Abstract
Purpose
Currently, the diagnosis of pedicle screw (PS) loosening is based on a subjectively assessed halo sign, that is, a radiolucent line around the implant wider than 1 mm in plain radiographs. We aimed at development and validation of a quantitative method to diagnose PS loosening on radiographs.
Methods
Between 11/2004 and 1/2010 36 consecutive patients treated with thoraco-lumbar spine fusion with PS instrumentation without PS loosening were compared with 37 other patients who developed a clinically manifesting PS loosening. Three different angles were measured and compared regarding their capability to discriminate the loosened PS over the postoperative course. The inter-observer invariance was tested and a receiver operating characteristics curve analysis was performed.
Results
The angle measured between the PS axis and the cranial endplate was significantly different between the early and all later postoperative images. The Spearman correlation coefficient for the measurements of two observers at each postoperative time point ranged between 0.89 at 2 weeks to 0.94 at 2 months and 1 year postoperative. The angle change of 1.9° between immediate postoperative and 6-month postoperative was 75 % sensitive and 89 % specific for the identification of loosened screws (AUC = 0.82).
Discussion
The angle between the PS axis and the cranial endplate showed good ability to change in PS loosening. A change of this angle of at least 2° had a relatively high sensitivity and specificity to diagnose screw loosening.
Keywords: Pedicle screw loosening, Pedicle screw complication, Pedicle screw angle, Pedicle screw position, Posterior spine instrumentation
Introduction
Pedicle screws (PS) are often used for fixation in spine surgery. They are superior to other fixation techniques for a wide range of spine-related disorders in terms of providing mechanical strength [1]. In osteoporotic bone, however, PS fixation is a major challenge as the implant-bone interface is reduced [2] and remains a significant clinical problem with an overall instrumentation failure between 0.6 and 11 % [3–6]. Several reports have described PS loosening as a complication in spine surgery [4, 7–13]. There is a considerable variation in the reported loosening rates, probably because of the different study designs, different patient populations, and different definitions of loosening. Wu et al. [14] compared screw loosening in osteoporotic lumbar spine fusion between expandable and conventional PS. A significantly lower rate of screw loosening was seen for the expandable PS (4 %) compared with the conventional ones (13 %).
The histological mechanism of screw loosening was studied by Schatzker et al. [15]. According to the authors, movements of the bone screw results in fibrous tissue formation around the screw, which is then radiologically discernible as the so-called ‘halo’ sign.
Diagnosis of PS loosening is performed on plain radiographs and is based on the presence of the halo sign, which is a radiolucent line around the implant wider than 1 mm [13]. Loosening is subjectively diagnosed by a radiologist or spine surgeon. Sanden et al. [16] reported that a radiolucent zone around a PS is a good indicator of loosening. The plain radiographs and diagnosis of screw loosening, however, are often made after its clinical manifestation. Currently, no objective method of diagnosing PS loosening exists.
In the following study we aimed at development and validation of a quantitative method to assess PS loosening in posterior spine instrumentation on plain radiographs.
Materials and methods
The study was performed at the Department for Spine Surgery at the University Hospital of Bern and represents a retrospective analysis of plain radiographs of patients with and without radiological screw loosening. Since the study was based on a retrospective evaluation of anonymous data no approval of the responsible ethics committee was needed.
Patients
Thirty-seven patients who underwent a thoracic, thoraco-lumbar or lumbar spine fusion with PS instrumentation between November 2004 and January 2010 and developed a clinically manifesting PS loosening confirmed in the revision surgery were included into the “exposed” group. Thirty-six other consecutive patients from the same time period who underwent the same treatment procedure and who did not develop PS loosening, based on both radiological and clinical examination, were included into a “control” group.
The demographic and treatment characteristics are shown in Table 1. The male/female ratio in the exposed group was 34/6 in contrast to 25/11 in the control group and the average age was 67 and 65 years, respectively. The distributions of treated vertebrae were similar between the groups, located between Th4 and S1. Also, the proportions of vertebrae with the measured screws were similar between the groups (Table 1).
Table 1.
Demographic and treatment characteristics of the groups
| Exposed group | Control group | |
|---|---|---|
| N | 37 | 36 |
| Ø age | 67 | 65 |
| Age range | 53–91 | 46–82 |
| % females | 85 % | 69 % |
| N of fused segments on average | 4 | 3 |
| Th7 screw (%) | 0 (0) | 1 (1) |
| Th8 screw (%) | 1 (3) | 1 (1) |
| Th9 screw (%) | 1 (3) | 3 (4) |
| Th10 screw (%) | 4 (11) | 2 (3) |
| Th11 screw (%) | 0 (0) | 6 (8) |
| Th12 screw (%) | 5 (14) | 4 (6) |
| L1 screw (%) | 13 (35) | 13 (18) |
| L2 screw (%) | 6 (16) | 11 (15) |
| L3 screw (%) | 2 (5) | 11 (15) |
| L4 screw (%) | 3 (8) | 13 (18) |
| L5 screw (%) | 1 (3) | 5 (7) |
| S1 screw (%) | 2 (3) | 2 (3) |
Radiological measurements and statistical analyses
In a first step all measurements were performed by a single observer in lateral plain radiographs performed in a standing position. In the exposed group only the levels with loosened screws were considered and in the control group the cranial and caudal end-levels of the instrumentation were assessed as individual levels. Thus, 37 loose PSs from 37 exposed patients and 72 control screws from 36 control patients were measured (109 screw measurements in total).
Three different measurements were performed and compared regarding their capability to discriminate the loose PSs over the postoperative course. Following angles were measured: (1) the angle ε1 between the bisector of PS axes and the caudal endplate of the same vertebra; (2) the angle ε2 between the bisector of PS axes and the cranial endplate of the same vertebra (Fig. 1); (3) the angle ε3 between the bisector of PS axes and the rod axis. Furthermore, all three measurements were performed at four different postoperative timepoints: (a) early postoperative (on average 0.13 days postoperative), (b) 2-week postoperative (on average 16 days postoperative), (c) 2-month postoperative (on average 68 days), and (d) 1-year postoperative (on average 321 days). On each radiograph all three angles were measured.
Fig. 1.
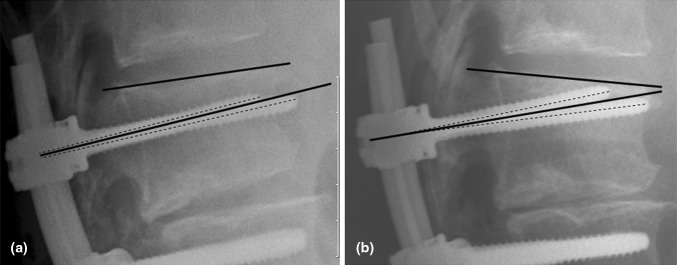
Standing lateral radiographs of L1 2 days (a) and 2 months (b) after posterior stabilization L1-S1 and early screw loosening in L1 (65-year-old female patient). For quantitative assessment the angle (ε2) between the cranial endplate (solid line) and the bisector (solid line) of the screw axis (dashed lines) was measured. The angle increased between the two follow-ups from 6.0° to 14.3°
It was hypothesized that at least one of the measurement methods should be able to discriminate a statistical difference in angle change between early and later postoperative images for loose screws. At the same time the same measurement method should not show any angle change between early and later postoperative images for the control screws. For the comparison between the angles of the loose and control screw Wilcoxon rank-sum test was used.
In a second step it was aimed to study the inter-observer invariance. Thereby the angle with the best discrimination capacity between the loose and control screw was applied for the same measurements by another observer, who was blinded to the findings. The inter-observer reliability regarding the preferred measurement method was assessed using the two-way random intra-class correlation method ICC(2,1). Furthermore, to assess the reliability of the two observers at different time points, Spearman coefficients for all measurement and average inter-observer discrepancy for each single measurement were calculated.
In a third step, a receiver operating characteristics (ROC) curve analysis was performed and the area under curve (AUC) was assessed to identify optimal cut-off values for the selected angle discriminating between patients with and without screw loosening. The sensitivity and specificity of the optimal cut-off values were calculated.
Nominal patient characteristics proportions between the groups were compared using the Chi-square test and ordinal variables using the Wilcoxon rank-sum test. Percentages are presented without decimal places, angles with one decimal place, and AUC, ICC, and Spearman coefficients with two decimal places. The α was set to 0.05 throughout the study. All statistical analyses were conducted using SAS 9.3 (SAS Institute, Inc., Cary, NC, USA).
Results
No significant differences between patient groups were observed for characteristics shown in Table 1.
A clear zone around the screw was observable in only six patients from the “exposed” group (16 %).
The ability of the measurement method to discriminate an angle change between early and later postoperative images is shown for loose and control screws in Table 2. It can be observed that the angle ε2, which was measured between the PS axis and the cranial endplate, was significantly different between the early and all later postoperative images. Neither the first angle ε1, measured between the PS axis and the caudal endplate, nor the third angle ε3, measured between the PS axis and the rod, was significantly changing between different timepoints for the loose or the control screws. At the same time, it can be seen that the ε2 angle changes were the smallest in the control screws, which is reflected in the highest non-significant p-values.
Table 2.
The ability of the three measurement methods to discriminate between angle changes between early and later postoperative images for loosened and control screws
| Angle difference between | Angle | Measurement method | Loosed screws | Control screws | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Early postop (SD) | Later postop (SD) | Mean change | p value | Early postop (SD) | Later postop (SD) | Mean change | p-value | |||
| Early postop vs. 2-week postop | ε1 | PS axis to the caudal endplate | 5.5 (4.8) | 7.7 (7.8) | −1.8 (4.5) | 0.12 | 4.1 (3.0) | 5.3 (6.2) | −0.4 (3.0) | 0.67 |
| ε 2 | PS axis to the cranial endplate | 5.3 (3.8) | 7.0 (6.3) | −2.4 (5.1) | 0.0401 | 4.1 (3.1) | 4.3 (3.6) | −0.1 (0.6) | 0.67 | |
| ε3 | PS axis and the rod axis | 90.4 (9.4) | 88.2 (11.5) | 1.2 (5.3) | 0.42 | 90.7 (4.7) | 89.2 (7.8) | −0.4 (1.9) | 0.32 | |
| Early postop vs. 2-month postop | ε1 | PS axis to the caudal endplate | 5.5 (4.8) | 8.5 (8.4) | −2.2 (6.0) | 0.13 | 4.1 (3.0) | 4.8 (5.7) | 0.0 (0.7) | 0.78 |
| ε 2 | PS axis to the cranial endplate | 5.3 (3.8) | 13.7 (14.2) | −9.6 (14.8) | 0.0003 | 4.1 (3.1) | 4.2 (3.5) | −0.2 (1.3) | 0.84 | |
| ε3 | PS axis and the rod axis | 90.4 (9.4) | 89.4 (13.3) | 0.5 (8.4) | 0.52 | 90.7 (4.7) | 88.9 (7.3) | 0.2 (1.7) | 0.88 | |
| Early postop vs. 1-year postop | ε1 | PS axis to the caudal endplate | 5.5 (4.8) | 6.5 (7.1) | −1.2 (6.2) | 0.45 | 4.1 (3.0) | 5.0 (5.6) | −0.2 (1.0) | 0.48 |
| ε 2 | PS axis to the cranial endplate | 5.3 (3.8) | 11.5 (7.7) | −8.2 (8.5) | 0.0003 | 4.1 (3.1) | 4.5 (3.6) | −0.5 (2.3) | 0.63 | |
| ε3 | PS axis and the rod axis | 90.4 (9.4) | 91.0 (10.3) | −1.7 (7.6) | 0.077 | 90.7 (4.7) | 89.0 (7.5) | 0.1 (2.0) | 0.29 | |
SD standard deviation. The significant p-values with the respective method are in bold
Based on this finding of good discrimination ability of the ε2 angle, the second, blinded observer repeated the measurement of this angle in all radiographs. The inter-observer reliability analysis showed ICC correlation coefficients of 0.45, 0.45, 0.42, and 0.55 for the measurement of ε2 in early postoperative, 2-week, 2-month, and 1-year postoperative radiographs, respectively. The measured ε2 for every postoperative timepoint are shown in Table 3. The Spearman correlation coefficient for the measurements of the two observers at each postoperative timepoint ranged between 0.89 for 2-week to 0.94 for 2-month and 1-year postoperative radiographs.
Table 3.
Average measured ε 2 for four postoperative timepoints and two observers with 95 % confidence intervals and ICC coefficient
| Average measured ε2 angle (95 % CI) | ||||
|---|---|---|---|---|
| Early postop | 2-week postop | 2-month postop | 1-year postop | |
| Observer 1 (°) | 5.2 (4.3–6.1) | 5.9 (4.9–7.0) | 7.8 (6.1–9.5) | 6.8 (5.6–8.0) |
| Observer 2 (°) | 4.9 (4.1–5.8) | 5.6 (4.6–6.6) | 7.8 (6.1–9.5) | 6.4 (5.3–7.6) |
| ICC coefficient | 0.45 | 0.45 | 0.42 | 0.55 |
| Average inter-observer discrepancy for each single measurement (°) | 0.1 (−0.2–0.4) | 0.1 (−0.2–0.5) | 0.0 (−0.3–0.3) | 0.3 (0.0–0.6) |
| Spearman correlation coefficient | 0.91 | 0.89 | 0.94 | 0.94 |
95 % CI 95 % confidence intervals
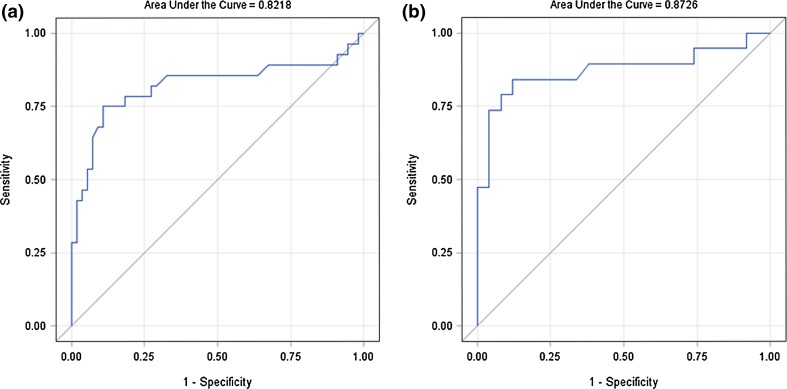
Based on the ROC analysis an ε2 angle change of at least 1.9° between immediate postoperative and 6 months after surgery resulted in a sensitivity of 75 % and specificity of 89 % for identification of loosened screws (Fig. 2a; AUC = 0.82). For the ε2 angle change between immediate postoperative and 1 year after surgery the optimal cut-off value was 2.0° with a sensitivity of 79 % and specificity of 92 % (Fig. 2b; AUC = 0.87).
Fig. 2.
ROC curve analysis for the identification of an optimal cut-off value in discrimination between loosened and control screw: a comparing immediate postoperative and 2-month postoperative images, b comparing immediate postoperative and 1-year postoperative images
Discussion
In the present study, three angles were selected and tested regarding their ability to show changes for loosened and control screws in the postoperative course. The angles ε1 and ε2 were similar, following the assumption that a loosened screw should change its position in relation to the cranial or caudal endplate. The idea behind angle ε3 was different, trying to estimate whether the screw-rod relation changes over time. The results have shown that the screw–rod relation remains practically the same. Despite the relatively high standard deviation of ε3 of around 10°, the maximum difference of ε3 observed between two different timepoints (91.0–88.2 = 2.8°) is negligible. In the postoperative course the average screw–rod angle remains around 90° in both control patients and those with a loosened screw.
Although, the mean angle change of around 2° was seen for ε1 angle at early and later postoperative timepoints for the loosened screws, this angle did also not change significantly. A clearly significant change was seen for the ε2 angle. The change of the relation between the bisector of the screw axes and the cranial endplate over the time was a clear indicator for a loosened PS. This angle measured in later postoperative images has considerably increased.
The small mean angle changes of ≤0.5° between baseline and all postoperative timepoints in the control group for all angles point to a good reproducibility of the measurements. On average slightly higher mean angle changes were observed in the group of loosened screws for all angles and all comparisons. However, ε2 angle measurements resulted in clearly higher (by factor >16) mean angle changes in loosened screws in comparison with the control screws. On the other hand, the mean angle changes between baseline and all postoperative timepoints for the ε3 angle, which was the angle-stable screw–rod fixation angle, were ≤1.7° in the loosened screws and ≤0.4° in the control group. This finding is another hint for a good reproducibility of the measurements. The still relatively high mean angle change of 1.7° for this angle in the loosened screws may potentially be caused by the change of the position of the unilateral loosened screw and therefore the change of the bisector-rod angle.
Interestingly, despite the ε2 and ε1 angles being related, only ε2 angle showed a clearly significant angle change. A probable explanation for this may be that the screws and the cranial endplate are closer to each other so that the influence of different X-ray beam projections is less relevant. Considering good reproducibility of the measurements of both angles, and, thus, exclusion of systematic measurement errors, ε2 can be regarded as superior to ε1 regarding the ability to change in loosened screws.
In a second step, a reproducibility and reliability of the angle measurement in comparison with the second observer blinded to the data was assessed. Very similar average angles were measured also by observer 2. The resulting intra-class correlation coefficients between 0.42 and 0.55 can be considered as moderate [17]. However, the differences between observers for the same measurement were very close to zero with the 95 % confidence intervals of around 0.6°. This finding together with the high Spearman correlation coefficients points to rather negligible differences between the observers.
In the measurements of control screws it was observed that practically for all angles and particularly for ε2 angle the differences between early and later postoperative images were around 0.2°–0.3° only. According to the ROC analysis, a change of the ε2 angle of 2° means a screw loosening with 75 % sensitivity and 89 % specificity at 2-month follow-up and with 79 % sensitivity, and 92 % specificity at 1-year follow-up.
In 2008, Tokuhashi et al. [18] studied the clinical course and significance of the clear zone around PSs. According to their results, the presence of clear zones did not necessarily mean pseudarthrosis. However, clear zones persisting for 2 years or longer after surgery represent a great risk of pseudarthrosis. Therefore, careful observation of clear zones around PSs is of great significance as an evaluation of bone union [18]. In our sample, however, only 16 % of cases with clear zones around PSs were observed. A change of the screw position in relation to the cranial endplate rather than just a clear zone around a screw should help in revealing patients with screw pseudarthrosis and clinical manifestation of screw loosening.
All the angles were measured in each radiograph. This was a necessary prerequisite for correct comparison of the angles. The influence of X-ray beam projection cannot be completely sorted out. To adjust for the X-ray beam projection in each measurement as well as to avoid mix-up with the anterior and posterior screws in sagittal X-ray projection, the bisector of the screw axes allowing also for an adjustment of the X-ray beam projection in each measurement was used. Figure 1 shows that the early postoperatively measured ε2 angle has increased at the next follow-up both if measured between the cranial endplate and the bisector of the screw axes as well as if measured between the cranial endplate and the better positioned screw. This allows the assumption that a unilaterally loosened screw should change the position of the second screw, as they both have an angle-stable fixation to the rod.
In summary, after a detailed literature search no quantitative method for the assessment of PS loosening was found. Our results show good ability to change of the angle between the PS axis and the cranial endplate in PS loosening. A change of this angle of at least 2° predicts screw loosening with a high sensitivity and specificity.
Conflict of interest
None.
References
- 1.Kothe R, Ruther W, Schneider E, Linke B. Biomechanical analysis of transpedicular screw fixation in the subaxial cervical spine. Spine. 2004;29:1869–1875. doi: 10.1097/01.brs.0000137287.67388.0b. [DOI] [PubMed] [Google Scholar]
- 2.Deckelmann S, Schwyn R, Van der Pol B, Windolf M, Heini PF, Benneker LM. DensiProbe spine: a novel instrument for intraoperative measurement of bone density in transpedicular screw fixation. Spine. 2010 doi: 10.1097/BRS.0b013e3181bc9470. [DOI] [PubMed] [Google Scholar]
- 3.Dickman CA, Fessler RG, MacMillan M, Haid RW. Transpedicular screw-rod fixation of the lumbar spine: operative technique and outcome in 104 cases. J Neurosurg. 1992;77:860–870. doi: 10.3171/jns.1992.77.6.0860. [DOI] [PubMed] [Google Scholar]
- 4.Esses SI, Sachs BL, Dreyzin V. Complications associated with the technique of pedicle screw fixation. A selected survey of ABS members. Spine. 1993;18:2231–2238. doi: 10.1097/00007632-199311000-00015. [DOI] [PubMed] [Google Scholar]
- 5.Okuyama K, Abe E, Suzuki T, Tamura Y, Chiba M, Sato K. Can insertional torque predict screw loosening and related failures? An in vivo study of pedicle screw fixation augmenting posterior lumbar interbody fusion. Spine. 2000;25:858–864. doi: 10.1097/00007632-200004010-00015. [DOI] [PubMed] [Google Scholar]
- 6.Wittenberg RH, Shea M, Swartz DE, Lee KS, White AA, 3rd, Hayes WC. Importance of bone mineral density in instrumented spine fusions. Spine. 1991;16:647–652. doi: 10.1097/00007632-199106000-00009. [DOI] [PubMed] [Google Scholar]
- 7.Nakashima H, Yukawa Y, Imagama S, Kanemura T, Kamiya M, Yanase M, Ito K, Machino M, Yoshida G, Ishikawa Y, Matsuyama Y, Ishiguro N, Kato F. Complications of cervical pedicle screw fixation for non-traumatic lesions: a multicenter study of 84 patients. J Neurosurg Spine. 2012;16:238–247. doi: 10.3171/2011.11.SPINE11102. [DOI] [PubMed] [Google Scholar]
- 8.Soini J, Laine T, Pohjolainen T, Hurri H, Alaranta H (1993) Spondylodesis augmented by transpedicular fixation in the treatment of olisthetic and degenerative conditions of the lumbar spine. Clin Orthop Relat Res pp 111–116 [PubMed]
- 9.McAfee PC, Weiland DJ, Carlow JJ. Survivorship analysis of pedicle spinal instrumentation. Spine. 1991;16:S422–S427. doi: 10.1097/00007632-199108001-00022. [DOI] [PubMed] [Google Scholar]
- 10.Yuan HA, Garfin SR, Dickman CA, Mardjetko SM. A historical cohort study of pedicle screw fixation in thoracic, lumbar, and sacral spinal fusions. Spine. 1994;19:2279S–2296S. doi: 10.1097/00007632-199410151-00005. [DOI] [PubMed] [Google Scholar]
- 11.Ohlin A, Karlsson M, Duppe H, Hasserius R, Redlund-Johnell I. Complications after transpedicular stabilization of the spine. A survivorship analysis of 163 cases. Spine. 1994;19:2774–2779. doi: 10.1097/00007632-199412150-00007. [DOI] [PubMed] [Google Scholar]
- 12.Pihlajamaki H, Myllynen P, Bostman O. Complications of transpedicular lumbosacral fixation for non-traumatic disorders. J Bone Jt Surg Br. 1997;79:183–189. doi: 10.1302/0301-620X.79B2.7224. [DOI] [PubMed] [Google Scholar]
- 13.Wu JC, Huang WC, Tsai HW, Ko CC, Wu CL, Tu TH, Cheng H. Pedicle screw loosening in dynamic stabilization: incidence, risk, and outcome in 126 patients. Neurosurg Focus. 2011;31:E9. doi: 10.3171/2011.7.FOCUS11125. [DOI] [PubMed] [Google Scholar]
- 14.Wu ZX, Gong FT, Liu L, Ma ZS, Zhang Y, Zhao X, Yang M, Lei W, Sang HX. A comparative study on screw loosening in osteoporotic lumbar spine fusion between expandable and conventional pedicle screws. Arch Orthop Trauma Surg. 2012;132:471–476. doi: 10.1007/s00402-011-1439-6. [DOI] [PubMed] [Google Scholar]
- 15.Schatzker J, Horne JG, Sumner-Smith G (1975) The effect of movement on the holding power of screws in bone. Clin Orthop Relat Res, pp 257–262 [DOI] [PubMed]
- 16.Sanden B, Olerud C, Petren-Mallmin M, Johansson C, Larsson S. The significance of radiolucent zones surrounding pedicle screws. Definition of screw loosening in spinal instrumentation. J Bone Jt Surg Br. 2004;86:457–461. doi: 10.1302/0301-620X.86B3.14323. [DOI] [PubMed] [Google Scholar]
- 17.StatTools (July 2012) http://www.stattools.net/ICC_Exp.php. StatTools
- 18.Tokuhashi Y, Matsuzaki H, Oda H, Uei H. Clinical course and significance of the clear zone around the pedicle screws in the lumbar degenerative disease. Spine. 2008;33:903–908. doi: 10.1097/BRS.0b013e31816b1eff. [DOI] [PubMed] [Google Scholar]