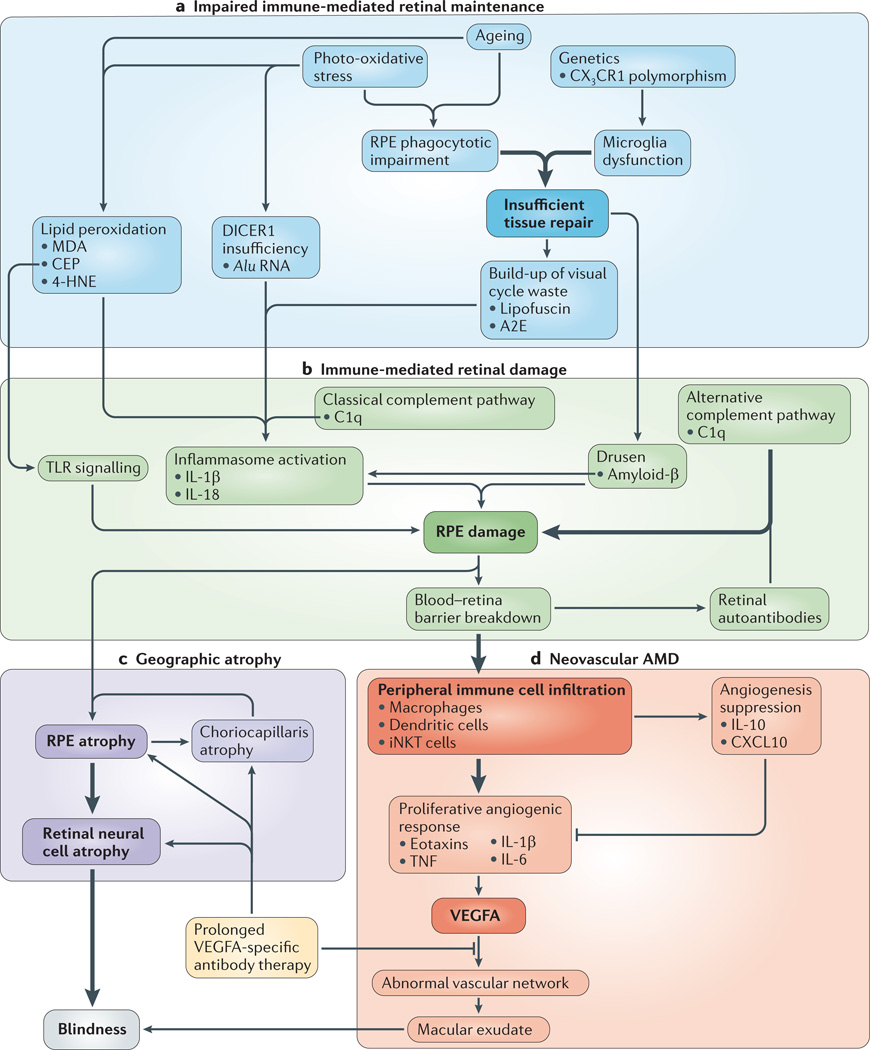
Figure 2. An integrated model of AMD pathogenesis.
The cell types, environmental factors and immune pathways that contribute to age-related macular degeneration (AMD) are categorized as either impaired immune-mediated retinal maintenance (part a) or immune-mediated retinal damage (part b). The combination of these factors leads to either geographic atrophy (part c) or neovascular AMD (part d). The most important pathways are highlighted in bold. The earliest known steps in AMD pathogenesis (part a) reflect a reduced capacity to manage the metabolic demands of the retina. The convergence of genetic, environmental and metabolic factors leads to a state in which the accumulation of toxic elements (such as lipid peroxidation by-products, lipofuscin and Alu RNAs) ultimately tips the balance towards immune activation. Once it is replete with unwanted waste material (part b), the retina is the target of inappropriate immune activation. The toxic contents of the retina induce inappropriate activation of diverse immune pathways, including classical and alternative complement pathways, the inflammasome and Toll-like receptor (TLR) signalling. Ultimately, the sustained activation of these pro-inflammatory and damaging pathways leads to advanced AMD. In the case of geographic atrophy (part c), sustained damage to the retinal pigmented epithelium (RPE) leads to the development of degeneration of the RPE, the choriocapillaris and, finally, neural retinal cells. In neovascular AMD (part d), breakdown of the blood–retinal barrier results in immune cell trafficking into the retina, which drives vascular endothelial growth factor A (VEGFA)-dependent neovascularization, causing blindness. 4-HNE, 4-hydroxynonenal; A2E, N-retinyl-N-retinylidene ethanolamine; C1q, complement component 1q; CEP, carboxyethylpyrrole; CX3CR1, CX3C-chemokine receptor 1; CXCL10, CXC-chemokine ligand 10; IL, interleukin; iNKT, invariant natural killer T; MDA, malondialdehyde; TNF, tumour necrosis factor.