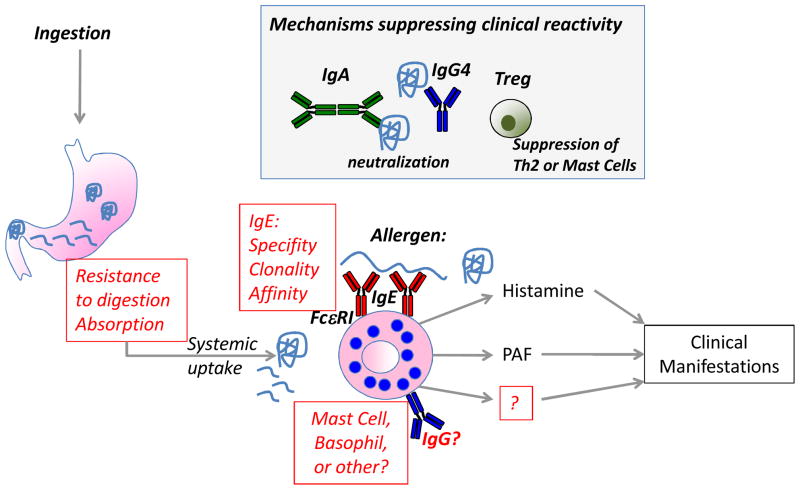
Figure 1. Factors contributing to clinical reactivity to foods.
The presence of food-specific IgE is not sufficient to predict clinical reactivity to foods, therefore other co-factors are needed. In a sensitized individual, allergen ingestion by the oral route can lead to clinical manifestations secondary to activation of systemic allergic effector cells by cross-linking IgE bound to effector cells through the FcεRI receptor. Highlighted in red are open questions about mechanisms contributing to the clinical reactivity to foods. Factors altering the absorption of food allergens from the intestine (e.g. food matrix, food processing such as heating), or preventing the proteolytic digestion of food allergens (e.g. antacid, food matrix, food processing) may determine whether clinical reactivity to foods occurs. The nature of the IgE response (affinity, clonality, linear versus conformational epitopes, and to which antigens within a food) will determine if activation of effector cells will occur. Questions remain about the relative contribution of mast cells and basophils in human food allergy, and the possible contribution of other effector cells or antibodies that have been shown to play a role in the mouse. In the grey box are mechanisms that are thought to suppress clinical reactivity to foods, and may play a role in the development of clinical tolerance. These include IgA and IgG4 that function as blocking antibodies and prevent IgE-mediated effector cell degranulation or IgE-facilitated antigen presentation, and Tregs that may suppress food allergy by blocking the generation of IgE (through blocking Th2 cells) or directly suppressing allergic effector cells.