Abstract
Aim of the study
The purpose of this study was to assess the concentration of urokinase-type plasminogen activator receptor (uPAR) in the serum of 103 women with breast cancer. Commonly recognized prognostic factors were taken into account, including age, histological grade of malignancy, stage of clinical advancement of the disease, status of local axillary lymph nodes and the size of the primary tumour.
Material and methods
The concentration of uPAR was assessed using an enzyme-linked immunosorbent assay (R&D Systems).
Results
The concentration of uPAR in women with breast cancer was found to be higher than in a control group and the difference was statistically significant. The concentration of uPAR was found to increase in line with increasing disease stage and this too was of statistical significance. Raised levels of uPAR were found in women with breast cancer both with and without metastases to the lymph nodes of the axilla. A positive relationship was also found between the concentration of the tested receptor and the size of the primary tumour. No significant relationship, however, was found between the concentration of uPAR and the histological grade of malignancy of the tumour. No statistically significant results were obtained regarding the menopausal status of the women, that is, whether they were pre- or post-menopausal.
Conclusions
Concentration of uPAR in serum of women with breast cancer is positively correlated with the stage of advancement of the disease. Thus, the assessment of this parameter can be useful in the clinical evaluation of women with breast cancer.
Keywords: fibrinolysis, metastasis, breast cancer, uPAR, plasminogen activation system
Introduction
A significant role in the growth of malignant tumours and in the formation of metastases is played by new blood vessels formed by the process of neoangiogenesis [1, 2]. Substances which play roles in the process arise from the vascular endothelial cells, from the tumour cells, and from the extracellular matrix (ECM). The many components produced have various functions, in which proteases have a regulatory role, such as inhibitors and receptors of the urokinase plasminogen activation system, including urokinase-type plasminogen activator (uPA), its receptors (uPAR – urokinase-type plasminogen activator receptor) and inhibitors PAI-1 and PAI-2 (plasminogen activator inhibitors) [3]. These components of the system not only take part in digestion, thus mobilising the endothelial cells into formation of new vessels, but also stimulate cancer cells to migrate and to form new remote metastases. One of the proteins of the plasminogen activation system which plays an important role in metastasis is urokinase (uPA), arising from the inactive precursor pro-uPA [4]. The functioning enzyme, whose role is to convert plasminogen into plasmin, is formed when urokinase binds with its specific membrane bound receptor – uPAR [6]. The uPAR receptor is a glycoprotein, of molecular weight 45–60 kDa, comprising 283 amino acids. The gene for this receptor is localised on chromosome 19q13.2, and is formed from 7 exons divided by 6 introns. In structure, the N-terminal fragment is bound with uPA and the C-terminal fragment is bound with the cell membrane by a glycosyl-phosphatidylinositol (GPI) chain [6]. To date, uPAR receptors have been identified on the surface of monocytes, granulocytes, fibroblasts, keratinocytes, vascular endothelial cells and cancer cells [7]. The expression of this receptor has also been observed in populations of macrophages and intravascular neutrophils. It has been shown that, on the surface of these cells, the uPAR takes an insoluble form, whilst the soluble form known as suPAR may be found in the plasma, in urine and in effusions from malignancies [7]. Scientific works in recent years have described increased expression of this receptor in cancers of the stomach, large intestine, ovary, endometrium and in cases of melanoma [8–12]. The authors of these studies noted that both the receptor (uPAR) and its complex with urokinase (uPA/uPAR) bring about changes regarding the invasiveness of cancer cells into the tissues surrounding the tumour. This is mostly through degradation of the ECM by these complexes, by stimulation of angiogenesis and by regulation of cell migration [12]. Recently it was suggested that the high concentration of uPA and the uPAR noted in the bodily fluids of many cancer patients may be of use in the diagnosis and prognosis of malignant diseases [12]. The purpose of this study was to assess the concentration of uPAR in the serum of breast cancer patients and its dependency on various commonly accepted prognostic factors, such as age, disease advancement, grade of tumour malignancy, the status of local axillary lymph nodes and the size of the tumour.
This study is a continuation of our previous studies into the role of the fibrinolytic system in women with primary breast cancer.
Material and methods
The concentration of urokinase-type plasminogen activator receptor was assessed in the serum of 103 women with breast cancer. Patients with primary breast cancer, before first surgery, were included in the study. Patients who used neoadjuvant chemotherapy were excluded from the study group. The women were aged between 29 and 89 years (average age 56 years) and were treated in the Department of Oncology Surgery of the Poznan University of Medical Sciences. In each case, the diagnosis had been confirmed by histopathology tests carried out in the Department of Tumour Pathology, also of the Poznan University of Medical Sciences. A group of 40 healthy women, aged between 24 and 75 years (average 47 years), comprised the control group. The authors obtained the agreement of the Bioethics Committee of the University of Medical Sciences, in order to carry out the study. Clinical characteristics of the breast cancer patients are presented in Table 1.
Table 1.
Clinical characteristics of patients with breast cancer
| Clinical characteristic | Number of patients | Percentage of tested patients (%) |
|---|---|---|
| Age | ||
| pre-menopausal | 31 | 30.1 |
| post-menopausal | 72 | 69.9 |
| Stage of clinical disease advancement according to TNM | ||
| I | 47 | 45.6 |
| II | 38 | 36.9 |
| III | 18 | 17.5 |
| Status of local axillary lymph nodes | ||
| pN0 | 51 | 49.5 |
| pN1 | 52 | 50.5 |
| Size of the primary tumour | ||
| pT < 20 mm | 54 | 52.4 |
| pT ≥ 20 ≤ 50 mm | 40 | 38.9 |
| pT ≥ 50 mm | 9 | 8.7 |
| Histological grade of malignancy | ||
| G1 | 11 | 10.7 |
| G2 | 50 | 48.5 |
| G3 | 42 | 40.8 |
Approximately 5 ml of venous blood was collected into clotting tubes from each patient. After about 30 minutes, the samples were centrifuged at 1000 rpm for 10 minutes. After centrifugation, the serum was isolated into 0.5 ml tubes and frozen at –20°C. The prepared tubes were stored in this manner until the time of testing, but not for more than six months. The concentration of uPAR was assessed using a “sandwich” type enzyme-linked immunosorbent assay (ELISA) from R&D Systems.
Statistical analysis
The obtained uPAR concentrations were subjected to statistical analysis using Statistica 8.0 software. Prior to analysis the variables were tested for normal distribution using the Shapiro-Wilk W test. For the purposes of identifying differences between the tested groups the Mann-Whitney U test was applied. Statistical hypotheses were accepted where the level of significance was p < 0.05.
Results
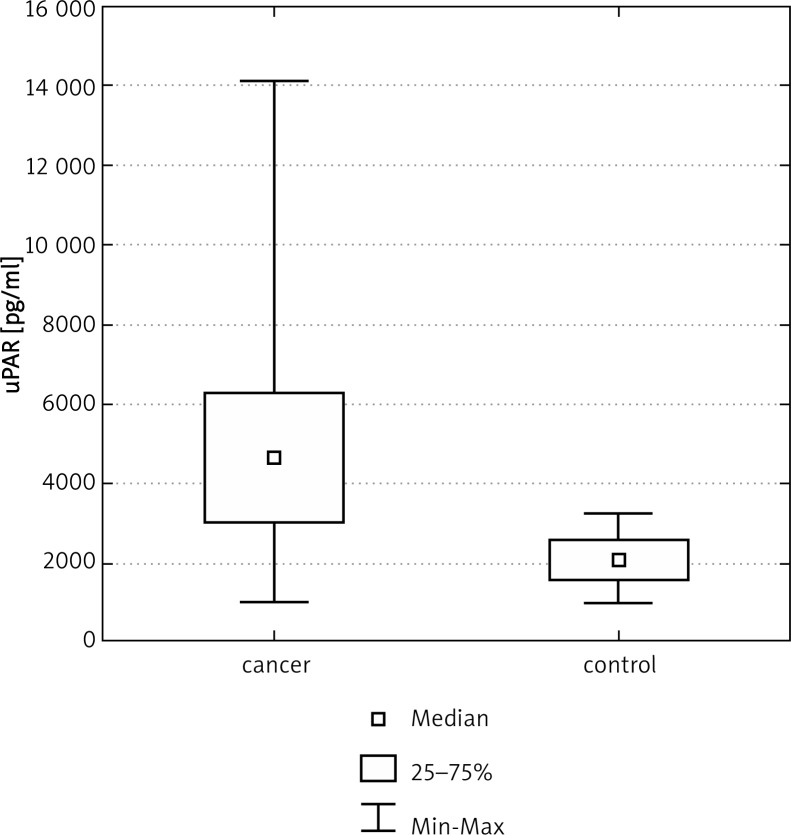
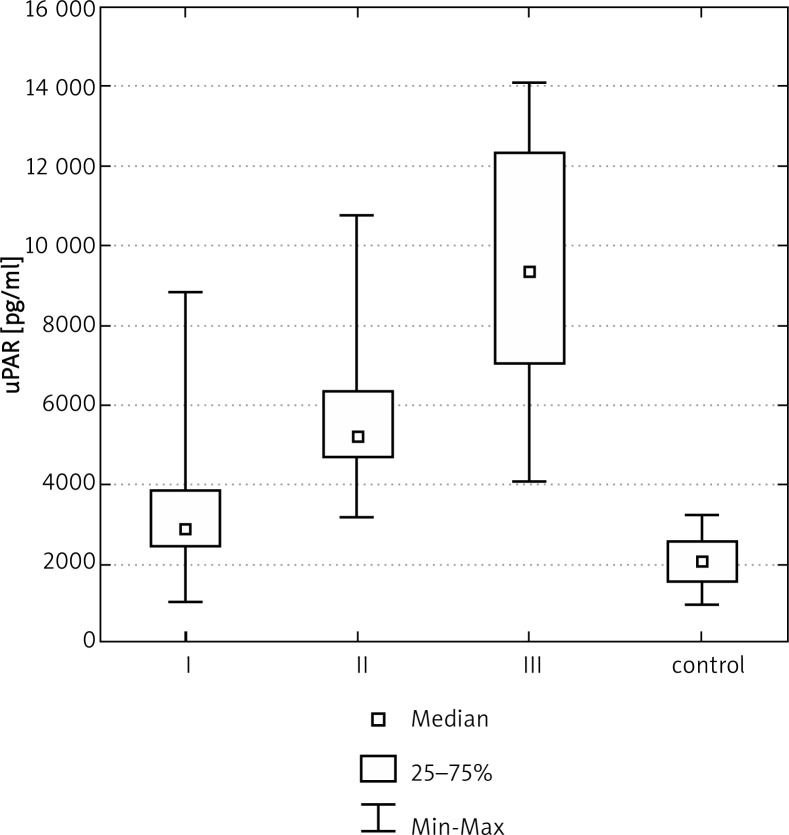
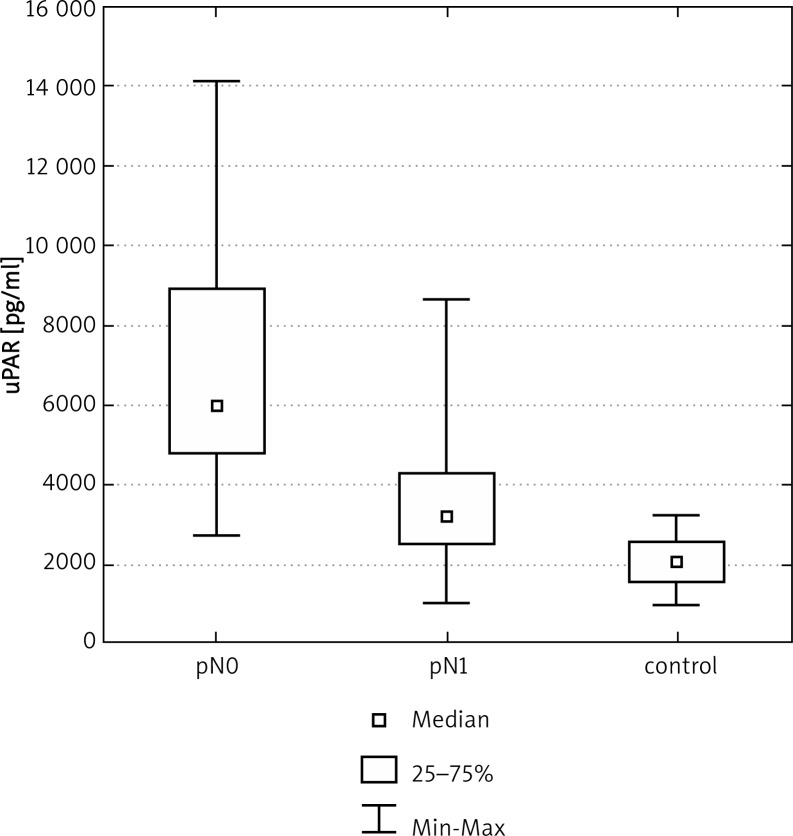
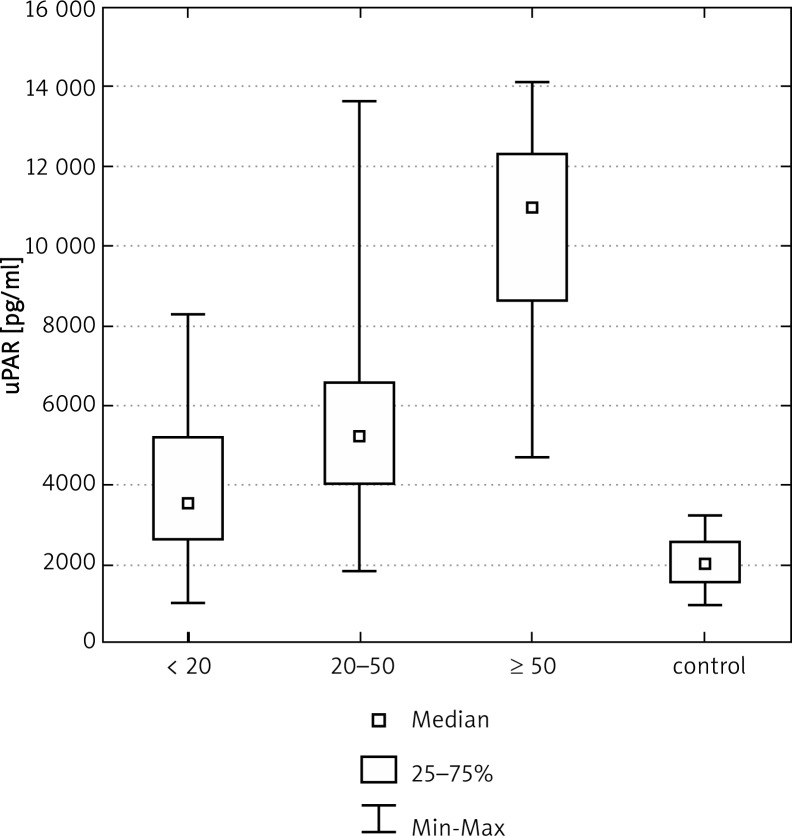
In the group of 103 women with breast cancer the median concentration of urokinase-type plasminogen activator receptor (uPAR) was more than 2.5 times greater than in the control group, and this difference was found to be statistically significant (Table 2, Fig. 1). The analysis of results also showed that the mean concentration of uPAR in the serum of post-menopausal women was significantly higher than in pre-menopausal patients (Table 2). The median concentration of uPAR was also found to increase in line with disease advancement (Table 2, Fig. 2). The highest median concentration of uPAR was found in the serum of women in stage III of disease advancement and this was found to be statistically significant in comparison with the levels found in women whose disease was in stage I or II (Table 2). A significant difference was also found between uPAR levels in patients in stage II of disease advancement, when compared to those in stage III. Another statistically significant difference was identified when comparing the levels of uPAR in the serum of women with metastases to the axillary lymph nodes to those without metastases (Table 2, Fig. 3). Further analysis showed that there is no relationship between the grade of histological malignancy and median uPAR concentration (Table 2). There is, however, a relationship of statistical significance between the concentration of uPAR in the serum of women whose tumour is sized less than 20 mm, between 20 mm and 50 mm, or greater than 50 mm in diameter (Table 2, Fig. 4).
Table 2.
Concentration of uPAR in patients with breast cancer and its relationship to age, stage of clinical advancement of disease, status of lymph nodes, tumour size and histological malignancy
| Patient characteristic | uPAR | |
|---|---|---|
|
|
||
| Median uPAR concentration [pg/ml] | uPAR concentration range [pg/ml] | |
| Control group n = 40 | 2039.8 | 1010.2–3231.5 |
| Breast cancer patients n = 103 | 4660.0* | 1020.4–14124.0 |
| Pre-menopausal | 3901.8* | 1020.4–14057.3 |
| Post-menopausal | 4882.2* | 1803.2–14124.0 |
| Stage of clinical disease advancement according to TNM | ||
| I n = 47 | 2901.3* | 1020.4–8831.2 |
| II n = 38 | 5263.8* & | 3189.4–10804.1 |
| III n = 18 | 9327.6* & # | 4071.5–14124.0 |
| Axillary lymph node status | ||
| pN0 n = 51 | 3189.4* | 1020.4–8636.4 |
| pN1 n = 52 | 6005.6* ▼ | 2709.4–14124.0 |
| Tumour size | ||
| pT < 20 mm n = 54 | 3543.2* | 1020.4–8327.9 |
| pT ≥ 20 < 50 mm n = 40 | 5246.8* ◆ | 1853.4–13676.1 |
| pT ≥ 50 mm n = 9 | 10986.1* ◆ ■ | 4705.0–14124.0 |
| Histological grade of malignancy | ||
| G1 n = 11 | 3429.3 | 1120.8–9001.2 |
| G2 n = 50 | 4202.1* | 1020.4–14057.3 |
| G3 n = 42 | 5588.6* | 1901.6–14124.0 |
n – number of tested women
Statistically significant difference for uPAR in comparison to control group, p < 0.05
Statistically significant difference for uPAR in comparison to the group of women in stage I of disease advancement, p < 0.05
Statistically significant difference for uPAR in comparison to the group of women in stage II of disease advancement, p < 0.05
Statistically significant difference for uPAR in comparison to women without metastases to the axillary lymph nodes, p < 0.05
Statistically significant difference for uPAR in comparison to women whose tumour measured < 20 mm, p < 0.05
Statistically significant difference for uPAR in comparison to women whose tumour measured ≥ 20 < 50 mm, p < 0.05
Fig. 1.
Concentration of uPAR in the serum of women with breast cancer
Fig. 2.
Concentration of uPAR in the serum of women with breast cancer in relation to stage of clinical advancement of the disease
Fig. 3.
Concentration of uPAR in the serum of women with breast cancer in relation to lymph node status
Fig. 4.
Concentration of uPAR in the serum of women with breast cancer in relation to tumour size
Discussion
The causes of the high coefficient of mortality in this disease are the lack of effective detection and diagnosis of this cancer, as well as the metastatic character of the disease [15]. At the time of diagnosis, around two thirds of patients already have metastases to the local lymph nodes and, in a considerable percentage of patients, there may also be micrometastases in remote organs. From the available data in the literature, it appears that a major factor in the formation of remote metastases is disturbance of the fibrinolytic system [16]. Substances produced by vascular endothelial cells and by tumour cells take part in this process [17]. An area of some interest, for many research centres, is the role of urokinase-type plasminogen activator (uPA) and its receptor in the process of metastasis in women with breast cancer [18]. So far, it has been shown that these substances are, above all, responsible for the conversion of plasminogen into plasmin. Plasmin is the main enzyme involved in the degradation of the vascular basement membranes, which facilitates migration and the adhesion of cancer cells to the surrounding tissues [17, 18]. Experimental work of recent years has brought information regarding the increased activity of uPA and uPAR in neoplastic tissues and in the bodily fluids of cancer patients [18, 19].
Our earlier studies showed increased uPA activity in women with breast cancer. It may be supposed that increased activity of uPA accelerates the processes of proliferation, migration and adhesion, not only in endothelial cells but also in tumour cells. Urokinase-type plasminogen activator takes its effects through binding with its specific uPAR, forming the uPA-uPAR complex which accelerates extracellular conversion of plasminogen into active plasmins. The enzyme directly catalyses the destruction of the basement membranes and cell matrices, including fibronectins, laminins, vitronectins and fibrins [18]. Increased production of plasmins also leads to activation of metalloproteinase, which, as the only enzyme involved in the processing of type IV collagen, is responsible for the formation of the skeleton of the vascular basement membranes. As a consequence of raised urokinase activity and increased plasmin production, there is increased degradation of the extracellular matrix surrounding the tumour, release of tumour cells from the primary tumour mass and their migration to the vessels. This makes it possible for tumour cells to invade remote organs [19]. The positive correlation between the activity of urokinase and the concentration of uPAR is a necessary condition for the process described above [20, 21]. The binding of uPA to the uPAR present on the surface of the tumour cells, thus forming the uPA-uPAR complex, is a condition for the formation of remote metastases.
In our study, we detected an increased level of uPAR in the serum of women with breast cancer, in comparison to the concentrations obtained from a control group.
In our group of 103 patients, 71 showed increased levels of uPAR. Similar observations were made by Witte et al., who found a statistically significant difference between the concentrations of uPAR in the plasma of breast cancer patients and the values for that receptor in a control group. Those authors also obtained raised results for the concentration of the uPA/uPAR complex and positive correlations between these parameters [22]. Similar findings were obtained by Risbro and colleagues, who simultaneously tested blood sera and homogenised breast cancer tissue [23]. Foekens and colleagues not only determined the concentrations of uPAR and uPA in the serum, but also demonstrated that high expression in homogenised tissues can be correlated with shortened survival and increased relapse rates [24]. From the available literature it may be concluded that expression of the uPAR is dependent on the presence of various cytokines, most of which are produced by Th1 lymphocytes. The cytokines interferon α (INF-α) and interleukin 2 (IL-2) increase the expression of uPAR and the activity of uPA, while the interleukins IL-4 and IL-13 increase the activity of urokinase and reduce the expression of the uPAR [25]. In their studies, Meng et al. observed high expression of uPAR in cancer tissues from the breast. Increased expression of the receptor was seen mainly in the outermost layers of the tumour, which, according to some authors, may be related to the presence of uPA on the surface of tumour cells [26]. The determination of disease stage is of particular importance in the prognosis of, and in selection of suitable treatments for, cancer patients. In our study we observed a relationship between the concentration of the uPAR and the stage of disease advancement. Disease stage, according to the TNM classification, rose in association with significantly raised uPAR levels in the serum of our group of breast cancer patients. We have found no results in the literature which relate the assessment of uPAR concentration in breast cancer patients to disease staging. Only Gong and co-workers, testing for uPAR in homogenised breast cancer tissue using an ELISA method, found a statistically significant relationship between the level of uPAR in women and stage (I or II) of clinical disease advancement [27]. Suzuki, using an in situ hybridization method, determined that expression of uPAR is increased in about 30% of cases of adenocarcinoma and in about 85% of cases of cancer of the large intestine; and that this increase in expression rises in line with increasing stage of advancement according to the Dukes scale [28]. Based on the findings of the study, that author also proposed that expression of the receptor was likely to be associated with the transformation of adenocarcinoma into invasive cancer [28]. In their experimental work, carried out on the serum of patients with multiple myeloma, Dmoszyńska and colleagues also noted high concentrations of uPAR. The results were significantly higher than those obtained from a control group. That study did not, however, confirm a relationship between the stage of disease advancement and the uPAR level, probably because of the small size of the studied group [29]. Another important prognostic factor in the survival of, and treatment selection for, patients with breast cancer, is the status of the axillary lymph nodes [30, 31]. Specialist oncologists believe that there is a good chance that patients whose disease is discovered sufficiently early, prior to the formation of metastases, can be permanently cured. The results of this study showed a statistically significant difference between levels of uPAR in patients with metastases to the lymph nodes and the level of the activator in patients without metastases. In their group of patients, Grondhal-Hansen obtained no statistically significant difference between levels of uPAR and the presence of metastases to the axillary lymph nodes [32]. Gong et al. made similar observations [27]. Kaneko's results, based on a study involving more than 100 patients with stomach cancer, showed that there was a positive relationship between the expression of the receptor and metastasis to the lymph nodes [33].
The analysis of our own results also included a comparison of serum uPAR concentrations to the degree of histological malignancy. We found no statistically significant differences between uPAR levels in patients with G1, G2 or G3 graded tumours. A lack of related findings in the literature meant that we were unable to compare our findings with those of other authors.
A significant prognostic parameter is the size of the tumour. The risk of disease progression and death rises in line with the size of the tumour. Small tumours are not, however, a reliable factor in a good prognosis, as even tumours measuring less than 10 mm can give rise to remote metastases. Our analysis showed that increasing tumour size goes hand in hand with increasing concentration of uPAR in the serum of women with breast cancer. We found statistically significant differences between the levels of uPAR in the control group, in patients with tumours measuring less than 20 mm, in patients whose tumours measured between 20 mm and 50 mm, and in those whose tumours measured greater than 50 mm. Little work has been carried out regarding the relationship between uPAR levels and tumour size, and so this parameter was also not compared with the findings of other researchers. On the basis of the available literature, we must accept that the plasminogen activation system plays an important role in the development of malignant tumours and the formation of metastases [34, 35]. The results of experimental studies, and of our own work, suggest that fibrinolysis may affect metastasis not only through the direct activation of plasmin, which is responsible for the degradation of vascular basement membranes and ECM, but also indirectly by the enzymatic activation of plasminogen [36, 37]. Among the main proteolytic enzymes are urokinase and tissue-type plasminogen activator (tPA). Earlier studies in our Laboratory Diagnostics Department showed raised levels of this activator in patients with breast cancer [38]. This enzyme not only directly takes part in the digestion of vascular basement membranes, but also activates metalloproteinases, thus facilitating the invasion of remote organs by cancer cells. It is presently believed that the binding of the uPAR, on the surface of tumour cells, to uPA, initiates an intracellular signalling cascade and plays an important role in the remodelling of the tissues surrounding the tumour and thus in the progression of the disease [38]. The formation of D-dimers is a result of the activation of the fibrinolytic system. In serum of patients with cancer an elevated concentration of this parameter has been observed. It is considered that determination of D-dimers is useful in the detection of latent intravascular activation of the coagulation system in patients with cancer [39, 40].
The relationship between tumour development and the activity of components of the fibrinolytic system gives hope that regulation of these processes may lead to new anti-cancer treatments [41]. Inhibition of the activities of the components of the fibrinolytic system is presently the subject of many studies.
In conclusion, increased levels of the uPAR was demonstrated in the serum of women with breast cancer. The level of this receptor was significantly higher in comparison to the level of uPAR in a control group. The presented results may indicate that increased activity of the fibrinolytic system and the action of its proteolytic components are involved in the formation of remote malignant metastases. It appears that the positive relationship between the concentration of the uPAR in women with breast cancer and advancing stage of disease may give us a valuable additional tool in the clinical assessment of women with this disease.
Acknowledgements
The authors would like to thank Professor Jan Bręborowicz of the Department of Tumour Pathology, Poznan University of Medical Sciences, for histopathological analyses, and Professor Sylwia Grodecka-Gazdecka of the Department of Oncological Surgery, Poznan University of Medical Sciences, for access to materials necessary for the study.
The authors declare no conflict of interests.
References
- 1.Sacewicz I, Wiktorska M, Wysocki T, Niewiarowska J. Mechanisms of cancer angiogenesis. Post Hig Med Dośw. 2009;63:159–68. [PubMed] [Google Scholar]
- 2.Fox SB, Generali DG, Harris AL. Breast tumour angiogenesis. Breast Cancer Res. 2007;9:216–27. doi: 10.1186/bcr1796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Andreasen PA, Egelund R, Petersen HH. The plasminogen activation system in tumor growth, invasion, and metastasis. Cell Mol Live Sci. 2000;57:25–40. doi: 10.1007/s000180050497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Skrzydlewska E, Sulkowska M, Koda M, Sulkowski S. Proteolytic-antiproteolytic balance and its regulation in carcinogenesis. World J Gastroenterol. 2005;11:1251–66. doi: 10.3748/wjg.v11.i9.1251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bernstein AM, Greenberg RS, Taliana L, Masur SK. Urokinase anchors uPAR to the actin cytoskeleton. Invest Ophthalmol Vis Sci. 2004;45:2967–77. doi: 10.1167/iovs.04-0030. [DOI] [PubMed] [Google Scholar]
- 6.Olson LJ, Yammani RD, Dahms NM, Kim JJ. Structure of uPAR, plasminogen, and sugar-binding sites of the 300 kDa mannose 6-phosphate receptor. EMBO J. 2004;23:2019–28. doi: 10.1038/sj.emboj.7600215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kroon ME, Koolwijk P, van Goor H, Weidle UH, Collen A, van der Pluijm G, van Hinsbergh VW. Role and localization of urokinase receptor in the formation of new microvascular structure in fibrin matrices. Am J Pathol. 1999;154:1731–42. doi: 10.1016/S0002-9440(10)65429-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Konno H, Abe J, Kaneko T, et al. Urokinase receptor and vascular endothelial growth factor are synergistycally associated with the liver metastasis of colorectal cancer. Jpn J Cancer Res. 2001;92:516–23. doi: 10.1111/j.1349-7006.2001.tb01124.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ganesh S, Sier CF, Heerding MM, et al. Prognostic value of the plasminogen activation system in patients with gastric carcinoma. Cancer. 1996;77:1035–43. doi: 10.1002/(sici)1097-0142(19960315)77:6<1035::aid-cncr5>3.0.co;2-g. [DOI] [PubMed] [Google Scholar]
- 10.Tecimer C, Doering DL, Goldsmith LJ, Meyer JS, Abdulhay G, Wittliff JL. Clinical relevance of urokinase-type plasminogen activator, its receptor, and its inhibitor type 1 in endometrial cancer. Gynecol Oncol. 2001;80:48–55. doi: 10.1006/gyno.2000.6015. [DOI] [PubMed] [Google Scholar]
- 11.Bottasso B, Mari D, Coppola R, Santoro N, Vaglini M, Mannucci PM. Hypercoagulability and hyperfibrynolisis in patients with melanoma. Thromb Res. 1996;8:345–52. doi: 10.1016/0049-3848(96)00006-0. [DOI] [PubMed] [Google Scholar]
- 12.Begum FD, Høgdall CK, Kjaer SK, et al. The prognostic value of plasma soluble urokinase plasminogen activator receptor (suPAR) levels in stage III ovarian cancer patients. Anticancer Res. 2004;24:1981–86. [PubMed] [Google Scholar]
- 13.Jakubiszyn E, Dzięgiel P, Zabel M. The plasminogen activation system in cell migration. Post Biol Kom. 2006;33:123–35. [Google Scholar]
- 14.Duffy MJ. The urokinase plasminogen activator system: role in malignancy. Curr Pharm Des. 2004;10:39–49. doi: 10.2174/1381612043453559. [DOI] [PubMed] [Google Scholar]
- 15.Autier P, Boniol M, La Vecchia C, Vatten L, Gavin A, Héry C, Heanue M. Disparities in breast cancer mortality trends between 30 European countries: retrospective trend analysis of WHO mortality database. BMJ. 2010;10:341–2. doi: 10.1136/bmj.c3620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Vogler EA, Siedlecki CA. Contact activation of blood-plasma coagulation. Biomaterials. 2009;30:1857–69. doi: 10.1016/j.biomaterials.2008.12.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Binder BR, Mihaly J, Prager GW. uPAR-uPA-PAI-1 interaction and signaling: a vascular biologists view. Thromb Haemost. 2007;97:336–42. [PubMed] [Google Scholar]
- 18.Watson T, Shantsila E, Lip GY. Mechanisms of thrombogenesis in atrial fibrillation: Virchow's triad revisited. Lancet. 2009;373:155–66. doi: 10.1016/S0140-6736(09)60040-4. [DOI] [PubMed] [Google Scholar]
- 19.Wang L, Madigan MC, Chen H, Liu F, Patterson KI, Beretov J, O'Brien PM, Li Y. Expression of urokinase plasminogen activator and its receptor in advanced epithelial ovarian cancer patients. Gynecol Oncol. 2009;114:265–72. doi: 10.1016/j.ygyno.2009.04.031. [DOI] [PubMed] [Google Scholar]
- 20.Hildenbrand R, Schaaf A, Dorn-Beineke A, Allgayer H, Sütterlin M, Marx A, Stroebel P. Tumor stroma is the predominant uPA, uPAR, PAI-1-expressing tissue in human breast cancer: prognostic impact. Histol Histopathol. 2009;24:869–77. doi: 10.14670/HH-24.869. [DOI] [PubMed] [Google Scholar]
- 21.Pedersen H, Brünner N, Francis D, Osterlind K, Rønne E, Hansen HH, Danø K, Grøndahl-Hansen J. Prognostic impact of urokinase, urokinase receptor and type 1 plasminogen activator inhibitor in squamous and large cell lung cancer tissue. Cancer Res. 1994;54:4671–5. [PubMed] [Google Scholar]
- 22.de Witte JH, Foekens JA, Brünner N, et al. Prognostic impact of urokinase-type plasminogen activator receptor (uPAR) in cytosols and pellet extracts derived from primary breast tumours. Br J Cancer. 2001;85:85–92. doi: 10.1054/bjoc.2001.1867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Riisbro R, Christensen IJ, Piironen T, et al. Prognostic significance of soluble urokinase plasminogen activator receptor in serum and cytosol of tumor tissue from patients with primary breast cancer. Clin Cancer Res. 2002;8:1132–41. [PubMed] [Google Scholar]
- 24.Foekens JA, Peters HA, Look MP, et al. The urokinase system of plasminogen activator an prognostic in 2780 breast cancer patients. Cancer Res. 2000;60:636–43. [PubMed] [Google Scholar]
- 25.Nykjaer A. The urokinase receptor: an activation antigen in T cells. Univ of Aarhus. 1995;1:100–10. [Google Scholar]
- 26.Meng S, Tripathy D, Shete S, et al. uPAR and HER-2 gene status in individual breast cancer from blood and tissues. Proc Natl Acad Sci U S A. 2006;103:17361–5. doi: 10.1073/pnas.0608113103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gong SJ, Rha SY, Chung HC, et al. Tissue urokinase-type plasminogen activator receptor leves in breast cancer. Int J Mol Med. 2000;6:301–5. [PubMed] [Google Scholar]
- 28.Suzuki S, Hayashi Y, Wang Y, et al. Urokinase type plasminogen activator receptor expression in colorectal neoplasms. Gut. 1998;43:798–805. doi: 10.1136/gut.43.6.798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Dmoszyńska A, Cioch M, Plesner T, et al. Correlation between plasma level of urokinase-type plasminogen activator, its receptor and prognostic markers in patients with multiple myeloma. Acta Haemat Pol. 2003;34:216–22. [Google Scholar]
- 30.Gottwald L, Spych M, Moszyńska-Zielińska M, Misiewicz P, Dukowicz A, Bibik R, Serbiak B, Fijuth J. Analiza kliniczna chorych z przerzutami raka piersi do osrodkowego ukladu nerwowego. Prz Menopauz. 2012;2:98–102. [Google Scholar]
- 31.Amir AS, Azar FP, Sahram N, et al. Prevalence of occult metastases in axillary sentinel lymph nodes of breast carcinoma. Pol J Pathol. 2012;1:40–4. [PubMed] [Google Scholar]
- 32.Grøndahl-Hansen J, Peters HA, van Putten WL, et al. Prognostic significance of the receptor for urokinase plasminogen activator in breast cancer. Clin Cancer Res. 1995;1:1079–87. [PubMed] [Google Scholar]
- 33.Kaneko T, Konno H, Baba M, Tanaka T, Nakamura S. Urokinase-type plasminogen activator expression correlates with tumor angiogenesis and poor outcome in gastric cancer. Cancer Sci. 2003;94:43–9. doi: 10.1111/j.1349-7006.2003.tb01350.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Dublin E, Hanby A, Patel NK, Liebman R, Barnes D. Immunohistochemical expression of uPA, uPAR, and PAI-1 in breast carcinoma. Am J Pathol. 2000;1:1219–27. doi: 10.1016/S0002-9440(10)64637-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Giannopoulou I, Mylona E, Kapranou A, Mavrommatis J, Markaki S, Zoumbouli Ch, Keramopoulos A, Nakopoulou L. The prognostic value of the topographic distribution of uPAR expression in invasive breast carcinomas. Cancer Lett. 2007;246:262–7. doi: 10.1016/j.canlet.2006.03.003. [DOI] [PubMed] [Google Scholar]
- 36.Guyton DP, Evans DM, Sloan-Stakleff KD. Urokinase plasminogen activator receptor (uPAR): a potential indicator of invasion for in situ breast cancer. Breast J. 2000;6:130–6. doi: 10.1046/j.1524-4741.2000.99025.x. [DOI] [PubMed] [Google Scholar]
- 37.Tang CH, Wei Y. The urokinase receptor and integrins in cancer progression. Cell Mol Life Sci. 2008;65:1916–32. doi: 10.1007/s00018-008-7573-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Thielemann A, Baszczuk A, Kopczyński Z, Szczepaniak M, Grodecka-Gazdecka S. The concentration of tissue-type plasminogen activator (t-PA) in patients with breast cancer. Diagn Lab. 2012;48:178–86. [Google Scholar]
- 39.Stanisławiak J, Markowska J. Thromboembolic complications in cancer. Contemp Oncol (Pozn) 2008;12:56–60. [Google Scholar]
- 40.Roszkowski K, Ziółkowska E. Fibrinolysis in neoplastic process. Contemp Oncol (Pozn) 2005;9:196–8. [Google Scholar]
- 41.Powroźnik B, Kubowicz P, Pękala E. Monoclonal antibodies in targeted therapy. Post Hig Med Dośw. 2012;66:663–73. doi: 10.5604/17322693.1009980. [DOI] [PubMed] [Google Scholar]