Abstract
Alcoholism results in about 2.5 million deaths annually worldwide, representing 4% of all mortality. Although alcoholism is associated with more than 60 diseases, most mortality from alcoholism results from alcoholic liver disease (ALD). ALD includes alcoholic steatosis, alcoholic hepatitis, and alcoholic cirrhosis, in order of increasing severity. Important scoring systems of ALD severity include: Child-Pugh, a semi-quantitative scoring system useful to roughly characterize clinical severity; model for end-stage liver disease, a quantitative, objective scoring system used for prognostication and prioritization for liver transplantation; and discriminant function, used to determine whether to administer corticosteroids for alcoholic hepatitis. Abstinence is the cornerstone of ALD therapy. Psychotherapies, including twelve-step facilitation therapy, cognitive-behavioral therapy, and motivational enhancement therapy, help support abstinence. Disulfiram decreases alcohol consumption by causing unpleasant sensations after drinking alcohol from accumulation of acetaldehyde in serum, but disulfiram can be hepatotoxic. Adjunctive pharmacotherapies to reduce alcohol consumption include naltrexone, acamprosate, and baclofen. Nutritional therapy helps reverse muscle wasting, weight loss, vitamin deficiencies, and trace element deficiencies associated with ALD. Although reduced protein intake was previously recommended for advanced ALD to prevent hepatic encephalopathy, a diet containing 1.2-1.5 g of protein/kg per day is currently recommended to prevent muscle wasting. Corticosteroids are first-line therapy for severe alcoholic hepatitis (discriminant function ≥ 32), but proof of their efficacy in decreasing mortality remains elusive. Pentoxifylline is an alternative therapy. Complications of advanced ALD include ascites, spontaneous bacterial peritonitis, esophageal variceal bleeding, hepatic encephalopathy, hepatorenal syndrome, hepatopulmonary syndrome, and portopulmonary hypertension. Alcoholic cirrhotics have increased risk of developing hepatomas. Liver transplantation is the ultimate therapy for severe ALD, but generally requires 6 mo of proven abstinence for eligibility. Alcoholic cirrhotics who maintain abstinence generally have a relatively favorable prognosis after liver transplantation.
Keywords: Alcoholic liver disease, Alcoholic steatosis, Alcoholic hepatitis, Alcoholic cirrhosis, Alcoholism, Liver disease, Corticosteroids, Pentoxifylline, Liver transplantation
Core tip: Alcoholism results in about 2.5 million deaths annually worldwide, representing 4% of all mortality. Most of this mortality is from alcoholic liver disease (ALD). ALD includes alcoholic steatosis, alcoholic hepatitis, and alcoholic cirrhosis, in order of increasing severity. This work reviews this clinically important subject, with a focus on informing clinicians of recent advances in therapy to reduce the currently high mortality from alcoholic hepatitis and alcoholic cirrhosis.
INTRODUCTION
Alcoholism results in an estimated 2.5 million deaths annually worldwide, representing 4% of all mortality[1]. This mortality is much greater than that caused by acquired immunodeficiency syndrome (AIDS) or tuberculosis[1]. It is the leading risk factor for mortality for ages 15-59 in males, and the eighth leading risk factor for mortality for all ages in both sexes[1]. Alcoholism is associated with more than 60 diseases, and is commonly associated with accidental injuries, including motor vehicle injuries[1]. Alcoholic liver disease (ALD), moreover, accounts for 40% of mortality from cirrhosis[2]. Annual mortality for ALD is 4.4 per 100000 in the general population, compared to 2.9 per 100000 for hepatitis C virus (HCV)[3].
Alcoholism, or alcohol use disorder, is defined, according to the Diagnostic and Statistical Manual of Mental Disorders, 5th edition (DSM-5), as a problematic pattern of alcohol use leading to clinically significant impairment or psychological distress[4]. Development of ALD is dose-dependent, and drinking ≥ 30 g/d of alcohol (“standard” drink: contains 0.6 fluid ounces or 14 g “pure” alcohol[5] increases the risk of ALD in both sexes[6]). Women have a greater risk of ALD than men, likely secondary to differences in ethanol metabolism[7-13]. For example, one study reported the threshold level of alcohol intake for developing ALD is 12-22 g/d in women vs 24-46 g/d in men[7]. Many alcoholic patients, however, do not develop clinically significant ALD[14]. Genetic and environmental factors are important, but the specific genes or environmental factors that predispose to ALD are poorly understood[14]. Potentiating factors for ALD include metabolic syndrome[13,15], diabetes[16,17], obesity[17,18], smoking[13,15], iron overload[12,13,17,19], and chronic viral hepatitis B or C[12,13,20,21].
The only definitive treatment for ALD is liver transplantation (LT). Abstinence is critical, but usually cannot reverse advanced ALD. Supportive therapy and nutritional management are also important. Several medical therapies have been studied, including corticosteroids and pentoxifylline, but no medical therapy has been proven to improve survival. This review discusses the spectrum of ALD; reviews the classification of severity and prognostic criteria for ALD; analyzes the current therapies for ALD, including abstinence, nutritional therapy, drugs, and LT; discusses the controversies regarding survival benefits for individual therapies; and reports professional society guidelines for management of cirrhosis and its complications.
SPECTRUM OF ALD
ALD is classified into alcoholic fatty liver (steatosis), alcoholic hepatitis (AH; steatohepatitis), and alcoholic cirrhosis. About 90% of alcoholics develop alcoholic steatosis, about 25% develop alcoholic hepatitis, about 15% develop alcoholic cirrhosis, and about 10% develop hepatocellular carcinoma[13,22-24]. Alcoholic steatosis, the earliest manifestation of ALD, is pathologically characterized by microvesicular and macrovesicular fat accumulation within hepatocytes, minimal inflammatory reaction, and no hepatic fibrosis[23]. It is often reversible with abstinence[25]. Patients are often asymptomatic, and the diagnosis is usually incidental. They do not exhibit stigmata of chronic liver disease, such as spider angiomata and palmar erythema. Patients typically present with mild elevations of liver enzymes, including gamma-glutamyl transpeptidase (GGT), aspartate aminotransferase (AST), and alanine aminotransferase (ALT) levels[25]. The serum bilirubin level and liver synthetic function [international normalized ratio (INR), albumin level] tend to be normal.
AH is an inflammatory process with predominantly neutrophilic infiltration, characterized by ballooning degeneration of hepatocytes, hepatocyte necrosis, steatosis, and presence of Mallory bodies (homogeneous, eosinophilic cytoplasmic perinuclear inclusions) within hepatocytes[23] (Figure 1A). Clinical findings include jaundice, pyrexia, unintentional weight loss, malnutrition, and tender, enlarged liver[26]. Patients typically present with moderate elevations in AST (usually < 300 IU/L), ALT, GGT, and serum bilirubin[25]. An AST:ALT ratio of ≥ 2:1 is strongly suggestive of ALD[27], likely from up-regulated mitochondrial AST molecular expression and synthesis by alcohol[28]. AH may be complicated by ascites, encephalopathy, or gastrointestinal (GI) bleeding from esophageal varices or portal gastropathy[26]. Imaging may show hepatomegaly, but this finding is nonspecific, and imaging is generally performed to identify radiologic evidence of cirrhosis, to identify its complications, and to exclude focal hepatic lesions[25,29]. Definitive diagnosis is by liver biopsy, but this is rarely necessary in clinical practice.
Figure 1.
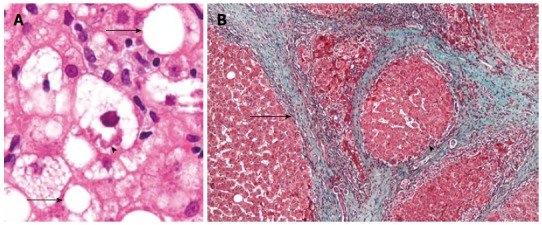
Photomicrograph. A: Photomicrograph showing a Mallory body (arrowhead), with twisted rope-like appearance, and fat vacuoles (arrows) as seen in alcoholic steatohepatitis (image from http://en.wikipedia.org/wiki/Alcoholic_hepatitis, licensed under Creative Commons Attribution-Share Alike 3.0 Unported); B: Photomicrograph showing a regenerating nodule (arrowhead) and bridging fibrosis (arrow) as seen in alcoholic cirrhosis (image from http://en.wikipedia.org/wiki/Alcoholic_cirrhosis, licensed under Creative Commons Attribution-Share Alike 3.0 Unported).
Alcoholic cirrhosis is pathologically characterized by severely disorganized liver architecture, with both bridging fibrosis and regenerating nodules, that are typically uniformly-sized and micronodular[23] (Figure 1B). Patients usually present with stigmata of chronic liver disease, including gynecomastia, palmar erythema, spider angiomata, testicular atrophy, and parotid gland enlargement; and signs of portal hypertension, including caput medusa. Dupuytren’s contracture is often present in patients with alcoholic cirrhosis[30]. Alcoholic cirrhosis is associated with multiple complications, as discussed below. Laboratory findings often include hypoalbuminemia, hyperbilirubinemia, thrombocytopenia, and prolonged prothrombin time (PT) and increased INR[26]. These abnormalities typically worsen with progression of cirrhosis. Imaging studies often demonstrate findings consistent with cirrhosis, including a small, shrunken liver, hepatic nodularity, abnormal tortuous vessels from intra-abdominal varices, and other abnormalities, such as ascites or focal hepatic lesions[25,31]. These findings assist in diagnosing cirrhosis, but cannot, by themselves, establish alcohol as the etiology[26,32]. Magnetic resonance imaging (MRI) findings suggestive of alcoholic cirrhosis include caudate lobe enlargement, presence of the right posterior hepatic notch, and smaller regenerative nodules (micronodular) than in other etiologies of cirrhosis[31]. Alcoholic cirrhosis is diagnosed by history of excessive alcohol intake, with exclusion of other causes of cirrhosis (Table 1)[33-36]. The evolution of alcoholic fatty liver to alcoholic hepatitis to alcoholic cirrhosis is usually progressive with continued alcohol use, but different stages can occur simultaneously in one patient (e.g., AH with alcoholic cirrhosis).
Table 1.
Differential diagnosis of cirrhosis, excluding alcoholic cirrhosis1
| Diseases | Diagnostic studies | Liver biopsy |
| Wilson’s disease | Serum ceruloplasmin < 20 mg/dL; 24-h urine copper excretion > 100 μg/24 h; slit-lamp ophthalmologic examination for Kayser-Fleischer rings | Steatosis; glycogenated nuclei in hepatocytes; focal hepatocellular necrosis, fibrosis, and ultimately, cirrhosis, usually macronodular[34]; copper retention in hepatocytes; hepatic copper concentration > 250 μg/g dry weight |
| Hemochromatosis | Serum transferrin-iron saturation > 45%; serum ferritin typically > 1000 μg/L; genotyping for detection of HFE mutations: C282Y and H63D; non-contrast CT of liver demonstrates attenuation values of > 70 HU[36] | Grade 4 stainable iron in hepatocytes, with periportal distribution and sparing of Kupffer cells; hepatic iron concentration > 80 μmol/g dry weight; hepatic iron index > 1.9 |
| Hepatitis C | Anti-HCV; HCV RNA in patients who test positive for HCV antibody | Triad of histological findings with acute infection: lymphoid aggregates in portal tracts, epithelial damage of small bile ducts, and prominent microvesicular and macrovesicular steatosis; chronic infection: periportal necrosis, intralobular necrosis, portal inflammation, and fibrosis; no characteristic pathognomonic features |
| Chronic hepatitis B | HBsAg; serum level of HBV DNA > 2000-20000 IU/mL | Acute infection: lobular disarray, ballooning degeneration, numerous apoptotic (Councilman) bodies, Kupffer cell activation, and lymphocyte-predominant lobular and portal inflammation; chronic infection: varying degree of predominantly lymphocytic portal inflammation with interface hepatitis and spotty lobular inflammation[34]; presence of HBcAg staining in the liver |
| Autoimmune hepatitis | Antinuclear antibody (ANA); smooth muscle antibody (SMA); antibodies to liver and kidney microsomes (anti-LKM1); anti-soluble liver antigen (anti-SLA); asialoglycoprotein receptor antibodies | Interface hepatitis at junction of portal region and liver lobule; lobular hepatitis with lymphocytoplasmacytic infiltration; intrahepatic bile ducts generally appear normal |
| α1-antitrypsin deficiency | Serum α1-antitrypsin genotype or phenotype (homozygous PiZZ or heterozygous PiSZ phenotype) | Giant-cell hepatitis with multinucleated giant cells; lobular disarray; cellular and canalicular cholestasis; neoductular proliferation; bridging hepatic fibrosis; PAS-positive and diastase-resistant cytoplasmic granules in periportal hepatocytes |
| Primary biliary cirrhosis | Antimitochondrial antibodies (AMA) ≥ 1: 80 titer; ANA, with immunofluorescence typically revealing speckled, homogeneous, nuclear dot, centromere, or rim-like patterns | Focal and segmental nonsuppurative cholangitis; “florid duct lesion”: bile duct surrounded by intense lymphocytic or granulomatous infiltrate with basal integrity of the bile duct breached by individual lymphocytes; granulomas in close proximity to bile duct; bile ductular proliferation (cholangioles or pseudoducts) along periphery of portal tract |
| Non alcoholic fatty liver disease | Diagnosis of exclusion, correlated with: metabolic syndrome: diabetes mellitus, hypertension, hyperlipidemia, abdominal obesity with waist circumference > 102 cm for men and > 88 cm for women; obesity (BMI ≥ 30 kg/m2); obstructive sleep apnea; sedentary lifestyle | Macrovesicular steatosis; early hepatocyte inflammation, predominantly neutrophilic; late nondescript fibrosis and cirrhosis |
1Patients may have more than one disease contributing to cirrhosis (e.g., alcoholism and iron overload, or alcoholism and hepatitis C). HFE: Human hemochromatosis protein; CT: Computed tomography; HU: Hounsfield units; HCV: Hepatitis C virus; HBsAg: Hepatitis B surface antigen; HBV: Hepatitis B virus; DNA: Deoxyribonucleic acid; HBcAg: Hepatitis B core antigen; PAS: Periodic acid-Schiff; BMI: Body mass index.
PROGNOSTIC CRITERIA AND MONITORS OF DISEASE SEVERITY
Several scoring systems assess severity of liver disease and predict patient survival. Child-Turcotte-Pugh (CTP) score, the oldest scoring system, uses serum bilirubin level, albumin level, PT, severity of ascites, and severity of encephalopathy[37]. Patients are categorized as: class A = scores 1-6, class B = scores 7-9, and class C = scores 10-15; the higher the score, the worse the disease[37,38]. Although heuristically useful, CTP scores are limited by subjectivity in grading and by use of PT instead of the more accurate INR[39]. It was previously used to prioritize candidates for LT, but was supplanted in 2002 by the more quantitative and less subjective model for end-stage liver disease (MELD) score[40]. MELD score was originally developed to assess short-term prognosis in cirrhotic patients undergoing transjugular intrahepatic portosystemic shunt (TIPS), but was found to also reliably estimate short-term survival in patients with any type of chronic liver disease[41-43]. MELD score includes serum bilirubin level, creatinine level, and INR[42]. It can be calculated on-line at a free website[44]. The United Network for Organ Sharing (UNOS) uses MELD score to prioritize LT candidates because it relatively accurately predicts 3-mo mortality in patients awaiting LT[39,40]. Recently, addition of serum sodium concentration (MELD-Na score) has been proposed to more accurately predict mortality in patients awaiting transplant[45,46]. The MELD-Na score, if used for liver allocation, can avert an additional 7% mortality in patients awaiting LT[45]. It is not yet widely used, but is a promising scoring system that may better predict mortality and improve donor liver allocation.
While CTP and MELD scores are applicable to all etiologies of cirrhosis, other scoring systems are specific for ALD. Discriminant function (DF), which includes only PT and serum bilirubin, is used to predict early mortality in AH patients and to objectively select AH patients likely to benefit from corticosteroid therapy[47,48]. DF < 32 is classified as non-severe AH, with 10% mortality, whereas DF ≥ 32 is classified as severe AH, with mortality ranging from 30%-60% without treatment[48-55]. Glasgow alcoholic hepatitis score (GAHS) is calculated as the sum of scores for the following individual parameters: age, leukocyte count, serum urea level, PT ratio (ratio of patient-to-control PT), and serum bilirubin level[56]. A score > 8 predicts poor prognosis[56]. ABIC, the most recent scoring system, includes age, serum bilirubin, INR, and serum creatinine[57]. It stratifies risk of mortality from AH as low (score < 6.71), intermediate (score: 6.71-8.99), and high (score ≥ 9.0), with 90 d mortality at 0%, 30%, and 75%, respectively (P < 0.0001)[57]. These last two scoring systems are promising prognostic indicators and treatment guides, but are currently rarely used clinically.
Lille score includes 6 variables: age, albumin level, bilirubin level at day 0, bilirubin level at day 7, PT, and presence of renal insufficiency[58]. It helps stratify patients with AH. It may be more accurate than other scoring systems, but is mostly used to predict 6-mo survival in patients with AH treated with corticosteroids[59]. It predicts about 75% of observed 6-mo mortality[59]. A score < 0.45 predicts 15% mortality, whereas a score ≥ 0.45 predicts 75% mortality (P < 0.0001)[59]. Alternative therapies should be considered when the score is ≥ 0.45 at day 7 of corticosteroid therapy[59].
THERAPY
Abstinence supportive therapies for abstinence
Abstinence is the cornerstone of therapy. It markedly reduces mortality[60-64]. However, this benefit may not become statistically significant until at least ≥ 1.5 years of abstinence[65]. Five-year mortality for patients with alcoholic cirrhosis who cease drinking decreases to 10%, compared to 30% for patients who continue to drink[22]. Alcohol consumption increases portal pressure and increases porto-collateral blood flow in cirrhotic patients[66]. Even moderate alcohol consumption significantly worsens hepatic hemodynamics[66]. Abstinence results in a decreased rate of rebleeding after acute variceal bleeding [hazard ratio (HR) 0.26, P = 0.002][64]. Abstinence may also decrease hepatic fibrosis, as measured by transient elastography, a noninvasive measure of liver stiffness[67-69]. Liver transplant programs in the United States generally mandate abstinence for ≥ 6 mo for eligibility for LT[70]. Therefore, strict, long-term abstinence is essential, and physicians should be vigilant for relapses and aggressively intervene in such cases.
Psychotherapies promoting abstinence include twelve-step facilitation therapy (TSF), cognitive-behavioral therapy (CBT), and motivational enhancement therapy (MET)[71]. TSF assumes that alcoholism is a progressive illness for which the only effective remedy is abstinence[72]. It provides a structured program to facilitate active involvement in alcoholics anonymous (AA)[72]. TSF emphasizes the twelve spiritual principles (traditions) of AA, including the first five critical principles focusing on acceptance, surrender, and moral inventories[72]. In “acceptance” patients accept they have a drinking problem. In “surrender” patients accept faith in a “Higher Power” and follow the AA path[72]. CBT identifies “high-risk” situations that increase the risk of alcoholism and encourages patients to assume responsibility and acquire self-control skills to prevent relapse[73]. It consists of 12 sessions to train clients to adopt active behavioral and cognitive methods, rather than alcohol, as coping mechanisms during “high-risk” situations[73]. Lastly, MET employs motivational psychology to produce internally motivated change, i.e., employs strategies to mobilize patient’s internal resources for change, rather than continuous external guidance[74]. A large RCT, incorporating 1726 patients, showed all three of these psychotherapies were beneficial and all produced roughly equivalent outcomes[71].
Disulfiram, naltrexone, acamprosate, and baclofen are used to treat alcohol dependence. Disulfiram (Antabuse), an acetaldehyde dehydrogenase inhibitor, alters alcohol metabolism to cause accumulation of serum acetaldehyde, which produces unpleasant sensations of nausea, vomiting, flushing, light-headedness, abdominal pain, and tachycardia[75]. Such unpleasant sensations provide negative reinforcement for ethanol ingestion[75]. However, disulfiram-related hepatotoxicity may result in up to 16% mortality[76], and it must be cautiously administered in patients with ALD. Naltrexone, a mu, kappa, and delta opioid receptor antagonist, decreases alcohol craving by blocking the central pleasurable effects of alcohol. It effectively decreases alcohol intake and prevents relapse[77,78]. A Cochrane meta-analysis reported that naltrexone reduced heavy alcohol consumption by 83%[77]. An extended-release, injectable formulation of naltrexone was reported to improve quality of life, including mental health, social functioning, general health, and physical functioning[79]. It produces relatively mild side effects, mainly nausea, abdominal pain, anorexia, and mild-to-moderate sedation, but is rarely hepatotoxic[77,78,80].
Acamprosate also helps decrease alcohol dependence. It decreases the rate of relapse and helps maintain abstinence[81-85]. Its mechanism of action is unknown[81]. It improves life expectancy and reduces lifetime medical costs in alcoholic patients[86]. It has a favorable safety profile. Diarrhea is the most frequent side effect[81,83]. Baclofen, a gamma-aminobutyric acid-B agonist, is a new, promising, adjuvant treatment for alcohol dependence. It helps alcoholic patients suppress alcohol craving, reduce alcohol intake, and achieve and maintain abstinence[87-90]. It also improves liver function parameters, including serum ALT, bilirubin, GGT, and albumin levels, and INR[88]. These favorable effects occur in alcoholic patients with cirrhosis, with or without concomitant HCV infection[88,90]. Most affirmative studies have been performed in Europe, but a large, randomized controlled trial (RCT) performed in the United States suggested that baclofen is not superior to placebo in treating alcohol dependence[91]. Baclofen produces minimal side effects and has no apparent hepatotoxicity[87-91], rendering it safe in patients with ALD. For all these aforementioned drugs, there are limited data on efficacy in patients with advanced liver disease. Psychotherapy and family support are essential components in the overall management of alcoholics with liver disease.
Nutritional therapy
Muscle wasting, weight loss, and nutritional deficiencies commonly occur in patients with ALD. These abnormalities are associated with increased morbidity and mortality[92,93]. The etiology of weight loss and malnutrition is multifactorial, including poor dietary intake from anorexia, altered sense of taste and smell, and nausea and vomiting; malabsorption; hypermetabolic state; and impaired protein synthesis from cytokine-induced inflammatory responses[92-95]. Nutritional deficiencies can include fat-soluble vitamins (A, D, E and K), folate, thiamine, niacin, and pyridoxine; and the trace elements zinc, magnesium, and selenium[92]. Each deficiency produces specific symptoms, signs, and complications[92]. For example, thiamine deficiency causes Wernicke’s encephalopathy.
The European Society for Clinical Nutrition and Metabolism (ESPEN) recommends enteral or parenteral nutritional support for patients with liver disease to improve nutritional status, liver function, mental status, and overall survival[96,97]. Nutritional support also reduces the incidence of complications after LT[96,97]. However, a recent Cochrane review of 37 RCTs found no significant difference in mortality in patients with advanced liver disease receiving either enteral or parenteral nutritional support vs those receiving neither[95]. The investigators did, however, note improvement in serum bilirubin level, nitrogen balance, and hepatic encephalopathy; and reduced incidence of post-operative complications, particularly infections. The reviewed RCTs generally had methodological flaws, which could have caused overestimation of the observed effects[95]. The American Association for the Study of Liver Diseases (AASLD) and American College of Gastroenterology (ACG) recommend regular assessment of patients for nutritional, vitamin, and mineral deficiencies; appropriate supplementation for identified deficiencies; enteral nutritional therapy for severe ALD; and frequent interval feedings, emphasizing breakfast and a nighttime snack[32]. The diet should include 1.2-1.5 g of protein/kg per day and 35-40 kcal/kg per day to improve nitrogen balance[32]. These recommendations revise prior recommendations to reduce protein intake to prevent hepatic encephalopathy, in order to maintain positive protein balance and prevent muscle wasting in cirrhotics[98].
Therapies for alcoholic hepatitis
Although nutritional and supportive management are important, the mainstay of therapy for AH remains alcohol abstinence. Treatment varies according to severity. Patients who have DF < 32 have only 10% 28 d mortality without treatment[55]. Supportive management is adequate for such patients. However, patients who have DF ≥ 32 have mortality between 30%-60% without treatment[48-54], and treatment may be lifesaving in this population.
Treatment options for severe AH include corticosteroids and pentoxifylline, which are well established, albeit controversial, therapies. Other treatment options, including infliximab, etanercept, antioxidants, and complementary medicines have not been shown to improve clinical outcome[24].
Corticosteroids: Corticosteroids are the oldest and most investigated pharmacologic therapy for severe AH. Several RCTs have been performed with contradictory results[48-54]. Ramond et al[49] reported 12.5% mortality among patients receiving prednisolone vs 55% mortality among patients receiving placebo (P = 0.001). Contrariwise, a large study of 178 patients by Mendenhall et al[50] reported no statistically significant difference in mortality among patients treated with corticosteroids vs placebo. Both studies had limited statistical power because of small-to-moderate study size. Several investigators performed meta-analyses of the numerous RCTs to increase statistical power[55,99-102]. Three of these meta-analyses showed improvement in short-term survival in AH patients receiving corticosteroid treatment[55,99,102], whereas two meta-analyses showed no improvement[100,101] (Table 2). For example, a Cochrane meta-analysis incorporating 721 randomized patients demonstrated no statistically significant improvement in mortality among AH patients treated with corticosteroids; however, a subgroup analysis performed on low-bias risk trials revealed significantly reduced mortality in corticosteroid-treated patients with either DF ≥ 32 or hepatic encephalopathy (RR = 0.33, 95%CI: 0.11-0.97)[100]. One affirmative meta-analysis performed individual patient data meta-analysis, considered the gold standard for meta-analysis with the least bias[103]; it showed that AH patients receiving corticosteroids had a 28-d mortality of only 20% vs 34% for controls (P = 0.0005)[99]. Furthermore, a prior meta-analysis demonstrated the importance of corticosteroid therapy in AH patients, showing that the number needed to treat (NNT) with corticosteroids to prevent one death was only five[55]. Additionally, corticosteroids, specifically prednisolone, have been shown to significantly reduce mortality for at least 1 year[104].
Table 2.
Meta-analyses of randomized controlled trials of corticosteroid therapy vs placebo for severe alcoholic hepatitis
| Ref. | Inclusion criteria | Number of RCTs (total number of patients) | Endpoint parameters (primary endpoint listed on first line of each entry) | RR, HR or OR for primary endpoint | 95%CI | Comments |
| Imperiale et al[102], 1990 | RCTs of patients with acute AH receiving corticosteroids vs placebo | 11 (562) | Mortality Hepatic encephalopathy | RR = 0.63 | 0.5-0.8 | Positive study (P = 0.025) |
| Christensen et al[101], 1995 | RCTs evaluating short term effect on survival of treatment with glucocorticoids vs placebo for AH | 13 (659) | Mortality Age Serum bilirubin Ascites Male gender Hepatic encephalopathy | RR = 0.78 | 0.51-1.18 | Negative study (P = 0.2) |
| Mathurin et al[55], 2002 | RCTs during 1984-1992 of patients receiving glucocorticoids vs placebo | 3 (215) | Survival Age Liver function tests DF Hepatic encephalopathy Gender Serum creatinine Ascites Leukocyte count | OR = 0.39 | 0.22-0.71 | Positive study (P = 0.002) Used individual patient data analysis to increase statistical rigor for the meta-analysis |
| Rambaldi et al[100], 2008 | RCTs of patients with severe, clinically overt AH diagnosed by clinical and biochemical criteria, treated with glucocorticoids vs placebo (or no intervention) | 15 (721) | Mortality Liver-related mortality Symptoms and complications Liver function tests Liver histology Adverse events | RR = 0.83 | 0.63-1.11 | Negative study (P = 0.21) |
| Mathurin et al[99], 2011 | RCTs from 1984 to 2006 with specific data on DF ≥ 32 or hepatic encephalopathy, of corticosteroids vs placebo, enteral nutrition or antioxidants | 5 (418) | Survival DF Lille score Liver function tests | Complete responder: HR = 0.18 | Complete responder: 0.05-0.71 | Positive study Complete responders (P = 0.005) |
| Serum creatinine Ascites | Partial responder: HR = 0.38 | Partial responder: 0.17-0.87 | Partial responders (P = 0.03) | |||
| Hepatic encephalopathy Age | Null responder: HR = 0.81 | Null responder: 0.45-1.45 | Null responders (P = 0.46) | |||
| Gender Leukocyte count | Used individual patient data analysis to increase statistical rigor for the meta-analysis |
RCT: Randomized controlled trials; AH: Alcoholic hepatitis; DF: Discriminant function.
The meta-analyses generally included only RCTs that analyzed patients with either DF ≥ 32 or hepatic encephalopathy, but none of the individual RCTs analyzed whether there was a maximum severity of AH (e.g., maximum DF) beyond which patients no longer benefited from corticosteroid therapy. One study[99] analyzed this question and noted that patients respond rapidly (≤ 7 d) to corticosteroids with sustained response until the conclusion of treatment. They stratified patients according to Lille score as complete responders (score ≤ 0.16), partial responders (score = 0.16-0.56), and null responders (score ≥ 0.56). Survival benefit was limited to patients who were partial or complete responders; therefore, this study suggests modifying corticosteroid therapy according to therapeutic response[99].
Clinical application of corticosteroid therapy for AH is currently limited by insufficient data on its molecular therapeutic mechanisms. However, in a recent study of mice heavily exposed to alcohol for 10 d, administration of prednisolone, a corticosteroid, enhanced ethanol-induced liver injury and fibrosis compared to untreated controls[105]. This study further investigated potential mechanisms for the deleterious effects of prednisolone after hepatotoxic injury. In carbon tetrachloride-induced liver injury in mice models, prednisolone led to attenuation of macrophage and neutrophil functions that normally help clear apoptotic cells and resolve hepatic inflammation, and caused delayed hepatocyte regeneration by inhibiting expression of genes involved in hepatocyte proliferation and repair, such as pSTAT3[105]. These data may help modify and improve clinical management of corticosteroid therapy for AH.
Despite variable survival benefit among studies, no severe complications were reported in patients receiving corticosteroid therapy, including no significantly increased risk of infections. Corticosteroid therapy should not be precluded in patients who have preexistent infections, after initiation of appropriate antibiotic therapy[106]. Although the current data are somewhat contradictory, use of corticosteroids is generally recommended as first-line therapy for severe AH[26,32].
Pentoxifylline: Pentoxifylline, a nonspecific phosphodiesterase inhibitor, has anti-inflammatory properties, including inhibition of tumor necrosis factor (TNF)-α, that may retard hepatic inflammation and fibrosis[107]. It prevents development of hepatopulmonary syndrome and development of a hyperdynamic circulatory state in cirrhotic rats[108]. It decreases the risk of hepatorenal syndrome (HRS), and significantly improves renal function in patients with severe AH or cirrhosis[107,109-111]. In a study of 50 patients, it decreased DF by > 50%, vs a decrease of only 7.1% in patients receiving placebo (P = 0.001)[109].
Despite these positive effects, improved survival from pentoxifylline remains controversial. Four RCTs of pentoxifylline vs placebo reported contradictory findings (Table 3)[107,109,110,112]. Two trials showed no statistically significant improvement in short-term survival[107,112]; a third trial showed statistically significant improvement[110]; and a fourth trial showed a statistically insignificant trend towards improved short-term survival (20% mortality with pentoxifylline vs 40% with placebo) (P = 0.216)[109]. A Cochrane review, incorporating 5 RCTs, was inconclusive, and recommended further RCTs on this drug[113]. Another meta-analysis, incorporating 884 patients, supported previous findings that pentoxifylline decreases the risk of severe HRS, but failed to demonstrate significantly improved survival[111]. Further research with larger patient studies is necessary to determine whether pentoxifylline improves survival. Nevertheless, the AASLD, ACG, and the European Association for the Study of the Liver (EASL) recommend pentoxifylline as a second-line therapy in patients with severe AH who have contraindications to corticosteroid therapy[26,32].
Table 3.
Published randomized controlled trials of pentoxifylline vs placebo for severe alcoholic hepatitis n (%)
| Ref. | n | Duration of treatment with pentoxifylline 400 mg PO tid | Mortality in placebo | Mortality in pentoxifylline | Relative risk or hazard ratio | 95%CI | Comments |
| Akriviadis et al[110], 2000 | 101 | 28 d | 24/52 (46) | 12/49 (24) | RR = 0.59 | 0.35-0.97 | Positive study (P = 0.037) |
| Fernández-Rodríguez et al[112], 2008 | 24 | 28 d | Not reported1 | Not reported1 | HR = 1.46 | 0.5-4.28 | Negative study (P = 0.48) |
| Tyagi et al[107], 2011 | 612 | 6 mo | 2/31 (6) | 1/30 (3) | Not reported | Not reported | Negative study2 (P = 0.15) |
| Sidhu et al[109], 2012 | 50 | 28 d | 10/25 (40) | 5/25 (20) | RR = 0.5 | 0.19-1.25 | Negative study (P = 0.216) |
Fernandez-Rodriguez et al[112] reported no statistically significant difference in short-term or long-term survival based on actuarial survival curve;
Tyagi et al[107] randomized 70 patients, but only 61 completed follow-up and were included in the analysis. The study did not show a significant difference in mortality, but showed a significant difference in the occurrence of hepatorenal syndrome. PO: Per overall survival; RR: Relative risk; HR: Hazard ratio.
Combination therapy: Corticosteroids or pentoxifylline are used in patients with severe AH, but the survival benefit for either drug remains controversial. Investigators combined both therapies to assess whether combination therapy is superior to corticosteroid monotherapy, especially for severe AH. However, two published RCTs found no significant difference in 6 mo mortality between combination therapy vs monotherapy[114,115]. The most recent RCT revealed 6-mo mortality of 30.1% in combination therapy vs 30.8% in monotherapy (P = 0.91)[115]. Although one RCT reported a significantly lower cumulative risk of HRS in the combination therapy group at 1 mo (P = 0.007)[115], the benefit was no longer significant at 6 mo[114,115]. Further studies are needed to explore combined treatment options to improve survival for severe AH.
Liver transplantation
LT is the only cure for end-stage ALD. Recent data from Organ Procurement and Transplantation Network (OPTN) and Scientific Registry of Transplant Recipients (SRTR) reveal 3563 alcoholic cirrhotics awaiting LT, constituting 23.2% of all patients awaiting LT[116]. Alcoholic cirrhosis is the second most common indication for LT, after cirrhosis from viral hepatitis[117]. Patients with alcoholic cirrhosis, however, have less likelihood of LT than other patients due to social factors. ALD is pejoratively thought as a “self-inflicted” disease, and donor organs are said to be better allocated to patients with other forms of end-stage liver disease (ESLD), which are not self-inflicted[118-120]. The critical, legitimate concern regarding LT for alcoholic cirrhosis is recidivism, with consequent disease recurrence in the allograft[117-121]. From 12%-46% of alcoholic cirrhotics resume alcohol consumption after LT[118-121]. The precise definition of recidivism varies among studies, and the rate of significant alcohol consumption post-transplant remains unclear[26]. Risk factors for recidivism include short duration of alcohol abstinence before LT, alcohol consumption just before LT, and patient denial of alcoholism[120,121]. To prevent recidivism, AASLD recommends LT candidates undergo assessment by an addictive behavior specialist, and delay of LT for ≥ 6 mo after commencing abstinence[70]. Six mo of abstinence may occasionally permit sufficient clinical improvement to render LT unnecessary[32]. EASL also supports this recommendation, and mandates a multidisciplinary approach, including psychological assessment, in addition to medical evaluation, to determine suitability for LT[26].
LT patients with alcoholic cirrhosis have at least comparable and perhaps even better survival than LT patients with other etiologies of ESLD[117,119,120]. For example, Burra et al[117] reported 1, 3, 5, and 10 years graft survival rates after LT in ALD patients to be 84%, 78%, 73%, and 58%, respectively; these rates are significantly higher than that for cirrhosis from viral hepatitis (P = 0.04) or cryptogenic cirrhosis (P = 0.05). Major causes of post-transplant mortality include infections, cardiovascular events and de novo malignancies[117], associated with immunosuppression[122,123]. De novo malignancies account for 23% of mortality in patients with alcoholic cirrhosis, compared to 11% of mortality in patients with cirrhosis from viral hepatitis without alcoholism or cryptogenic cirrhosis (P < 0.0001)[117]. The cumulative risk for de novo malignancies rises from 6% prior to LT to 55% 15 years after LT[26]. Therefore, regular screening for certain malignancies, including skin cancer, the most frequent post-transplantation cancer, is recommended[122].
NATURAL HISTORY AND COMPLICATIONS OF ALCOHOLIC CIRRHOSIS
Long-term management of complications of alcoholic cirrhosis is similar to that for other etiologies of cirrhosis (Table 4)[124-131]. Ascites is the most common complication of cirrhosis. Patients with new-onset ascites should undergo diagnostic paracentesis, to exclude other etiologies of ascites, such as cardiac disease, malignant ascites, or nephrotic syndrome; and to exclude spontaneous bacterial peritonitis (SBP). Ascitic fluid should be analyzed for cell count and differential, total protein, and serum-ascites albumin gradient (SAAG). A SAAG ≥ 1.1 g/dL supports the diagnosis of ascites secondary to portal hypertension; a SAAG < 1.1 g/dL supports other etiologies for ascites[132]. First-line treatment of ascites from cirrhosis includes alcohol cessation; dietary sodium restriction to ≤ 2 g/d; oral diuretics, usually spironolactone and furosemide; and discontinuation of non-steroidal anti-inflammatory drugs (NSAIDs)[129]. In patients who develop hyponatremia, reduction of diuretic dose or its temporary discontinuation may be necessary[127].
Table 4.
Management of complications of cirrhosis, per professional society guidelines1
| Complication | Screening/diagnosis | Treatment | Long-term management surveillance |
| Ascites | Diagnostic paracentesis for new-onset ascites: ascitic fluid analyzed for cell count and differential, total protein, and SAAG | Alcohol cessation; dietary sodium restriction; oral diuretics; discontinuation of NSAIDs | Refractory ascites: periodic large-volume therapeutic paracenteses; TIPS; midodrine; or peritoneovenous shunts |
| Spontaneous bacterial peritonitis | Diagnostic paracentesis: ≥ 250 polymorphonuclear cells/mm3 | Empiric antibiotic therapy with cefotaxime 2 g every 8 h, while awaiting culture results | Prophylaxis with norfloxacin or trimethoprim-sulfamethoxazole after one documented episode of SBP or if patient presents with variceal bleeding |
| Esophageal and gastric varices | Esophagogastroduodenoscopy | Treatment depends upon size of varices or risk of variceal bleeding: Prophylaxis with nadolol or propranolol for small varices at high risk of bleeding or for medium/large varices; EVL for medium/large varices at high risk of bleeding | No varices: EGD every 3 yr (earlier if hepatic decompensation occurs) Small varices: EGD every 2 yr Medium/large varices: EGD every 6-12 mo |
| Hepatic encephalopathy | Diagnosed by serum ammonia level and clinical findings of confusion, personality and mental status changes, and asterixis (exclude other causes of mental status changes) | Investigation and correction of precipitating factors; lactulose and/or rifaximin, supportive care | Secondary prophylaxis with lactulose and/or rifaximin indefinitely |
| Hepatorenal syndrome (type 1-rapidly progressive renal insufficiency; type 2-slowly progressive renal insufficiency) | Serum creatinine > 1.5 mg/dL, in the absence of other identifiable cause of renal failure (exclude other causes by urine chemistries, urine culture, and/or renal imaging) | Initial fluid challenge; albumin and terlipressin or albumin and combined octreotide plus midodrine; dialysis; LT definitive | Serial serum creatinine monitoring |
| Hepatocellular carcinoma (HCC) | Abdominal ultrasound every 6 mo; alpha fetoprotein determination every 6 mo no longer recommended, but optional | For HCC treatment[124] | Abdominal ultrasound every 6 mo |
| Hepatopulmonary syndrome | Screening by arterial blood gas; Confirmation by CEE | Symptomatic management with long-term oxygen therapy; LT definitive | |
| Portopulmonary hypertension | Screening by transthoracic Doppler echocardiography; Confirmation by right heart catheterization | Intravenous or inhaled prostacyclin; long-term oxygen therapy |
1American Association for the Study of Liver Diseases[124,128,129]; American College of Gastroenterology[125,126]; Department of Veterans Affairs Hepatitis C Resource Center Program and the National Hepatitis C Program[127]; European Association for the Study of the Liver[130]; and European Respiratory Society[131]. SAAG: Serum-ascites albumin gradient; NSAID: Non-steroidal anti-inflammatory drugs; TIPS: Transjugular intrahepatic portosystemic shunt; SBP: Spontaneous bacterial peritonitis; GI: Gastrointestinal; EGD: Esophagogastroduodenoscopy; EVL: Endoscopic variceal ligation; CEE: Transthoracic echocardiography with contrast enhancement.
Patients with refractory ascites may warrant second-line treatment, including serial, large-volume, therapeutic paracenteses, TIPS, and addition of midodrine, especially in patients with systemic hypotension[129]. Midodrine, an α-adrenergic agonist, improves systemic hemodynamics by causing arterial vasoconstriction (reversing arterial vasodilation that contributes to development of ascites)[127]. β-blockers, angiotensin converting enzyme inhibitors, and angiotensin receptor blockers are no longer recommended for patients with ascites from cirrhosis, because of risks of life-threatening systemic hypotension[129]. Infusion of 6-8 g of albumin per liter of removed ascitic fluid is recommended during large-volume paracentesis (removal of > 5 liters of ascitic fluid)[129]. Peritoneovenous shunts used to be popular to treat refractory ascites, but are now restricted to patients with diuretic-resistant ascites who are poor candidates for serial paracenteses, transplantation, or TIPS, because of risks of disseminated intravascular coagulation and/or sepsis[129,133-135].
SBP, a complication of ascites, is diagnosed by presence of ≥ 250 polymorphonuclear cells/mm3 in ascitic fluid. In the appropriate clinical setting, patients should receive empiric antibiotic therapy, preferably cefotaxime 2 g every 8 h, immediately after performing aerobic and anaerobic cultures of ascitic fluid[129]. Delaying antibiotic therapy to await culture results may cause life-threatening, overwhelming infection. Ascitic fluid culture is not necessary for diagnosis because up to 60% of patients have negative cultures[129]. Risk factors for persistent SBP include MELD score > 25, SAAG > 1.5, and positive ascitic fluid culture[136]. After one episode of SBP, patients should receive long-term prophylaxis with norfloxacin or trimethoprim/sulfamethoxazole[129]. Cirrhotic patients presenting with GI bleeding should also receive SBP antibiotic prophylaxis, with either intravenous ceftriaxone or oral norfloxacin, for 7 d[129].
Cirrhotic patients should undergo screening esophagogastroduodenoscopy (EGD) to diagnose or exclude esophageal and gastric varices. Classification of varices has been simplified to: small varices - minimally elevated veins above esophageal mucosal surface; medium varices - tortuous veins occupying < 1/3 of esophageal lumen; and large varices - tortuous veins occupying > 1/3 of esophageal lumen[128]. Patients with no varices undergo repeat EGD every 3 years, or sooner if hepatic decompensation occurs. Patients with small varices at increased risk of bleeding should receive primary prophylaxis with nonselective β-blockers, such as propranolol or nadolol, and should undergo EGD every 2 years. Patients at high risk of bleeding includes those with red wale markings at EGD or those with CTP stage B or C cirrhosis[128]. Patients with medium/large varices should also receive primary prophylaxis with nonselective β-blockers, but should undergo endoscopic variceal ligation when at high risk for variceal bleeding. This high-risk population should undergo surveillance EGD every 6-12 mo[127,128].
Hepatic encephalopathy is a potentially reversible neuropsychiatric disturbance resulting from hepatic insufficiency. It is characterized by confusion, personality and mental status changes, asterixis, and hyperammonemia. Hepatic encephalopathy is staged according to West-Haven criteria as: 0, normal; 1, mild; 2, lethargy; 3, somnolence-to-stupor; and 4, coma[126]. Precipitating factors, including GI bleeding, infections, electrolyte disturbances (especially hyponatremia), medications (primarily narcotics and sedatives), constipation, and excessive nitrogenous dietary intake, should be assiduously investigated and corrected[126]. Acute pharmacologic management includes lactulose and/or rifaximin therapy[125,126]. Lactulose, a non-absorbable disaccharide cathartic, reduces nitrogenous load in gut, thereby reducing ammonia production[126]. Rifaximin, an antimicrobial agent with minimal systemic absorption, reduces ammonia-producing enteric bacteria. Rifaximin has been shown to reduce the risk of breakthrough hepatic encephalopathy during a 6 mo period of remission and to be superior to lactulose in treating hepatic encephalopathy[137]. Supportive management includes fall prevention, nursing care, prophylactic intubation in cases of severe hepatic encephalopathy, and adequate nutritional support[126]. After recovery, patients require secondary prophylaxis indefinitely with lactulose, rifaximin, or combination therapy to prevent recurrence.
HRS is characterized by serum creatinine > 1.5 mg/dL in a patient with ESLD, in the absence of other identifiable causes of acute or chronic renal failure[130]. It is a diagnosis of exclusion. It is classified into: type 1 HRS, characterized by rapidly progressive impairment in renal function (100% increase in baseline creatinine or creatinine level > 2.5 mg/dL, usually within 2 wk); and type 2 HRS, characterized by slowly progressive (> 2 wk) worsening renal function[127,130]. All cirrhotic patients with sudden increases in serum creatinine to > 1.5 mg/dL should have discontinuation of diuretics and receive a fluid challenge with 1.5 L intravenous normal saline[138]. Patients who are prerenal respond to fluid challenge, with decrease in creatinine levels and improved urine output, whereas patients with HRS are mostly unresponsive to fluid challenge[127,138]. Other causes of renal toxicity should be excluded, such as NSAIDs, hypotension, hypovolemia, obstructive uropathy, and sepsis. First-line therapy for HRS includes albumin and terlipressin, a vasopressin analogue that improves splanchnic circulation[130], or albumin and combined octreotide plus midodrine[127]. Patients not responding to these therapies may require dialysis and subsequent LT (usually with simultaneous renal transplant), the only definitive treatment for HRS. Pentoxifylline, as aforementioned, can decrease the incidence of HRS[107].
HCC occurs in 5%-15% of patients with alcoholic cirrhosis[23]. The precise incidence is, however, uncertain, as patients with alcoholic cirrhosis are often co-infected with HCV, which acts synergistically to potentiate the risk of HCC[124]. Nevertheless, screening for HCC is recommended in all patients with alcoholic cirrhosis. HCC surveillance is usually performed by abdominal ultrasound every 6 mo. Surveillance with serial serum alpha-fetoprotein determinations is no longer recommended because of insufficient specificity and sensitivity[124], but is still frequently performed. Diagnosis and treatment are similar in all patients with HCC, regardless of etiology of cirrhosis. The reader is referred to a comprehensive review on this subject[124].
Pulmonary vascular complications of chronic liver disease include hepatopulmonary syndrome (HPS) and portopulmonary hypertension (PPHTN). HPS is defined as an arterial oxygenation defect caused by intrapulmonary vascular dilatation in patients with liver disease, especially cirrhosis[139]. It occurs in approximately 20% of patients awaiting LT. Symptoms include dyspnea and platypnea, a characteristic finding of increased shortness of breath on rising from supine to upright position[131]. Screening, using arterial blood gas, is done in LT candidates and patients with liver disease who present with such symptoms. Transthoracic echocardiography with contrast enhancement (CEE) is the gold standard for diagnosis of HPS. CEE is commonly accomplished by hand agitation of 10 mL normal saline, resulting in microbubbles (≤ 90 μm in diameter), which are injected into an upper extremity vein[131]. Detection of microbubbles within the left atrium is considered a positive CEE[131]. Diagnostic criteria include: (1) presence of liver disease; (2) alveolar-arterial oxygen tension difference (A-a gradient) ≥ 15 mmHg; and (3) positive CEE[131]. The only curative treatment for HPS is LT, but patients can be managed symptomatically with long-term oxygen therapy.
PPHTN is defined as pulmonary artery hypertension associated with portal hypertension, likely secondary to imbalance in vasoactive substances reaching the pulmonary circulation from portosystemic shunts or defective hepatic metabolism[140]. It occurs in approximately 5% of patients awaiting LT. Patients present with dyspnea, chest discomfort, or syncope. Transthoracic Doppler echocardiography is used for screening; PPHTN is suspected by finding of right ventricular systolic pressure > 40-50 mmHg. Diagnosis is confirmed by right heart catheterization, that reveals: (1) mean pulmonary artery pressure > 25 mmHg; (2) mean pulmonary artery occlusion pressure < 15 mmHg; and (3) pulmonary vascular resistance > 240 dyn-s/cm-5[131]. Treatment may include pulmonary vasodilator therapy with intravenous and inhaled prostacyclin, as well as long-term oxygen therapy. LT is reserved for patients who fail to improve with these therapies.
FUTURE DIRECTIONS
Current research on ALD involves non-invasive diagnosis of ALD and novel treatment options. Non-invasive diagnostic liver tests, including FibroScan, have been studied, but the diagnostic accuracy of these tests have not been compared to the gold standard of liver biopsy, to define cut-off values for ALD[141]. The current prognostic scoring systems account for only 75%-85% of mortality for ALD or other causes of liver disease. Scoring systems incorporating more linearly independent variables may increase prognostic accuracy.
Currently, LT remains the only curative treatment. Further studies are needed for currently popular therapies, such as corticosteroids and pentoxifylline, to determine efficacy, especially to prove survival benefit. Combined medical therapies may be useful to achieve synergy in improving survival.
New treatment options that target pathways implicated in ALD pathogenesis, including oxidative stress, endotoxin production, cytokine production, and immune regulators[12] are being investigated. Recently investigated antioxidants include milk thistle (silymarin extracts) and S-adenosyl-L-methionine, both of which have not been proven beneficial[142,143]. However, most studies have been of low quality, and high quality RCTs regarding these relatively nontoxic, and possibly helpful treatments should be performed. Other TNF-α inhibitors, including etanercept and infliximab, have been studied, but only 3 RCTs with small study sizes have been published on these medications[144-146]. Reported adverse events and likely increased mortality limit their use, but further studies may be needed to confirm these findings.
Interleukin-22 (IL-22) is a potential therapy for ALD[14]. IL-22 ameliorates hepatic steatosis and liver injury in animal models after acute or chronic-binge ethanol feeding[147]. It may promote hepatocyte proliferation or hepatic regeneration and inhibit hepatic fibrosis in response to alcohol-induced liver injury[147]. IL-22 theoretically appears to be relatively safe because only hepatocytes, epithelial cells, and a few other cell types have IL-22 receptors. IL-22, however, promotes proliferation of preexisting hepatomas, even though it does not initiate hepatoma formation[148]. It is therefore likely contraindicated in patients with ALD complicated by hepatoma and may have limited use in patients with alcoholic cirrhosis.
Increased intestinal permeability to gut-derived microorganisms appears to increase morbidity and mortality in AH[149]. Several multi-institutional consortia are developing therapies for AH based on preventing or neutralizing these effects of increased intestinal permeability. For example, lipopolysaccharide (LPS) antibody may help neutralize injury from lipopolysaccharide from exposure to gut-derived microorganisms. One study will compare the effects of lipopolysaccharide (LPS) antibody in combination with corticosteroids vs corticosteroid monotherapy in patients with severe AH[149]. Other studies will examine the efficacy of probiotics vs placebo for moderately severe AH, or the effect of adding zinc, a mineral that improves gut barrier function, to other therapies for severe AH.
Another promising approach to AH therapy is targeting macrophage/Kupfer cell activation in AH which leads to increased IL-1 beta activation. A clinical trial is examining a combination of Anakinra, an interleukin 1 receptor antagonist, and traditional therapy vs traditional therapy alone for severe AH[150]. Another attractive approach is to inhibit caspases which are death induction molecules downstream to TNF-alpha activation during hepatotoxic injury. Emricasan, a pancaspase inhibitor, is proposed to be tested to block hepatocyte injury induced by TNF-beta, without blocking the beneficial hepatic effects of TNF-beta on liver regeneration and immune cell function[150]. Other novel potential therapies are in the process of development or undergoing preliminary clinical trials[14].
CONCLUSION
ALD is a prominent and preventable cause of morbidity and mortality. The cornerstone of therapy is abstinence, which improves overall survival. Psychological and pharmacologic therapies can support abstinence. Nutritional and supportive therapies are also important. Several therapies for AH, such as corticosteroids and pentoxifylline, are widely administered, but their survival benefit remains unproven. These drugs are generally well tolerated, without significant toxicity. Other potential therapies include TNF-α inhibitors other than pentoxifylline, antioxidants, and complementary medicine, none of which have demonstrable benefits for ALD and are not recommended as therapies. LT remains the only definitive treatment for alcoholic cirrhosis, and multidisciplinary management, including aggressive psychosocial therapy to prevent relapse should be instituted post-transplant. Patients with advanced ALD have complications that are similar to cirrhosis of other etiologies. Prophylaxis, surveillance, and aggressive treatment are important to prevent significant morbidity and mortality.
Footnotes
P- Reviewers: Gao B, Shi BY S- Editor: Qi Y L- Editor: A E- Editor: Liu XM
References
- 1.World Health Organization. Global status report on alcohol and health. Geneva: World Health Organization; 2011. p. 286. [Google Scholar]
- 2.Kim WR, Brown RS, Terrault NA, El-Serag H. Burden of liver disease in the United States: summary of a workshop. Hepatology. 2002;36:227–242. doi: 10.1053/jhep.2002.34734. [DOI] [PubMed] [Google Scholar]
- 3.Paula H, Asrani SK, Boetticher NC, Pedersen R, Shah VH, Kim WR. Alcoholic liver disease-related mortality in the United States: 1980-2003. Am J Gastroenterol. 2010;105:1782–1787. doi: 10.1038/ajg.2010.46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.American Psychiatric Association. Alcohol Use Disorder. Diagnostic and Statistical Manual of Mental Disorders. Arlington, VA: American Psychiatric Publishing; 2013. pp. 490–497. [Google Scholar]
- 5.National Institute on Alcohol Abuse and Alcoholism. Rethinking Drinking: Alcohol and Your Health, 2010. Available from: http://rethinkingdrinking.niaaa.nih.gov.
- 6.Bellentani S, Saccoccio G, Costa G, Tiribelli C, Manenti F, Sodde M, Saveria Crocè L, Sasso F, Pozzato G, Cristianini G, et al. Drinking habits as cofactors of risk for alcohol induced liver damage. The Dionysos Study Group. Gut. 1997;41:845–850. doi: 10.1136/gut.41.6.845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Becker U, Deis A, Sørensen TI, Grønbaek M, Borch-Johnsen K, Müller CF, Schnohr P, Jensen G. Prediction of risk of liver disease by alcohol intake, sex, and age: a prospective population study. Hepatology. 1996;23:1025–1029. doi: 10.1002/hep.510230513. [DOI] [PubMed] [Google Scholar]
- 8.Tuyns AJ, Pequignot G. Greater risk of ascitic cirrhosis in females in relation to alcohol consumption. Int J Epidemiol. 1984;13:53–57. doi: 10.1093/ije/13.1.53. [DOI] [PubMed] [Google Scholar]
- 9.Ward RJ, Coutelle Ch. Women and alcohol susceptibility: could differences in alcohol metabolism predispose women to alcohol-related diseases. Arch Womens Ment Health. 2003;6:231–238. doi: 10.1007/s00737-003-0015-7. [DOI] [PubMed] [Google Scholar]
- 10.Wagnerberger S, Schäfer C, Schwarz E, Bode C, Parlesak A. Is nutrient intake a gender-specific cause for enhanced susceptibility to alcohol-induced liver disease in women. Alcohol Alcohol. 2008;43:9–14. doi: 10.1093/alcalc/agm161. [DOI] [PubMed] [Google Scholar]
- 11.Frezza M, di Padova C, Pozzato G, Terpin M, Baraona E, Lieber CS. High blood alcohol levels in women. The role of decreased gastric alcohol dehydrogenase activity and first-pass metabolism. N Engl J Med. 1990;322:95–99. doi: 10.1056/NEJM199001113220205. [DOI] [PubMed] [Google Scholar]
- 12.Seth D, Haber PS, Syn WK, Diehl AM, Day CP. Pathogenesis of alcohol-induced liver disease: classical concepts and recent advances. J Gastroenterol Hepatol. 2011;26:1089–1105. doi: 10.1111/j.1440-1746.2011.06756.x. [DOI] [PubMed] [Google Scholar]
- 13.Orman ES, Odena G, Bataller R. Alcoholic liver disease: pathogenesis, management, and novel targets for therapy. J Gastroenterol Hepatol. 2013;28 Suppl 1:77–84. doi: 10.1111/jgh.12030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gao B, Bataller R. Alcoholic liver disease: pathogenesis and new therapeutic targets. Gastroenterology. 2011;141:1572–1585. doi: 10.1053/j.gastro.2011.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Park EY, Lim MK, Oh JK, Cho H, Bae MJ, Yun EH, Kim DI, Shin HR. Independent and supra-additive effects of alcohol consumption, cigarette smoking, and metabolic syndrome on the elevation of serum liver enzyme levels. PLoS One. 2013;8:e63439. doi: 10.1371/journal.pone.0063439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Taniai M, Hashimoto E, Tokushige K, Kodama K, Kogiso T, Torii N, Shiratori K. Roles of gender, obesity, and lifestyle-related diseases in alcoholic liver disease: Obesity does not influence the severity of alcoholic liver disease. Hepatol Res. 2012;42:359–367. doi: 10.1111/j.1872-034X.2011.00935.x. [DOI] [PubMed] [Google Scholar]
- 17.Raynard B, Balian A, Fallik D, Capron F, Bedossa P, Chaput J, Naveau S. Risk factors of fibrosis in alcohol-induced liver disease. Hepatology. 2002;35:635–638. doi: 10.1053/jhep.2002.31782. [DOI] [PubMed] [Google Scholar]
- 18.Naveau S, Giraud V, Borotto E, Aubert A, Capron F, Chaput J. Excess weight risk factor for alcoholic liver disease. Hepatology. 1997;25:108–111. doi: 10.1002/hep.510250120. [DOI] [PubMed] [Google Scholar]
- 19.Fletcher LM, Halliday JW, Powell LW. Interrelationships of alcohol and iron in liver disease with particular reference to the iron-binding proteins, ferritin and transferrin. J Gastroenterol Hepatol. 1999;14:202–214. doi: 10.1046/j.1440-1746.1999.01836.x. [DOI] [PubMed] [Google Scholar]
- 20.Schmidt CS, Schön D, Schulte B, Lüth S, Polywka S, Reimer J. Viral hepatitis in alcohol-dependent inpatients: prevalence, risk factors, and treatment uptake. J Addict Med. 2013;7:417–421. doi: 10.1097/ADM.0b013e3182a50817. [DOI] [PubMed] [Google Scholar]
- 21.Zhang M, Wu R, Jiang J, Minuk GY, Niu J. The presence of hepatitis B core antibody is associated with more advanced liver disease in alcoholic patients with cirrhosis. Alcohol. 2013;47:553–558. doi: 10.1016/j.alcohol.2013.07.003. [DOI] [PubMed] [Google Scholar]
- 22.Mann RE, Smart RG, Govoni R. The epidemiology of alcoholic liver disease. Alcohol Res Health. 2003;27:209–219. [PMC free article] [PubMed] [Google Scholar]
- 23.MacSween RN, Burt AD. Histologic spectrum of alcoholic liver disease. Semin Liver Dis. 1986;6:221–232. doi: 10.1055/s-2008-1040605. [DOI] [PubMed] [Google Scholar]
- 24.O'Shea RS, McCullough AJ. Treatment of alcoholic hepatitis. Clin Liver Dis. 2005;9:103–134. doi: 10.1016/j.cld.2004.11.004. [DOI] [PubMed] [Google Scholar]
- 25.Pateria P, de Boer B, MacQuillan G. Liver abnormalities in drug and substance abusers. Best Pract Res Clin Gastroenterol. 2013;27:577–596. doi: 10.1016/j.bpg.2013.08.001. [DOI] [PubMed] [Google Scholar]
- 26.European Association for the Study of Liver. EASL clinical practical guidelines: management of alcoholic liver disease. J Hepatol. 2012;57:399–420. doi: 10.1016/j.jhep.2012.04.004. [DOI] [PubMed] [Google Scholar]
- 27.Sorbi D, Boynton J, Lindor KD. The ratio of aspartate aminotransferase to alanine aminotransferase: potential value in differentiating nonalcoholic steatohepatitis from alcoholic liver disease. Am J Gastroenterol. 1999;94:1018–1022. doi: 10.1111/j.1572-0241.1999.01006.x. [DOI] [PubMed] [Google Scholar]
- 28.Zhou SL, Gordon RE, Bradbury M, Stump D, Kiang CL, Berk PD. Ethanol up-regulates fatty acid uptake and plasma membrane expression and export of mitochondrial aspartate aminotransferase in HepG2 cells. Hepatology. 1998;27:1064–1074. doi: 10.1002/hep.510270423. [DOI] [PubMed] [Google Scholar]
- 29.Tchelepi H, Ralls PW, Radin R, Grant E. Sonography of diffuse liver disease. J Ultrasound Med. 2002;21:1023–1032; quiz 1033-1034. doi: 10.7863/jum.2002.21.9.1023. [DOI] [PubMed] [Google Scholar]
- 30.Attali P, Ink O, Pelletier G, Vernier C, Jean F, Moulton L, Etienne JP. Dupuytren’s contracture, alcohol consumption, and chronic liver disease. Arch Intern Med. 1987;147:1065–1067. [PubMed] [Google Scholar]
- 31.Okazaki H, Ito K, Fujita T, Koike S, Takano K, Matsunaga N. Discrimination of alcoholic from virus-induced cirrhosis on MR imaging. AJR Am J Roentgenol. 2000;175:1677–1681. doi: 10.2214/ajr.175.6.1751677. [DOI] [PubMed] [Google Scholar]
- 32.O'Shea RS, Dasarathy S, McCullough AJ. Alcoholic liver disease. Am J Gastroenterol. 2010;105:14–32; quiz 33. doi: 10.1038/ajg.2009.593. [DOI] [PubMed] [Google Scholar]
- 33.Liangpunsakul S, Crabb DW. Alcoholic liver disease. Textbook of Gastroenterology. 5th ed. Oxford: Blackwell Publishing Ltd; 2009. pp. 2247–2273. [Google Scholar]
- 34.Roberts EA, Schilsky ML. Diagnosis and treatment of Wilson disease: an update. Hepatology. 2008;47:2089–2111. doi: 10.1002/hep.22261. [DOI] [PubMed] [Google Scholar]
- 35.Mani H, Kleiner DE. Liver biopsy findings in chronic hepatitis B. Hepatology. 2009;49:S61–S71. doi: 10.1002/hep.22930. [DOI] [PubMed] [Google Scholar]
- 36.Rofsky NM, Fleishaker H. CT and MRI of diffuse liver disease. Semin Ultrasound CT MR. 1995;16:16–33. doi: 10.1016/0887-2171(95)90012-8. [DOI] [PubMed] [Google Scholar]
- 37.Pugh RN, Murray-Lyon IM, Dawson JL, Pietroni MC, Williams R. Transection of the oesophagus for bleeding oesophageal varices. Br J Surg. 1973;60:646–649. doi: 10.1002/bjs.1800600817. [DOI] [PubMed] [Google Scholar]
- 38.Lucey MR, Brown KA, Everson GT, Fung JJ, Gish R, Keeffe EB, Kneteman NM, Lake JR, Martin P, McDiarmid SV, et al. Minimal criteria for placement of adults on the liver transplant waiting list: a report of a national conference organized by the American Society of Transplant Physicians and the American Association for the Study of Liver Diseases. Liver Transpl Surg. 1997;3:628–637. doi: 10.1002/lt.500030613. [DOI] [PubMed] [Google Scholar]
- 39.Wiesner R, Edwards E, Freeman R, Harper A, Kim R, Kamath P, Kremers W, Lake J, Howard T, Merion RM, et al. Model for end-stage liver disease (MELD) and allocation of donor livers. Gastroenterology. 2003;124:91–96. doi: 10.1053/gast.2003.50016. [DOI] [PubMed] [Google Scholar]
- 40.Freeman RB, Wiesner RH, Harper A, McDiarmid SV, Lake J, Edwards E, Merion R, Wolfe R, Turcotte J, Teperman L. The new liver allocation system: moving toward evidence-based transplantation policy. Liver Transpl. 2002;8:851–858. doi: 10.1053/jlts.2002.35927. [DOI] [PubMed] [Google Scholar]
- 41.Malinchoc M, Kamath PS, Gordon FD, Peine CJ, Rank J, ter Borg PC. A model to predict poor survival in patients undergoing transjugular intrahepatic portosystemic shunts. Hepatology. 2000;31:864–871. doi: 10.1053/he.2000.5852. [DOI] [PubMed] [Google Scholar]
- 42.Kamath PS, Wiesner RH, Malinchoc M, Kremers W, Therneau TM, Kosberg CL, D’Amico G, Dickson ER, Kim WR. A model to predict survival in patients with end-stage liver disease. Hepatology. 2001;33:464–470. doi: 10.1053/jhep.2001.22172. [DOI] [PubMed] [Google Scholar]
- 43.Al Sibae MR, Cappell MS. Accuracy of MELD scores in predicting mortality in decompensated cirrhosis from variceal bleeding, hepatorenal syndrome, alcoholic hepatitis, or acute liver failure as well as mortality after non-transplant surgery or TIPS. Dig Dis Sci. 2011;56:977–987. doi: 10.1007/s10620-010-1390-3. [DOI] [PubMed] [Google Scholar]
- 44.The MELD Model 2013. Available from: http://www.mayoclinic.org/meld/mayomodel5.html.
- 45.Kim WR, Biggins SW, Kremers WK, Wiesner RH, Kamath PS, Benson JT, Edwards E, Therneau TM. Hyponatremia and mortality among patients on the liver-transplant waiting list. N Engl J Med. 2008;359:1018–1026. doi: 10.1056/NEJMoa0801209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Biggins SW, Kim WR, Terrault NA, Saab S, Balan V, Schiano T, Benson J, Therneau T, Kremers W, Wiesner R, et al. Evidence-based incorporation of serum sodium concentration into MELD. Gastroenterology. 2006;130:1652–1660. doi: 10.1053/j.gastro.2006.02.010. [DOI] [PubMed] [Google Scholar]
- 47.Maddrey WC, Boitnott JK, Bedine MS, Weber FL, Mezey E, White RI. Corticosteroid therapy of alcoholic hepatitis. Gastroenterology. 1978;75:193–199. [PubMed] [Google Scholar]
- 48.Carithers RL, Herlong HF, Diehl AM, Shaw EW, Combes B, Fallon HJ, Maddrey WC. Methylprednisolone therapy in patients with severe alcoholic hepatitis. A randomized multicenter trial. Ann Intern Med. 1989;110:685–690. doi: 10.7326/0003-4819-110-9-685. [DOI] [PubMed] [Google Scholar]
- 49.Ramond MJ, Poynard T, Rueff B, Mathurin P, Théodore C, Chaput JC, Benhamou JP. A randomized trial of prednisolone in patients with severe alcoholic hepatitis. N Engl J Med. 1992;326:507–512. doi: 10.1056/NEJM199202203260802. [DOI] [PubMed] [Google Scholar]
- 50.Mendenhall CL, Anderson S, Garcia-Pont P, Goldberg S, Kiernan T, Seeff LB, Sorrell M, Tamburro C, Weesner R, Zetterman R. Short-term and long-term survival in patients with alcoholic hepatitis treated with oxandrolone and prednisolone. N Engl J Med. 1984;311:1464–1470. doi: 10.1056/NEJM198412063112302. [DOI] [PubMed] [Google Scholar]
- 51.Theodossi A, Eddleston AL, Williams R. Controlled trial of methylprednisolone therapy in severe acute alcoholic hepatitis. Gut. 1982;23:75–79. doi: 10.1136/gut.23.1.75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Depew W, Boyer T, Omata M, Redeker A, Reynolds T. Double-blind controlled trial of prednisolone therapy in patients with severe acute alcoholic hepatitis and spontaneous encephalopathy. Gastroenterology. 1980;78:524–529. [PubMed] [Google Scholar]
- 53.Shumaker JB, Resnick RH, Galambos JT, Makopour H, Iber FL. A controlled trial of 6-methylprednisolone in acute alcoholic hepatitis. With a note on published results in encephalopathic patients. Am J Gastroenterol. 1978;69:443–449. [PubMed] [Google Scholar]
- 54.Blitzer BL, Mutchnick MG, Joshi PH, Phillips MM, Fessel JM, Conn HO. Adrenocorticosteroid therapy in alcoholic hepatitis. A prospective, double-blind randomized study. Am J Dig Dis. 1977;22:477–484. doi: 10.1007/BF01072499. [DOI] [PubMed] [Google Scholar]
- 55.Mathurin P, Mendenhall CL, Carithers RL, Ramond MJ, Maddrey WC, Garstide P, Rueff B, Naveau S, Chaput JC, Poynard T. Corticosteroids improve short-term survival in patients with severe alcoholic hepatitis (AH): individual data analysis of the last three randomized placebo controlled double blind trials of corticosteroids in severe AH. J Hepatol. 2002;36:480–487. doi: 10.1016/s0168-8278(01)00289-6. [DOI] [PubMed] [Google Scholar]
- 56.Forrest EH, Evans CD, Stewart S, Phillips M, Oo YH, McAvoy NC, Fisher NC, Singhal S, Brind A, Haydon G, et al. Analysis of factors predictive of mortality in alcoholic hepatitis and derivation and validation of the Glasgow alcoholic hepatitis score. Gut. 2005;54:1174–1179. doi: 10.1136/gut.2004.050781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Dominguez M, Rincón D, Abraldes JG, Miquel R, Colmenero J, Bellot P, García-Pagán JC, Fernández R, Moreno M, Bañares R, et al. A new scoring system for prognostic stratification of patients with alcoholic hepatitis. Am J Gastroenterol. 2008;103:2747–2756. doi: 10.1111/j.1572-0241.2008.02104.x. [DOI] [PubMed] [Google Scholar]
- 58.Lille Model 2013. Available from: http://www.lillemodel.com/score.aspscore=lillept.
- 59.Louvet A, Naveau S, Abdelnour M, Ramond MJ, Diaz E, Fartoux L, Dharancy S, Texier F, Hollebecque A, Serfaty L, et al. The Lille model: a new tool for therapeutic strategy in patients with severe alcoholic hepatitis treated with steroids. Hepatology. 2007;45:1348–1354. doi: 10.1002/hep.21607. [DOI] [PubMed] [Google Scholar]
- 60.Pessione F, Ramond MJ, Peters L, Pham BN, Batel P, Rueff B, Valla DC. Five-year survival predictive factors in patients with excessive alcohol intake and cirrhosis. Effect of alcoholic hepatitis, smoking and abstinence. Liver Int. 2003;23:45–53. doi: 10.1034/j.1600-0676.2003.01804.x. [DOI] [PubMed] [Google Scholar]
- 61.Borowsky SA, Strome S, Lott E. Continued heavy drinking and survival in alcoholic cirrhotics. Gastroenterology. 1981;80:1405–1409. [PubMed] [Google Scholar]
- 62.Powell WJ Jr, Klatskin G. Duration of survival in patients with Laennec's cirrhosis: Influence of alcohol withdrawal, and possible effects of recent changes in general management of the disease. Am J Med. 1968;44:406–420. doi: 10.1016/0002-9343(68)90111-3. [DOI] [PubMed] [Google Scholar]
- 63.Brunt PW, Kew MC, Scheuer PJ, Sherlock S. Studies in alcoholic liver disease in Britain. I. Clinical and pathological patterns related to natural history. Gut. 1974;15:52–58. doi: 10.1136/gut.15.1.52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Muntaner L, Altamirano JT, Augustin S, González A, Esteban R, Guardia J, Genescà J. High doses of beta-blockers and alcohol abstinence improve long-term rebleeding and mortality in cirrhotic patients after an acute variceal bleeding. Liver Int. 2010;30:1123–1130. doi: 10.1111/j.1478-3231.2010.02287.x. [DOI] [PubMed] [Google Scholar]
- 65.Xie YD, Feng B, Gao Y, Wei L. Effect of abstinence from alcohol on survival of patients with alcoholic cirrhosis: A systematic review and meta-analysis. Hepatol Res. 2013:Epub ahead of print. doi: 10.1111/hepr.12131. [DOI] [PubMed] [Google Scholar]
- 66.Luca A, García-Pagán JC, Bosch J, Feu F, Caballería J, Groszmann RJ, Rodés J. Effects of ethanol consumption on hepatic hemodynamics in patients with alcoholic cirrhosis. Gastroenterology. 1997;112:1284–1289. doi: 10.1016/s0016-5085(97)70142-2. [DOI] [PubMed] [Google Scholar]
- 67.Bardou-Jacquet E, Legros L, Soro D, Latournerie M, Guillygomarc’h A, Le Lan C, Brissot P, Guyader D, Moirand R. Effect of alcohol consumption on liver stiffness measured by transient elastography. World J Gastroenterol. 2013;19:516–522. doi: 10.3748/wjg.v19.i4.516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Gelsi E, Dainese R, Truchi R, Mariné-Barjoan E, Anty R, Autuori M, Burroni S, Vanbiervliet G, Evesque L, Cherikh F, et al. Effect of detoxification on liver stiffness assessed by Fibroscan® in alcoholic patients. Alcohol Clin Exp Res. 2011;35:566–570. doi: 10.1111/j.1530-0277.2010.01374.x. [DOI] [PubMed] [Google Scholar]
- 69.Trabut JB, Thépot V, Nalpas B, Lavielle B, Cosconea S, Corouge M, Vallet-Pichard A, Fontaine H, Mallet V, Sogni P, et al. Rapid decline of liver stiffness following alcohol withdrawal in heavy drinkers. Alcohol Clin Exp Res. 2012;36:1407–1411. doi: 10.1111/j.1530-0277.2012.01737.x. [DOI] [PubMed] [Google Scholar]
- 70.Murray KF, Carithers RL. AASLD practice guidelines: Evaluation of the patient for liver transplantation. Hepatology. 2005;41:1407–1432. doi: 10.1002/hep.20704. [DOI] [PubMed] [Google Scholar]
- 71.Matching Alcoholism Treatments to Client Heterogeneity: Project MATCH posttreatment drinking outcomes. J Stud Alcohol. 1997;58:7–29. [PubMed] [Google Scholar]
- 72.Nowinski J, Baker S, Carroll K. Twelve Step Facilitation Therapy Manual: A clinical guide for therapists treating individuals with alcohol abuse and dependence. Rockville, Maryland: National Institute on Alcohol Abuse and Alcoholism (NIAAA), National Institute of Health (NIH). Project MATCH Monograph Series 1992. Volume 1. Available from: http://lib.adai.washington.edu/pubs/match1/match1part1.pdf.
- 73.Kadden R, Carroll K, Donovan D, Cooney N, Monti P, Abrams D, Litt M, Hester R. Cognitive-Behavior Coping Skills Therapy Manual: A clinical research guide for therapists treating individuals with alcohol abuse and dependence. Rockville, Maryland: National Institute on Alcohol Abuse and Alcoholism (NIAAA), National Institute of Health (NIH). Project MATCH Monograph Series 1992. Volume 3. Available from: http://pubs.niaaa.nih.gov/publications/MATCHSeries3/Project%20MATCH%20Vol_3.pdf.
- 74.Miller W, Zweben A, DiClemente C, Rychtarik R. Motivational Enhancement Therapy Manual: A clinical research guide for therapists treating individuals with alcohol abuse and dependence. Rockville, Maryland: National Institute on Alcohol Abuse and Alcoholism (NIAAA), National Institute of Health (NIH). Project MATCH Monograph Series 1992. Volume 2. Available from: http://casaa.unm.edu/download/MET.pdf.
- 75.Fuller RK, Branchey L, Brightwell DR, Derman RM, Emrick CD, Iber FL, James KE, Lacoursiere RB, Lee KK, Lowenstam I. Disulfiram treatment of alcoholism. A Veterans Administration cooperative study. JAMA. 1986;256:1449–1455. [PubMed] [Google Scholar]
- 76.Björnsson E, Nordlinder H, Olsson R. Clinical characteristics and prognostic markers in disulfiram-induced liver injury. J Hepatol. 2006;44:791–797. doi: 10.1016/j.jhep.2005.12.016. [DOI] [PubMed] [Google Scholar]
- 77.Rösner S, Hackl-Herrwerth A, Leucht S, Vecchi S, Srisurapanont M, Soyka M. Opioid antagonists for alcohol dependence. Cochrane Database Syst Rev. 2010;(12):CD001867. doi: 10.1002/14651858.CD001867.pub3. [DOI] [PubMed] [Google Scholar]
- 78.Jarosz J, Miernik K, Wąchal M, Walczak J, Krumpl G. Naltrexone (50 mg) plus psychotherapy in alcohol-dependent patients: a meta-analysis of randomized controlled trials. Am J Drug Alcohol Abuse. 2013;39:144–160. doi: 10.3109/00952990.2013.796961. [DOI] [PubMed] [Google Scholar]
- 79.Pettinati HM, Gastfriend DR, Dong Q, Kranzler HR, O’Malley SS. Effect of extended-release naltrexone (XR-NTX) on quality of life in alcohol-dependent patients. Alcohol Clin Exp Res. 2009;33:350–356. doi: 10.1111/j.1530-0277.2008.00843.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Tetrault JM, Tate JP, McGinnis KA, Goulet JL, Sullivan LE, Bryant K, Justice AC, Fiellin DA. Hepatic safety and antiretroviral effectiveness in HIV-infected patients receiving naltrexone. Alcohol Clin Exp Res. 2012;36:318–324. doi: 10.1111/j.1530-0277.2011.01601.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Rösner S, Hackl-Herrwerth A, Leucht S, Lehert P, Vecchi S, Soyka M. Acamprosate for alcohol dependence. Cochrane Database Syst Rev. 2010;(9):CD004332. doi: 10.1002/14651858.CD004332.pub2. [DOI] [PubMed] [Google Scholar]
- 82.Mason BJ, Lehert P. Acamprosate for alcohol dependence: a sex-specific meta-analysis based on individual patient data. Alcohol Clin Exp Res. 2012;36:497–508. doi: 10.1111/j.1530-0277.2011.01616.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Mason BJ, Goodman AM, Chabac S, Lehert P. Effect of oral acamprosate on abstinence in patients with alcohol dependence in a double-blind, placebo-controlled trial: the role of patient motivation. J Psychiatr Res. 2006;40:383–393. doi: 10.1016/j.jpsychires.2006.02.002. [DOI] [PubMed] [Google Scholar]
- 84.Baltieri DA, De Andrade AG. Acamprosate in alcohol dependence: a randomized controlled efficacy study in a standard clinical setting. J Stud Alcohol. 2004;65:136–139. doi: 10.15288/jsa.2004.65.136. [DOI] [PubMed] [Google Scholar]
- 85.Mann K, Lehert P, Morgan MY. The efficacy of acamprosate in the maintenance of abstinence in alcohol-dependent individuals: results of a meta-analysis. Alcohol Clin Exp Res. 2004;28:51–63. doi: 10.1097/01.ALC.0000108656.81563.05. [DOI] [PubMed] [Google Scholar]
- 86.Palmer AJ, Neeser K, Weiss C, Brandt A, Comte S, Fox M. The long-term cost-effectiveness of improving alcohol abstinence with adjuvant acamprosate. Alcohol Alcohol. 2000;35:478–492. doi: 10.1093/alcalc/35.5.478. [DOI] [PubMed] [Google Scholar]
- 87.Addolorato G, Caputo F, Capristo E, Domenicali M, Bernardi M, Janiri L, Agabio R, Colombo G, Gessa GL, Gasbarrini G. Baclofen efficacy in reducing alcohol craving and intake: a preliminary double-blind randomized controlled study. Alcohol Alcohol. 2002;37:504–508. doi: 10.1093/alcalc/37.5.504. [DOI] [PubMed] [Google Scholar]
- 88.Addolorato G, Leggio L, Ferrulli A, Cardone S, Vonghia L, Mirijello A, Abenavoli L, D’Angelo C, Caputo F, Zambon A, et al. Effectiveness and safety of baclofen for maintenance of alcohol abstinence in alcohol-dependent patients with liver cirrhosis: randomised, double-blind controlled study. Lancet. 2007;370:1915–1922. doi: 10.1016/S0140-6736(07)61814-5. [DOI] [PubMed] [Google Scholar]
- 89.Addolorato G, Leggio L, Ferrulli A, Cardone S, Bedogni G, Caputo F, Gasbarrini G, Landolfi R. Dose-response effect of baclofen in reducing daily alcohol intake in alcohol dependence: secondary analysis of a randomized, double-blind, placebo-controlled trial. Alcohol Alcohol. 2011;46:312–317. doi: 10.1093/alcalc/agr017. [DOI] [PubMed] [Google Scholar]
- 90.Leggio L, Ferrulli A, Zambon A, Caputo F, Kenna GA, Swift RM, Addolorato G. Baclofen promotes alcohol abstinence in alcohol dependent cirrhotic patients with hepatitis C virus (HCV) infection. Addict Behav. 2012;37:561–564. doi: 10.1016/j.addbeh.2011.12.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Garbutt JC, Kampov-Polevoy AB, Gallop R, Kalka-Juhl L, Flannery BA. Efficacy and safety of baclofen for alcohol dependence: a randomized, double-blind, placebo-controlled trial. Alcohol Clin Exp Res. 2010;34:1849–1857. doi: 10.1111/j.1530-0277.2010.01273.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.McClain CJ, Barve SS, Barve A, Marsano L. Alcoholic liver disease and malnutrition. Alcohol Clin Exp Res. 2011;35:815–820. doi: 10.1111/j.1530-0277.2010.01405.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Tsiaousi ET, Hatzitolios AI, Trygonis SK, Savopoulos CG. Malnutrition in end stage liver disease: recommendations and nutritional support. J Gastroenterol Hepatol. 2008;23:527–533. doi: 10.1111/j.1440-1746.2008.05369.x. [DOI] [PubMed] [Google Scholar]
- 94.Huisman EJ, Trip EJ, Siersema PD, van Hoek B, van Erpecum KJ. Protein energy malnutrition predicts complications in liver cirrhosis. Eur J Gastroenterol Hepatol. 2011;23:982–989. doi: 10.1097/MEG.0b013e32834aa4bb. [DOI] [PubMed] [Google Scholar]
- 95.Koretz RL, Avenell A, Lipman TO. Nutritional support for liver disease. Cochrane Database Syst Rev. 2012;5:CD008344. doi: 10.1002/14651858.CD008344.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Plauth M, Cabré E, Riggio O, Assis-Camilo M, Pirlich M, Kondrup J, Ferenci P, Holm E, Vom Dahl S, Müller MJ, et al. ESPEN Guidelines on Enteral Nutrition: Liver disease. Clin Nutr. 2006;25:285–294. doi: 10.1016/j.clnu.2006.01.018. [DOI] [PubMed] [Google Scholar]
- 97.Plauth M, Cabré E, Campillo B, Kondrup J, Marchesini G, Schütz T, Shenkin A, Wendon J. ESPEN Guidelines on Parenteral Nutrition: hepatology. Clin Nutr. 2009;28:436–444. doi: 10.1016/j.clnu.2009.04.019. [DOI] [PubMed] [Google Scholar]
- 98.Poh Z, Chang PE. A current review of the diagnostic and treatment strategies of hepatic encephalopathy. Int J Hepatol. 2012;2012:480309. doi: 10.1155/2012/480309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Mathurin P, O’Grady J, Carithers RL, Phillips M, Louvet A, Mendenhall CL, Ramond MJ, Naveau S, Maddrey WC, Morgan TR. Corticosteroids improve short-term survival in patients with severe alcoholic hepatitis: meta-analysis of individual patient data. Gut. 2011;60:255–260. doi: 10.1136/gut.2010.224097. [DOI] [PubMed] [Google Scholar]
- 100.Rambaldi A, Saconato HH, Christensen E, Thorlund K, Wetterslev J, Gluud C. Systematic review: glucocorticosteroids for alcoholic hepatitis--a Cochrane Hepato-Biliary Group systematic review with meta-analyses and trial sequential analyses of randomized clinical trials. Aliment Pharmacol Ther. 2008;27:1167–1178. doi: 10.1111/j.1365-2036.2008.03685.x. [DOI] [PubMed] [Google Scholar]
- 101.Christensen E, Gluud C. Glucocorticoids are ineffective in alcoholic hepatitis: a meta-analysis adjusting for confounding variables. Gut. 1995;37:113–118. doi: 10.1136/gut.37.1.113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Imperiale TF, McCullough AJ. Do corticosteroids reduce mortality from alcoholic hepatitis A meta-analysis of the randomized trials. Ann Intern Med. 1990;113:299–307. doi: 10.7326/0003-4819-113-4-299. [DOI] [PubMed] [Google Scholar]
- 103.Stewart LA, Parmar MK. Meta-analysis of the literature or of individual patient data: is there a difference. Lancet. 1993;341:418–422. doi: 10.1016/0140-6736(93)93004-k. [DOI] [PubMed] [Google Scholar]
- 104.Mathurin P, Duchatelle V, Ramond MJ, Degott C, Bedossa P, Erlinger S, Benhamou JP, Chaput JC, Rueff B, Poynard T. Survival and prognostic factors in patients with severe alcoholic hepatitis treated with prednisolone. Gastroenterology. 1996;110:1847–1853. doi: 10.1053/gast.1996.v110.pm8964410. [DOI] [PubMed] [Google Scholar]
- 105.Kwon HJ, Won YS, Park O, Feng D, Gao B. Opposing effects of prednisolone treatment on T/NKT cell- and hepatotoxin-mediated hepatitis in mice. Hepatology. 2013:Epub ahead of print. doi: 10.1002/hep.26748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Louvet A, Wartel F, Castel H, Dharancy S, Hollebecque A, Canva-Delcambre V, Deltenre P, Mathurin P. Infection in patients with severe alcoholic hepatitis treated with steroids: early response to therapy is the key factor. Gastroenterology. 2009;137:541–548. doi: 10.1053/j.gastro.2009.04.062. [DOI] [PubMed] [Google Scholar]
- 107.Tyagi P, Sharma P, Sharma BC, Puri AS, Kumar A, Sarin SK. Prevention of hepatorenal syndrome in patients with cirrhosis and ascites: a pilot randomized control trial between pentoxifylline and placebo. Eur J Gastroenterol Hepatol. 2011;23:210–217. doi: 10.1097/MEG.0b013e3283435d76. [DOI] [PubMed] [Google Scholar]
- 108.Sztrymf B, Rabiller A, Nunes H, Savale L, Lebrec D, Le Pape A, de Montpreville V, Mazmanian M, Humbert M, Hervé P. Prevention of hepatopulmonary syndrome and hyperdynamic state by pentoxifylline in cirrhotic rats. Eur Respir J. 2004;23:752–758. doi: 10.1183/09031936.04.00080404. [DOI] [PubMed] [Google Scholar]
- 109.Sidhu SS, Goyal O, Singla M, Bhatia KL, Chhina RS, Sood A. Pentoxifylline in severe alcoholic hepatitis: a prospective, randomised trial. J Assoc Physicians India. 2012;60:20–22. [PubMed] [Google Scholar]
- 110.Akriviadis E, Botla R, Briggs W, Han S, Reynolds T, Shakil O. Pentoxifylline improves short-term survival in severe acute alcoholic hepatitis: a double-blind, placebo-controlled trial. Gastroenterology. 2000;119:1637–1648. doi: 10.1053/gast.2000.20189. [DOI] [PubMed] [Google Scholar]
- 111.Parker R, Armstrong MJ, Corbett C, Rowe IA, Houlihan DD. Systematic review: pentoxifylline for the treatment of severe alcoholic hepatitis. Aliment Pharmacol Ther. 2013;37:845–854. doi: 10.1111/apt.12279. [DOI] [PubMed] [Google Scholar]
- 112.Fernández-Rodríguez CM, Lledó JL, López-Serrano P, Gutiérrez ML, Alonso S, Pérez-Fernández MT, Fernández Gil M, Pazos R, Tolon R, Hernández T, et al. [Effect of pentoxifylline on survival, cardiac function and both portal and systemic hemodynamics in advanced alcoholic cirrhosis--a randomized double-blind placebo-controlled trial] Rev Esp Enferm Dig. 2008;100:481–489. doi: 10.4321/s1130-01082008000800007. [DOI] [PubMed] [Google Scholar]
- 113.Whitfield K, Rambaldi A, Wetterslev J, Gluud C. Pentoxifylline for alcoholic hepatitis. Cochrane Database Syst Rev. 2009;(4):CD007339. doi: 10.1002/14651858.CD007339.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Sidhu SS, Goyal O, Singla P, Gupta D, Sood A, Chhina RS, Soni RK. Corticosteroid plus pentoxifylline is not better than corticosteroid alone for improving survival in severe alcoholic hepatitis (COPE trial) Dig Dis Sci. 2012;57:1664–1671. doi: 10.1007/s10620-012-2097-4. [DOI] [PubMed] [Google Scholar]
- 115.Mathurin P, Louvet A, Duhamel A, Nahon P, Carbonell N, Boursier J, Anty R, Diaz E, Thabut D, Moirand R, et al. Prednisolone with vs without pentoxifylline and survival of patients with severe alcoholic hepatitis: a randomized clinical trial. JAMA. 2013;310:1033–1041. doi: 10.1001/jama.2013.276300. [DOI] [PubMed] [Google Scholar]
- 116.Matas AJ, Smith JM, Skeans MA, Lamb KE, Gustafson SK, Samana CJ, Stewart DE, Snyder JJ, Israni AK, Kasiske BL. Organ Procurement and Transplantation Network (OPTN) and Scientific Registry of Transplant Recipients (SRTR) 2011 Data Report. Am J Transpl. 2013;13(suppl 1):11–46. doi: 10.1111/ajt.12019. [DOI] [PubMed] [Google Scholar]
- 117.Burra P, Senzolo M, Adam R, Delvart V, Karam V, Germani G, Neuberger J. Liver transplantation for alcoholic liver disease in Europe: a study from the ELTR (European Liver Transplant Registry) Am J Transplant. 2010;10:138–148. doi: 10.1111/j.1600-6143.2009.02869.x. [DOI] [PubMed] [Google Scholar]
- 118.Mackie J, Groves K, Hoyle A, Garcia C, Garcia R, Gunson B, Neuberger J. Orthotopic liver transplantation for alcoholic liver disease: a retrospective analysis of survival, recidivism, and risk factors predisposing to recidivism. Liver Transpl. 2001;7:418–427. doi: 10.1053/jlts.2001.23789. [DOI] [PubMed] [Google Scholar]
- 119.Schmeding M, Heidenhain C, Neuhaus R, Neuhaus P, Neumann UP. Liver transplantation for alcohol-related cirrhosis: a single centre long-term clinical and histological follow-up. Dig Dis Sci. 2011;56:236–243. doi: 10.1007/s10620-010-1281-7. [DOI] [PubMed] [Google Scholar]
- 120.Hartl J, Scherer MN, Loss M, Schnitzbauer A, Farkas S, Baier L, Szecsey A, Schoelmerich J, Schlitt HJ, Kirchner GI. Strong predictors for alcohol recidivism after liver transplantation: non-acceptance of the alcohol problem and abstinence of < 3 months. Scand J Gastroenterol. 2011;46:1257–1266. doi: 10.3109/00365521.2011.603160. [DOI] [PubMed] [Google Scholar]
- 121.Kumar S, Stauber RE, Gavaler JS, Basista MH, Dindzans VJ, Schade RR, Rabinovitz M, Tarter RE, Gordon R, Starzl TE. Orthotopic liver transplantation for alcoholic liver disease. Hepatology. 1990;11:159–164. doi: 10.1002/hep.1840110202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Herrero JI. De novo malignancies following liver transplantation: Impact and recommendations. Liver Transpl. 2009;15:S90–S94. doi: 10.1002/lt.21898. [DOI] [PubMed] [Google Scholar]
- 123.Jonas S, Rayes N, Neumann U, Neuhaus R, Bechstein WO, Guckelberger O, Tullius SG, Serke S, Neuhaus P. De novo malignancies after liver transplantation using tacrolimus-based protocols or cyclosporine-based quadruple immunosuppression with an interleukin-2 receptor antibody or antithymocyte globulin. Cancer. 1997;80:1141–1150. doi: 10.1002/(sici)1097-0142(19970915)80:6<1141::aid-cncr18>3.0.co;2-8. [DOI] [PubMed] [Google Scholar]
- 124.Bruix J, Sherman M; American Association for the Study of Liver Diseases. Management of hepatocellular carcinoma: An update. Hepatology. 2011;53:1020–1022. doi: 10.1002/hep.24199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Hepatology Centers of Educational Expertise. Hepatic encephalopathy update: Reports from ACG 2012 and the Liver Meeting 2012. Available from: http://www.chronicliverdisease.org/disease_focus/enewsletters/HepCofEE_eNewsletter_Reports_From_ACG2012_2013_ol.pdf.
- 126.Blei AT, Córdoba J. Hepatic encephalopathy. Am J Gastroenterol. 2001;96:1968–1976. doi: 10.1111/j.1572-0241.2001.03964.x. [DOI] [PubMed] [Google Scholar]
- 127.Garcia-Tsao G, Lim JK. Management and treatment of patients with cirrhosis and portal hypertension: recommendations from the Department of Veterans Affairs Hepatitis C Resource Center Program and the National Hepatitis C Program. Am J Gastroenterol. 2009;104:1802–1829. doi: 10.1038/ajg.2009.191. [DOI] [PubMed] [Google Scholar]
- 128.Garcia-Tsao G, Sanyal AJ, Grace ND, Carey W. Prevention and management of gastroesophageal varices and variceal hemorrhage in cirrhosis. Hepatology. 2007;46:922–938. doi: 10.1002/hep.21907. [DOI] [PubMed] [Google Scholar]
- 129.Runyon B. AASLD Practice Guideline: Management of Adult Patients with Ascites Due to Cirrhosis: Update 2012. Available from: http://www.aasld.org/practiceguidelines/Documents/ascitesupdate2013.pdf. [DOI] [PubMed]
- 130.European Association for the Study of the Liver. EASL clinical practice guidelines on the management of ascites, spontaneous bacterial peritonitis, and hepatorenal syndrome in cirrhosis. J Hepatol. 2010;53:397–417. doi: 10.1016/j.jhep.2010.05.004. [DOI] [PubMed] [Google Scholar]
- 131.Rodríguez-Roisin R, Krowka MJ, Hervé P, Fallon MB. Pulmonary-Hepatic vascular Disorders (PHD) Eur Respir J. 2004;24:861–880. doi: 10.1183/09031936.04.00010904. [DOI] [PubMed] [Google Scholar]
- 132.Runyon BA, Montano AA, Akriviadis EA, Antillon MR, Irving MA, McHutchison JG. The serum-ascites albumin gradient is superior to the exudate-transudate concept in the differential diagnosis of ascites. Ann Intern Med. 1992;117:215–220. doi: 10.7326/0003-4819-117-3-215. [DOI] [PubMed] [Google Scholar]
- 133.Perera E, Bhatt S, Dogra VS. Complications of denver shunt. J Clin Imaging Sci. 2011;1:6. doi: 10.4103/2156-7514.75247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Sugawara S, Sone M, Arai Y, Sakamoto N, Aramaki T, Sato Y, Inaba Y, Takeuchi Y, Ueno T, Matsueda K, et al. Radiological insertion of Denver peritoneovenous shunts for malignant refractory ascites: a retrospective multicenter study (JIVROSG-0809) Cardiovasc Intervent Radiol. 2011;34:980–988. doi: 10.1007/s00270-010-0057-y. [DOI] [PubMed] [Google Scholar]
- 135.White MA, Agle SC, Padia RK, Zervos EE. Denver peritoneovenous shunts for the management of malignant ascites: a review of the literature in the post LeVeen Era. Am Surg. 2011;77:1070–1075. doi: 10.1177/000313481107700830. [DOI] [PubMed] [Google Scholar]
- 136.Desai AP, Reau N, Reddy KG, Te HS, Mohanty S, Satoskar R, Devoss A, Jensen D. Persistent spontaneous bacterial peritonitis: a common complication in patients with spontaneous bacterial peritonitis and a high score in the model for end-stage liver disease. Therap Adv Gastroenterol. 2012;5:275–283. doi: 10.1177/1756283X11417037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Bass NM, Mullen KD, Sanyal A, Poordad F, Neff G, Leevy CB, Sigal S, Sheikh MY, Beavers K, Frederick T, et al. Rifaximin treatment in hepatic encephalopathy. N Engl J Med. 2010;362:1071–1081. doi: 10.1056/NEJMoa0907893. [DOI] [PubMed] [Google Scholar]
- 138.Arroyo V, Ginès P, Gerbes AL, Dudley FJ, Gentilini P, Laffi G, Reynolds TB, Ring-Larsen H, Schölmerich J. Definition and diagnostic criteria of refractory ascites and hepatorenal syndrome in cirrhosis. Hepatology. 1996;23:164–176. doi: 10.1002/hep.510230122. [DOI] [PubMed] [Google Scholar]
- 139.Rodríguez-Roisin R, Agustí AG, Roca J. The hepatopulmonary syndrome: new name, old complexities. Thorax. 1992;47:897–902. doi: 10.1136/thx.47.11.897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Krowka MJ. Portopulmonary hypertension. Semin Respir Crit Care Med. 2012;33:17–25. doi: 10.1055/s-0032-1301731. [DOI] [PubMed] [Google Scholar]
- 141.Stevenson M, Lloyd-Jones M, Morgan MY, Wong R. Non-invasive diagnostic assessment tools for the detection of liver fibrosis in patients with suspected alcohol-related liver disease: a systematic review and economic evaluation. Health Technol Assess. 2012;16:1–174. doi: 10.3310/hta16040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Rambaldi A, Jacobs BP, Gluud C. Milk thistle for alcoholic and/or hepatitis B or C virus liver diseases. Cochrane Database Syst Rev. 2007;(4):CD003620. doi: 10.1002/14651858.CD003620.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Rambaldi A, Gluud C. S-adenosyl-L-methionine for alcoholic liver diseases. Cochrane Database Syst Rev. 2006;(2):CD002235. doi: 10.1002/14651858.CD002235.pub2. [DOI] [PubMed] [Google Scholar]
- 144.Spahr L, Rubbia-Brandt L, Frossard JL, Giostra E, Rougemont AL, Pugin J, Fischer M, Egger H, Hadengue A. Combination of steroids with infliximab or placebo in severe alcoholic hepatitis: a randomized controlled pilot study. J Hepatol. 2002;37:448–455. doi: 10.1016/s0168-8278(02)00230-1. [DOI] [PubMed] [Google Scholar]
- 145.Naveau S, Chollet-Martin S, Dharancy S, Mathurin P, Jouet P, Piquet MA, Davion T, Oberti F, Broët P, Emilie D. A double-blind randomized controlled trial of infliximab associated with prednisolone in acute alcoholic hepatitis. Hepatology. 2004;39:1390–1397. doi: 10.1002/hep.20206. [DOI] [PubMed] [Google Scholar]
- 146.Reep GL, Soloway RD. Recent and currently emerging medical treatment options for the treatment of alcoholic hepatitis. World J Hepatol. 2011;3:211–214. doi: 10.4254/wjh.v3.i8.211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Kong X, Feng D, Mathews S, Gao B. Hepatoprotective and anti-fibrotic functions of interleukin-22: therapeutic potential for the treatment of alcoholic liver disease. J Gastroenterol Hepatol. 2013;28 Suppl 1:56–60. doi: 10.1111/jgh.12032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Jiang R, Tan Z, Deng L, Chen Y, Xia Y, Gao Y, Wang X, Sun B. Interleukin-22 promotes human hepatocellular carcinoma by activation of STAT3. Hepatology. 2011;54:900–909. doi: 10.1002/hep.24486. [DOI] [PubMed] [Google Scholar]
- 149.Vlachogiannakos J, Viazis N, Vasianopoulou P, Vafiadis I, Karamanolis DG, Ladas SD. Long-term administration of rifaximin improves the prognosis of patients with decompensated alcoholic cirrhosis. J Gastroenterol Hepatol. 2013;28:450–455. doi: 10.1111/jgh.12070. [DOI] [PubMed] [Google Scholar]
- 150.Singal AK, Kamath PS, Gores GJ, Shah VH. Alcoholic Hepatitis: Current Challenges and Future Directions. Clin Gastroenterol Hepatol. 2013;pii:S1542–3565(13)00872-0. doi: 10.1016/j.cgh.2013.06.013. [DOI] [PMC free article] [PubMed] [Google Scholar]


