlighted differences in income based on gender and the influence this had on nutritious food access: “It just seems like there is an economic disparity based on gender. So often, men make more money than women anyway, which means that they have greater resources for food.”
Relationships
Participants stressed the importance of connections to growers, food service personnel, and/or other customers in food outlets as important social influences on nutritious food access. About half of the participants expressed a preference for purchasing foods grown locally. There was a sense of connection with locally grown products as the following interviewee highlights: “You want to support the local growers because they’re here. It’s like me supporting the home football team. They are a part of this community so you want them to be able to survive and strive and actually excel.”
Participants discussed the importance of relationships with food store personnel. One focus group participant, for instance, stated that she goes to the store nearly every day because she likes to interact with the staff. Food store personnel were considered to be part of the social network for several participants. Staff members in smaller stores were considered to be more personable than in larger stores as the following focus group participant highlights: “If you’re at a bodega, you know everybody’s name. You know the guy that cut the meat. You know the guy that makes the sandwiches. You know his family.” Participants also referenced store access in relation to their friendship networks. For some, going to a food store provided an opportunity to hang out with friends as the following interviewee highlights: “I go different places to shop. Sometimes I just go with my people just to be going.”
Personal Domain
Finally, personal factors related to nutritious food access were identified. The personal domain included factors that enhanced or diminished access to nutritious foods when systemic domains of nutritious food access were present. The personal domain included three dimensions: (a) health status, (b) knowledge, and (c) food-related identities and preferences.
Health status
Health status referred to aspects of individual and family health that influence access to food. Health status influenced both perceptions of access and selection of food outlets. Participants explained how changes in health status influenced food shopping patterns. Many participants described having limited access to foods that were needed for their specific health issues, with statements such as, “My daughter takes me like 25 miles to [name of chain supermarket] because I’m a diabetic.” Concern for the health status of children and spouses was also a main theme in the personal domain. Participants talked about aspects of family health including genetics, cancer, obesity, high blood pressure, child attention problems, and allergies. The following quote illustrates one mother’s concern for both her husband and her child:
My husband … is very heavy. I’m trying to help us … and I figure my child, you know, she has his genetics and his family is pretty heavy and I’m trying to help them and help me with the blood pressure issue. … There’s nothing wrong with my kid right now but when I felt like he was having problems, going all the way across town [to shop], you know, that would have been nice had it been closer.
Participants also reported that purchasing and consuming healthy foods had a direct impact on how they felt physically and emotionally. One participant said, “I feel better about myself when I eat something good.”
Food and nutrition knowledge
Participants talked about the importance of knowledge for accessing food, as well as the limitations of knowledge to nutritious food access. In other words, knowledge was described as being a necessary, but not sufficient, element of nutritious food access. The following quote illustrates an interviewee’s belief in the importance of community knowledge:
I think it would do good for my community … especially if they’re educated on the right foods, and with the right foods, you don’t have to worry about heart disease, colon cancer, other types of cancer, depending on what type of food you eat, because a lot of the stuff [health issues] is being traced back to food.
Other participants highlighted the limitations of knowledge to increasing nutritious food access particularly when households are operating in “survival mode” due to other family stressors.
Knowledge passed through generations was also mentioned by participants. An interviewee stressed the importance of knowledge gained from children prompting utilization of different food outlets:
The kids coming home talking about, “Momma, you know what we had? … Some vegetables at the farmers market and you need to buy some vegetables.” … That really prompted me … to want to buy some for dinner. I guess the first time I bought them and I cooked them, they were so good …. to eat fresh food. … And it tasted so good. It tasted so different. Then … I wanted more so I just try to make a point of doing that. I think some of it was just me transitioning my mind-set, because that’s the key. If people can change their minds, their behavior will follow. We often just try to change the behavior but if the mind is never changed they are going to return back to that behavior eventually.
An interviewee talked about how knowledge gained from his mother influenced his ability to access food as an adult: “Mama raised me to be independent, so she taught me how to cook. … We had to come and watch her cook when we were kids so we learned how to do it. And in doing so you learn how to shop.”
Food-related identities and preferences
Participants described how their selection of foods and food outlets was shaped by relationships between their identity as eaters and food preferences. Many participants described themselves as “healthy eaters.” Being a healthy eater was also described as being a “weird eater” by participants with family members who had different eating identities. One participant explained that she what eats gets “mixed up between what I eat and what my family eats because they are so tied together.” Other healthy eaters described eating in “moderation” and being a “healthy food shopper.” In contrast, some participants described themselves as “picky eaters” and, by extension, “picky shoppers.”
Picky eaters tended to limit the types of foods they purchased and the locations where they accessed food to those they were most familiar with or those that carried specific food items as the following focus group quotation highlights: “Because I’m a diabetic. You have to be picky. There is no other choice.”
DISCUSSION
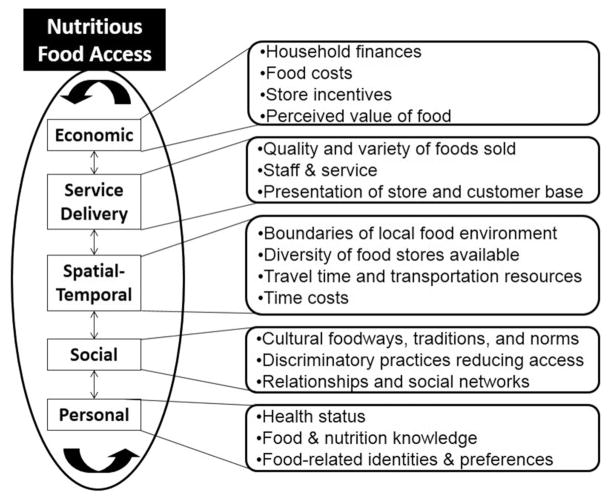
Results from the qualitative analysis reveal a multidimensional conceptual model of nutritious food access that includes five domains and related dimensions (see Figure 1). The domains include economic, service delivery, spatial–temporal, social, and personal access. Data reveal that the domains are interrelated. Spatial–temporal access, for instance, is influenced, in part, by social access such as patterns of discrimination that result in certain neighborhoods having more (or less) balanced nutritious food access. The emergent conceptual model provides guidance for policy and environmental efforts focused on improving access to healthy foods. The model emphasizes the importance of multilevel and multi-component interventions.
FIGURE 1.
Domains and related dimensions of nutritious food access.
The resulting conceptual model underscores the role of economic factors as key determinants of nutritious food access. Recent research reports or intervenes on the costs of foods in stores (Giskes et al., 2007; Glanz, Sallis, Saelens, & Frank, 2007; Hendrickson et al., 2006; Larsen & Gilliland, 2009), whereas the emergent conceptual model also explicates the relationship between household finances and nutritious food access. Thus, it is not only important to have reasonable prices for healthy foods in food stores, but also to have the financial resources to purchase these foods. Accordingly, nutritious food access initiatives ought to include parallel efforts to increase economic opportunities for households to earn a living wage for employment and to maximally benefit from food assistance programs (e.g., Supplemental Nutrition Assistance Program, Women, Infants, and Children program, food pantries). This is a logical connection for social workers to engage in nutritious food access work and expand the notion of access to include the availability and attainment of social and financial supports. Social workers may advocate for social policies to occur in tandem with nutritious food access policies to ensure individuals and families experience economic security necessary to provide for basic needs like food. Additionally, social work community practitioners may provide guidance for building food stores in food deserts in a manner that offers job training and economic security for local residents and establishes community ownership of nutritious food access through ventures such as resident-run food cooperatives and farmers’ markets.
The emergent conceptual model draws attention to service delivery factors influencing nutritious food access, which have been emphasized by others (Blitstein et al., 2012; Block & Kouba, 2006; Hendrickson et al., 2006; Zenk et al., 2006). The quality and variety of foods sold in a store, staff and service, and overall store presentation influenced food shopping decisions. Service delivery aspects of access create opportunities for store-level interventions (Gittelsohn et al., 2007). Social workers serving food insecure households may expand their practice to include efforts to ensure food stores serving low-income consumers offer high quality, fresh products and actively work to increase access to these items through efforts to expand refrigeration sections in stores, re-vision product placement and marketing, and increase the amount of locally-grown products available in food deserts.
In accord with the majority of food access research, the proposed conceptual model highlights spatial–temporal elements. Data corroborate research that highlights the negative effects of living in an imbalanced food environment (Larson, Story, & Nelson, 2009; Walker, Keane, & Burke, 2010), as well as expand the definition of what it means to have balanced access to food stores. Participants highlighted that it was not only important to have access to a food store, but to also to have access to other types of stores for full-service shopping needs. This is has importance for policy because, with the exception of the modified food retail environment index (Centers for Disease Control and Prevention, 2011), the majority of current policy-relevant measures of community food access exclusively focus on the presence of very few store types (i.e., supermarkets, fruit and vegetable markets) in geographically bounded contexts (Centers for Disease Control and Prevention, 2009; Reinvestment Fund, 2012; US Department of Agriculture, 2011). The modified food retail environment index captures the proportion of healthy food retailers in a Census tract as a function of all food retailers in the area (Centers for Disease Control and Prevention, 2011). The results of our study highlight the benefits of qualitative research, which provides a chance for participants to highlight nuances like the importance of multipurpose stores to their overall perception of nutritious food access. Social workers may further nutritious food access initiatives through efforts related to commercial business zoning policies in communities.
The data on spatial aspects of nutritious food access also have import for research. In our sample, participants differentially responded to the terms neighborhood and community when asked to think about their food environment (e.g., foods available in their neighborhood/community). In many food access studies, these words are used as cues for understanding spatial food access. One of the most popular measures of food access includes the word neighborhood in the items of the scale (e.g., “A large selection of fresh fruits and vegetables is available in my neighborhood;” Mujahid, Diez Roux, Morenoff, & Raghunathan, 2007; Mujahid et al., 2008). Our data highlight the subjectivity of this term and thus interrogate the validity of quantitative findings about food access based on questions that include terms like neighborhood or community without formative research to understand the meaning of this term in the study population. Social work scholars have highlighted the dynamism of concepts like neighborhood and community and have shown that even people living near each other have different definitions of the boundaries of their neighborhood; these boundaries frequently do not coincide with administratively defined boundaries (Coulton, Chan, & Mikelbank, 2011). Nutritious food access research and related policy would be enhanced with more in-depth analysis of the meanings of spatial boundaries for neighborhoods and communities, generally, and food environments, specifically.
The spatial–temporal domain of nutritious food access also illuminates the value of time to many households. This resource is particularly limited for those working one or more jobs, caring for children or other family members, living in areas with limited store options, and without access to transportation. Temporal aspects of nutritious food access highlight the importance of integrating multi-sector approaches to improving food access. In particular, transportation and city planning are central to intervention efforts aimed to improve food environments. This type of integration would not only address public transportation routes and nutritious food access, but also address design features such as including multiple store options in one central location. Additionally, the presence of work–family demands was a particularly salient theme among female participants, which is consistent with the literature on work–family spillover (Blake et al., 2009; Blake, Wethington, Farrell, Bisogni, & Devine, 2011; Devine, Connors, Sobal, & Bisogni, 2003; Grzywacz, Almeida, & McDonald, 2002). Interventions aimed at improving nutritious food access need to consider disparities in time for shopping and food preparation. Temporal access to food is influenced by work, family, and other demands and may be as influential on one’s ability to access food through other domains.
The social domain of nutritious food access reveals broader socio-cultural factors influencing access such as family and ethnic foodways, as well as patterns of discrimination based on race, class, gender, and geographic location. Our data reveal that social factors make certain foods inaccessible, even when they are available according to other domains. For instance, if certain foods are considered “not for us” based on cultural food rules (Freedman, 2011; Lewin, 1997), their presence in a neighborhood store at a reasonable price may have little influence on shopping patterns. Moreover, social networks were identified as key aspects of nutritious food access, including being connected to store personnel or food producers as well as shopping with friends and family. These factors create new venues for social work intervention, such as exploring cultural foodways and working with individuals and communities to reconnect contemporary eating patterns with historical perspectives. This process may reveal structural barriers to accessing and consuming certain foodstuff. It may also provide opportunities for empowering communities to transgress contemporary food norms because historical practices included the provision of certain, potentially healthier, foodstuff. Social work’s commitment to social justice and to addressing the needs of oppressed groups makes the field poised to further nutritious food access research and practice to more purposefully address the role of discrimination in food (in)access and related outcomes like obesity and food insecurity. Moreover, social workers have the potential to expand nutritious food access initiatives by advocating for more just policies for historically marginalized groups. Wage parity policies, for instance, would influence nutritious food access by increasing economic resources for families, as well as time available for food-related activities if people are able to work fewer hours because of more equitable pay. However, these types of economic policies have not been central to current food access policy initiatives.
Finally, the personal domain of nutritious food access highlights the importance of multilevel interventions, a key tenet of ecological perspectives (Bronfenbrenner, 1977). Our data suggest that food environment researchers should not focus exclusively on systemic approaches for improving nutritious food access. Instead, individual-level interventions ought to be incorporated into multilevel approaches (Pomerleau, Lock, Knai, & McKee, 2005). This aligns with research on access in other arenas. Access to healthcare, for instance, has been conceptualized to include structural factors (e.g., availability of medical home, lack of childcare resources) and financial factors (e.g., cost of care, health insurance) as well as cognitive factors (knowledge, communication; Carrillo, Carrillo, Perez, Salas-Lopez, Natale-Pereira, & Byron, 2011). Scholarship on food choice and consumption behaviors, an outcome associated with nutritious food access, also highlights personal factors such as food choice values (Sobal & Bisogni, 2009), nutrition information (Glanz, Sallis, Saelens, & Frank, 2005), and personal health concerns (Jilcott, Laraia, Evenson, & Ammerman, 2009) influencing differential uptake of foods that are systemically accessible. Our data highlighted that lack of nutritious food-related knowledge may reduce access when other domains of food access are addressed. However, addressing personal factors alone was considered to be insufficient for promoting nutritious food access. Personal factors such as nutrition-related knowledge and personal or familial health status influenced nutritious food access. In our sample, we found that having a health condition requiring certain dietary habits or eating healthy foods as a form of prevention caused some food stores to be “off limits” even when they were accessible in other domains. Similarly, eating identities and preferences influenced store accessible. Nutritious food access interventions that target contexts where diet-related health conditions are prevalent may be particularly useful (e.g., establishing a grocery store in an area with high rates of diabetes). Incorporating an educational intervention in conjunction with this type of community-level intervention may further enhance nutritious food access.
Strengths and Limitations
As with all studies, this research has both strengths and limitations. Key strengths include the qualitative research approach, which allowed for the exploration of the nuances of nutritious food access without the constraints of closed-ended questions (Schensul, Schensul, & LeCompte, 1999). The study population is another strength, which included participants from two states in the southeastern region of the United States with variation related to race, class, gender, and geographic region (e.g., rural/urban). Given the small sample size, however, the participants may not be representative. The goal in grounded theory analysis is to have a range of perspectives inform the data collection process through purposeful and maximum variation sampling (Charmaz, 2001). This adds to the complexity of the emergent model. Targeted analyses are needed to determine the relevance of the model to specific populations. Additionally, the interview participants were selected at a farmers’ market; they may have different views about nutritious food access than people who do not frequent farmers’ markets.
Conclusion
In conclusion, this study makes an important contribution to food environment research by providing a conceptual model that can be tested with other populations and refined. Efforts are needed to measure each domain and related dimension of nutritious food access and delineate the relative importance of these factors with diverse populations in diverse contexts (McKinnon, Reedy, Morrissette, Lytle, & Yaroch, 2009). The conceptual model also provides practical guidance to policy makers and program administrators working to improve nutritious food access in communities. Most important, the model highlights that nutritious food access is multifaceted and cannot be addressed through myopic approaches. In other words, nutritious food access for populations may not improve by simply building a grocery store in a food desert. Instead, economic, service delivery, social, and personal domains of nutritious food access ought to be addressed in tandem with spatial–temporal efforts. Social work scholars and practitioners have the potential to contribute expertise to this growing field by offering a broader concept of the social determinants of nutritious food access. Through transdisciplinary and cross-sector collaboration with colleagues from public health, medicine, nursing, city planning, transportation, and human geography, social workers engagement in food environment work may ultimately facilitate more equitable access to food in communities and may shift the focus of nutritious food access initiatives to realize the goal of food justice and health equity.
Acknowledgments
FUNDING
This research was supported by grants from the National Cancer Institute (R21CA132133-02-S1) and the Vanderbilt Center for Community Studies. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Cancer Institute, the National Institutes of Health, or the Vanderbilt Center for Community Studies. We thank the interview and focus group participants for their insights and contributions to this research. We are thankful to Jeff Hatala and Denika Hiter Lomax for research assistance, and Michelle Kaiser, Carrier Draper, and the anonymous reviewers for their thoughtful comments on earlier versions of the article.
Footnotes
We do not have any actual or potential conflicts of interest related to this research.
Contributor Information
DARCY A. FREEDMAN, Case Western Reserve University, Cleveland, OH, USA
CHRISTINE E. BLAKE, Arnold School of Public Health, University of South Carolina, Columbia, SC, USA
ANGELA D. LIESE, Arnold School of Public Health, University of South Carolina, Columbia, SC, USA
References
- Baker E, Schootman M, Barnidge E, Kelly C. The role of race and poverty in access to foods that enable individuals to adhere to dietary guidelines. Preventing Chronic Disease. 2006;3(3):1–11. [PMC free article] [PubMed] [Google Scholar]
- Blake CE, Devine CM, Wethington E, Jastran M, Farrell TJ, Bisogni CA. Employed parents’ satisfaction with food choice coping strategies: Influence of gender and household structure. Appetite. 2009;52(3):711–719. doi: 10.1016/j.appet.2009.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blake CE, Wethington E, Farrell TJ, Bisogni CA, Devine CM. Behavioral contexts, food choice coping strategies, and dietary quality of a multiethnic sample of employed parents. Journal of the American Dietetic Association. 2011;111:1–7. doi: 10.1016/j.jada.2010.11.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blitstein JL, Snider J, Evans WD. Perceptions of the food shopping environment are associated with greater consumption of fruits and vegetables. Public Health Nutrition. 2012;15:1124–1129. doi: 10.1017/S1368980012000523. [DOI] [PubMed] [Google Scholar]
- Block D, Kouba J. A comparison of the availability and affordability of a market basket in two communties in the Chicago area. Public Health Nutrition. 2006;9:837–845. doi: 10.1017/phn2005924. [DOI] [PubMed] [Google Scholar]
- Bronfenbrenner U. Toward an experimental ecology of human development. American Psychologist. 1977;32:513–531. [Google Scholar]
- Bywaters P. Tackling inequalities in health: A global challenge for social work. British Journal of Social Work. 2009;39:353–367. [Google Scholar]
- Calle EE, Thun MJ. Obesity and cancer. Oncogene. 2004;23:6365–6378. doi: 10.1038/sj.onc.1207751. [DOI] [PubMed] [Google Scholar]
- Carrillo JE, Carrillo VA, Perez HR, Salas-Lopez D, Natale-Pereira A, Byron AT. Defining and targeting health care access barriers. Journal of Health Care for the Poor and Underserved. 2011;22:562–575. doi: 10.1353/hpu.2011.0037. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. State indicator report on fruits and vegetables, 2009. Atlanta, GA: Author; 2009. [Google Scholar]
- Centers for Disease Control and Prevention. Children’s food environment state indictor report, 2011. Atlanta, GA: Author; 2011. [Google Scholar]
- Charmaz K. Grounded theory. In: Emerson RM, editor. Contemporary field research. Long Grove, IL: Waveland; 2001. pp. 335–352. [Google Scholar]
- Chung C, Myers SL. Do the poor pay more for food? An analysis of grocery store availability and food price disparities. Journal of Consumer Affairs. 1999;33(2):276–296. [Google Scholar]
- Coleman-Jensen A, Nord M, Andrews M, Carlson S. In: Household food security in the United States in 2011. Service ER, editor. Washington, DC: US Department of Agriculture; 2012. [Google Scholar]
- Coulton C, Chan T, Mikelbank K. Finding place in community change initiatives: Using GIS to uncover resident perceptions of their neighborhoods. Journal of Community Practice. 2011;19:10–28. [Google Scholar]
- Devine CM, Connors MM, Sobal J, Bisogni CA. Sandwiching it in: Spillover of work onto food choices and family roles in low- and moderate-income urban households. Social Science and Medicine. 2003;56:617–630. doi: 10.1016/s0277-9536(02)00058-8. [DOI] [PubMed] [Google Scholar]
- Drewnowski A, Aggarwal A, Hurvitz PM, Monsivais P, Moudon AV. Obesity and supermarket access: Proximity or price? American Journal of Public Health. 2012;102:e74–e80. doi: 10.2105/AJPH.2012.300660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dutko P, Ver Ploeg M, Farrigan T. Economic Research Service, editor. Characteristics and influential factors of food deserts. Washington, DC: US Department of Agriculture; 2012. [Google Scholar]
- Evans RG, Barer ML, Marmor TR, editors. Why are some people health and others not? The determinants of health of populations. New York, NY: Aldine de Gruyter; 1994. [Google Scholar]
- Flegal KM, Carroll MD, Ogden CL, Curtin LR. Prevalence and trends in obesity among US adults, 1999–2008. Journal of the American Medical Association. 2010;303:235–241. doi: 10.1001/jama.2009.2014. [DOI] [PubMed] [Google Scholar]
- Franklin B, Jones A, Love D, Puckett S, Macklin J, White-Means S. Exploring mediators of food insecurity and obesity: A review of recent literature. Journal of Community Health. 2012;37:253–264. doi: 10.1007/s10900-011-9420-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freedman DA. Local food environments: they’re all stocked differently. American Journal of Community Psychology. 2009;44:382–393. doi: 10.1007/s10464-009-9272-6. [DOI] [PubMed] [Google Scholar]
- Freedman DA. Embodying food studies: unpacking the ways we become what we eat. In: Casper MJ, Currah P, editors. Corpus: An interdisciplinary reader on bodies and knowledge. New York, NY: Palgrave Macmillan; 2011. pp. 81–94. [Google Scholar]
- Freedman DA, Bell BA, Collins LV. The veggie project: A case study of a multi-component farmers’ market intervention. Journal of Primary Prevention. 2011;32:213–224. doi: 10.1007/s10935-011-0245-9. [DOI] [PubMed] [Google Scholar]
- Giskes K, Van Lenthe FJ, Brug J, Mackenbach JP, Turrell G. Socioeconomic inequalities in food purchasing: the contribution of respondent-perceived and actual (objectively measured) price and availability of foods. Preventive Medicine. 2007;45:41–48. doi: 10.1016/j.ypmed.2007.04.007. [DOI] [PubMed] [Google Scholar]
- Gittelsohn J, Franceschini MC, Rasooly IR, Ries AV, Ho LS, Pavlovich W, Frick KD. Understanding the food environment in a low-income urban setting: implications for food store interventions. Journal of Hunger and Environmental Nutrition. 2007;2:33–50. [Google Scholar]
- Glanz K, Sallis JF, Saelens BE, Frank LD. Health nutrition environments: Concepts and measures. American Journal of Health Promotion. 2005;19:330–333. doi: 10.4278/0890-1171-19.5.330. [DOI] [PubMed] [Google Scholar]
- Glanz K, Sallis JF, Saelens BE, Frank LD. Nutrition environment measures survey in stores (NEMS-S): development and evaluation. American Journal of Preventive Medicine. 2007;32:282–289. doi: 10.1016/j.amepre.2006.12.019. [DOI] [PubMed] [Google Scholar]
- Glaser BG, Strauss AL. The discovery of grounded theory: strategies for qualitative research. Chicago, IL: Aldine; 1967. [Google Scholar]
- Grzywacz JG, Almeida DM, McDonald DA. Work-family spillover and daily reports of work and family stress in the adult labor force. Family Relations. 2002;51:28–36. [Google Scholar]
- Hendrickson D, Smith C, Eikenberry N. Fruit and vegetable access in four low-income food deserts communities in Minnesota. Agriculture and Human Values. 2006;23:371–383. [Google Scholar]
- Hu FB, Manson JE, Stampfer MJ, Colditz G, Liu S, Solomon CG, Willett WC. Diet, lifestyle, and the risk of Type 2 diabetes mellitus in women. New England Journal of Medicine. 2001;345:790–797. doi: 10.1056/NEJMoa010492. [DOI] [PubMed] [Google Scholar]
- Jilcott SB, Laraia BA, Evenson KR, Ammerman AS. Perceptions of the community food environment and related influences on food choice among midlife women residing in rural and urban areas: A qualitative analysis. Women Health. 2009;49:164–180. doi: 10.1080/03630240902915085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khan LK, Sobush K, Keener D, Goodman K, Lowry A, Kakietek J, Zaro S. Recommended community strategies and measurements to prevent obesity in the United States. Morbity and Mortaility Weekly Report. 2009;58(RR07):1–26. [PubMed] [Google Scholar]
- Kindig D, Stoddart G. What is population health? American Journal of Public Health. 2003;93:380–383. doi: 10.2105/ajph.93.3.380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larsen K, Gilliland J. A farmers’ market in a food desert: Evaluating impacts on the price and availability of healthy food. Health & Place. 2009;15:1158–1162. doi: 10.1016/j.healthplace.2009.06.007. [DOI] [PubMed] [Google Scholar]
- Larson N, Story M, Nelson M. Neighborhood environments: Disparities in access to healthy foods in the U.S. American Journal of Preventive Medicine. 2009;36:74–81. doi: 10.1016/j.amepre.2008.09.025. [DOI] [PubMed] [Google Scholar]
- Lewin K. Resolving social conflicts: Field theory in social science. Washington, DC: American Psychological Association; 1997. Psychological ecology (1943) pp. 289–300. [Google Scholar]
- Liese AD, Bell BA, Barnes TL, Colabianchi N, Hibbert J, Blake CE, Freedman DA. Environmental influences on fruit and vegetable intake: Results from a path analytic model. Public Health Nutrition. 2013 doi: 10.1017/S1368980013002930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liese AD, Weis KE, Pluto D, Smith E, Lawson A. Food store types, availability, and cost of foods in a rural environment. Journal of the American Dietetic Association. 2007;107:1916–1923. doi: 10.1016/j.jada.2007.08.012. [DOI] [PubMed] [Google Scholar]
- McElroy SL, Kotwal R, Malhorta S, Nelson EB, Keck PE, Nemeroff CB. Are mood disorders and obesity related? A review for the mental health professional. Journal of Clinical Psychiatry. 2004;65:634–651. doi: 10.4088/jcp.v65n0507. [DOI] [PubMed] [Google Scholar]
- McKinnon RA, Reedy J, Morrissette MA, Lytle LA, Yaroch AL. Measure of the food environment: A compilation of the literature, 1990–2007. American Journal of Preventive Medicine. 2009;36:S124–S133. doi: 10.1016/j.amepre.2009.01.012. [DOI] [PubMed] [Google Scholar]
- Miles MB, Huberman AM. Making good sense: drawing and verifying conclusions. In: Miles MB, Huberman AM, editors. Qualitative data analysis. Thousand Oaks, CA: Sage; 1994. pp. 245–280. [Google Scholar]
- Moore L, Diez Roux A. Associations of neighborhood characteristics with location and type of food stores. American Journal of Public Health. 2006;96:325–331. doi: 10.2105/AJPH.2004.058040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morland K, Wing S, Diez Roux A, Poole C. Neighborhood characteristics associated with the location of food stores and food service places. American Journal of Preventive Medicine. 2002;22:23–29. doi: 10.1016/s0749-3797(01)00403-2. [DOI] [PubMed] [Google Scholar]
- Mujahid MS, Diez Roux AV, Morenoff JD, Raghunathan R. Assessing the measurement proporties of neighborhood scales: from psychometics to ecometrics. American Journal of Epidemiology. 2007;165:858–867. doi: 10.1093/aje/kwm040. [DOI] [PubMed] [Google Scholar]
- Mujahid MS, Diez Roux AV, Shen M, Gowda D, Sanchez B, Shea S, Jackson SA. Relation between neighborhood environments and obesity in the Multi-Ethnic Study of Atherosclerosis. American Journal of Epidemiology. 2008;167:1349–1357. doi: 10.1093/aje/kwn047. [DOI] [PubMed] [Google Scholar]
- National Research Council. Committee on National Statistics, Division of Behavioral and Social Sciences and Education. Washington, DC: The National Academies Press; 2005. Measuring food insecurity and hunger: Phase 1 Report. Panel to Review US Department of Agriculture’s Measurement of Food Insecurity and Hunger. [Google Scholar]
- Oakes JM, Masse LC, Messer LC. Work group III: Methodologic issues in research on the food and physical activity environments, addressing data complexity. American Journal of Preventive Medicine. 2009;36:S177–S181. doi: 10.1016/j.amepre.2009.01.015. [DOI] [PubMed] [Google Scholar]
- Obama, Michelle & American Academy of Pediatrics (AAP) Let’s move: America’s move to raise a healthier generation of kids. Retrieved January 20, 2011, from http://www.letsmove.gov/
- Ogden CL, Carroll MD, Curtin LR, Lamb MM, Flegal KM. Prevalence of high body mass index in US children and adolescents, 2007–2008. Journal of the American Medical Association. 2010;303:242–249. doi: 10.1001/jama.2009.2012. [DOI] [PubMed] [Google Scholar]
- Pan L, Galuska DA, Sherry B, Hunter AS, Rutledge GE, Dietz WH, Balluz LS. Differences in prevalence of obesity among black, white, and Hispanic adults—United States, 2006–2008. Morbidity and Mortality Weekly Report. 2009;58:740–744. [PubMed] [Google Scholar]
- Phillips N. Revival: Grocery, credit union open after 5 years. The State. 2008 Jul 27; Retrieved December 31, 2012 from http://www.thestate.com/520/story/472397.html.
- Pomerleau J, Lock K, Knai C, McKee M. Interventions designed to increase fruit and vegetable intake can be effective: a systematic review of the literature. Journal of Nutrition. 2005;135:2486–2495. doi: 10.1093/jn/135.10.2486. [DOI] [PubMed] [Google Scholar]
- Reinvestment Fund. Searching for markets: The geography of inequitable access to healthy and affordable food in the United States. Philadelphia, PA: Author; 2012. [Google Scholar]
- Schensul SL, Schensul JJ, LeCompte MD. Essential ethnographic methods: observations, interviews, and questionnaires. Walnut Creek, CA: AltaMira Press; 1999. [Google Scholar]
- Scientific Software Development. ATLAS.ti (Version 5.2.0) Berlin, Germany: Scientific Software Development; 2011. [Google Scholar]
- Sobal J, Bisogni CA. Constructing food choice decisions. Annals of Behavioral Medicine. 2009;38(Suppl 1):37–46. doi: 10.1007/s12160-009-9124-5. [DOI] [PubMed] [Google Scholar]
- Story M, Kaphingst KM, Robinson-O’Brien R, Glanz K. Creating healthy food and eating environments: Policy and environmental approaches. Annual Review of Public Health. 2008;29:253–272. doi: 10.1146/annurev.publhealth.29.020907.090926. [DOI] [PubMed] [Google Scholar]
- Story M, Giles-Corti B, Yaroch AL, Cummins S, Frank LD, Huang TT, Lewis LB. Work group IV: future directions for measures of the food and physical activity environments. American Journal of Preventive Medicine. 2009;36:S182–S188. doi: 10.1016/j.amepre.2009.01.008. [DOI] [PubMed] [Google Scholar]
- Szreter S. The population health approach in historical perspective. American Journal of Public Health. 2003;93:421–431. doi: 10.2105/ajph.93.3.421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Department of Agriculture. Access to affordable and nutritious food: measuring and understanding food deserts and their consequences. Washington, DC: Economic Research Service, US Department of Agriculture; 2009. [Google Scholar]
- U.S. Department of Agriculture. Dietary guidelines for Americans. 7. Washington, DC: US Government Printing Office; 2010. [Google Scholar]
- U.S. Department of Agriculture. Food desert locator. 2011 Retrieved December 19, 2011, from http://www.ers.usda.gov/data/fooddesert/about.html.
- U.S. Department of Agriculture. Creating access to healthy, affordable food: Frequently asked questions. 2012 Retrieved January 16, 2013, from http://apps.ams.usda.gov/fooddeserts/FAQ.aspx.
- U.S. Department of Health and Human Services. Obama administration details Healthy Food Financing Initiative. 2010 Retrieved November 6, 2010, from http://www.hhs.gov/news/press/2010pres/02/20100219a.html.
- Walker RE, Keane CR, Burke JG. Disparities and access to healhty food in the United States: A review of food deserts literature. Health & Place. 2010;16:876–884. doi: 10.1016/j.healthplace.2010.04.013. [DOI] [PubMed] [Google Scholar]
- Wang Y, Beydoun MA. The obesity epidemic in the United States—Gender, age, socioeconomic, racial/ethnic, and geographic characteristics: A systematic review and meta-regression analysis. Epidemiologic Reviews. 2007;29:6–28. doi: 10.1093/epirev/mxm007. [DOI] [PubMed] [Google Scholar]
- Warnecke RB, Oh A, Breen N, Gehlert S, Paskett E, Tucker KL, Hiatt RA. Approaching health disparities from a population perspective: The National Institutes of Health Centers for Population Health and Health Disparities. American Journal of Public Health. 2008;98:1608–1615. doi: 10.2105/AJPH.2006.102525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss RS. Learning from strangers: the art and method of qualitative interviews. New York, NY: Free Press; 1994. [Google Scholar]
- Whitehead M, Dahlgren G. What can be done about inequalities in health? Lancet. 1991;338:1059–1063. doi: 10.1016/0140-6736(91)91911-d. [DOI] [PubMed] [Google Scholar]
- World Health Organization. Overweight and obesity fact sheet(No. 311) 2013 Mar; Retrieved July 26, 2013 from http://www.who.int/mediacentre/factsheets/fs311/en/
- Wrigley N, Warm D, Margetts B. Deprivation, diet, and food-retail access: Findings from teh Leeds ‘food deserts’ study. Enviornment and Planning. 2003;35:151–188. [Google Scholar]
- Zenk SN, Schulz AJ, Israel BA, James SA, Bao SM, Wilson ML. Fruit and vegetable access differs by community racial composition and socioecnomic position in Detroit, Michigan. Ethnicity & Disease. 2006;16:275–280. [PubMed] [Google Scholar]