Abstract
Objectives
The present study examined the impact of cumulative trauma exposure on current posttraumatic stress disorder (PTSD) symptom severity in a nonclinical sample of adults in their 60s. The predictive utility of cumulative trauma exposure was compared to other known predictors of PTSD, including trauma severity, personality traits, social support, and event centrality.
Method
Community-dwelling adults (n = 2,515) from the crest of the Baby Boom generation completed the Traumatic Life Events Questionnaire, the PTSD Checklist, the NEO Personality Inventory, the Centrality of Event Scale, and rated their current social support.
Results
Cumulative trauma exposure predicted greater PTSD symptom severity in hierarchical regression analyses consistent with a dose-response model. Neuroticism and event centrality also emerged as robust predictors of PTSD symptom severity. In contrast, the severity of individuals’ single most distressing life event, as measured by self-report ratings of the A1 PTSD diagnostic criterion, did not add explanatory variance to the model. Analyses concerning event categories revealed that cumulative exposure to childhood violence and adulthood physical assaults were most strongly associated with PTSD symptom severity in older adulthood. Moreover, cumulative self-oriented events accounted for a larger percentage of variance in symptom severity compared to events directed at others.
Conclusion
Our findings suggest that the cumulative impact of exposure to traumatic events throughout the life course contributes significantly to post-traumatic stress in older adulthood above and beyond other known predictors of PTSD.
Keywords: cumulative trauma exposure, PTSD symptom severity, personality, event centrality, social support
According to United States population estimates, the majority of individuals who experience a trauma report exposure to more than one traumatic event during their lifetime (Breslau et al., 1998; Kessler, Sonnega, Bromet, Hughes, & Nelson, 1995). The widespread prevalence of multiple lifetime traumas has driven interest in understanding the cumulative effects of exposure to trauma given the potential for important treatment and policy implications. Determining the role of cumulative trauma exposure in the development of trauma-related psychopathology may also elucidate the mechanisms underlying the observed heterogeneity in how individuals respond to traumatic events. Accordingly, a growing body of research has documented the impact of cumulative trauma exposure on a wide-range of psychological outcomes, including post-traumatic stress disorder (PTSD; Breslau, Peterson, & Schultz, 2008), depression (Kraaij & de Wilde, 2001), and life satisfaction (Krause, 2004).
In general, this research indicates that exposure to multiple traumatic events exerts a greater negative impact on the severity of posttraumatic outcomes compared to singular, discrete trauma (Green et al., 2000; Schnurr et al., 2002; Turner & Lloyd, 1995). Such findings support a dose-response model in which stressors of greater severity (as measured by proximity, duration, or frequency) are associated with greater impairments. However, the majority of studies concerning cumulative trauma have tested young adults (Lloyd & Taylor, 2003), samples ranging broadly in age with age covaried (Seery, Homan, & Silver, 2010), military service members (Clancy et al., 2006), or effects of cumulative trauma experienced during select developmental periods (i.e., childhood; Anda et al., 2006). It is important to investigate whether findings from such studies extend to lifetime trauma exposure among older adults who may be more likely to encounter traumatic events with age (Creamer & Parslow, 2008; Glaesmer et al., 2010; Spitzer et al., 2008) and exhibit greater stress symptoms following recent traumas compared to younger adults (Kimhi et al., 2012). Moreover, several factors specific to older adulthood may increase older adults’ vulnerability to negative post-traumatic outcomes compared to younger individuals (for reviews see Averill & Beck, 2000; Hiskey et al., 2008). Older adults may be more likely to experience certain types of trauma, in particular, unexpected deaths of close others, which has been linked to greater PTSD severity (Breslau et al., 1998). Loss of loved ones may have the secondary effect of diminishing social support networks, which may further increase PTSD severity (Brewin, Andrews, & Valentine, 2000). Certain normative life events that occur during older adulthood, such as retirement, are also associated with the resurgence or triggering of PTSD symptoms (Kaup, Ruskin, & Nyman, 1994; Schnurr et al., 2005). Related to physical health, research has shown that age-related changes in health status and mobility are accelerated by cumulative trauma exposure (Krause, Shaw, & Kairney, 2004). Furthermore, some researchers have proposed that PTSD may manifest differently in older adulthood, as indicated by more frequent reports of poor health, chronic pain, and cognitive impairment among older compared to younger adults with trauma histories (Graziano, 2003). The number of risk factors in older adulthood that contribute to an elevated risk of negative post-traumatic outcomes calls for wider investigation of how the health and well-being of older adults is impacted by the cumulative burden of traumatic life events.
The need for more research on cumulative trauma exposure in aging populations is further underscored by recent studies of adults ages 50 and older in which complex relations between cumulative trauma and various indices of psychological health and functioning were found. Keinan, Shrira, and Shmotkin (2012) reported that cumulative exposure to self-oriented traumatic events, or events directed at oneself, was associated with more depression symptoms and lower well-being, whereas cumulative exposure to other-oriented events (i.e., traumas directed at others) was associated with positive mental health outcomes, including well-being and optimism. Similarly, Shrira, Shmotkin, and Litwin (2012) found that self-oriented traumas experienced in adulthood were associated with greater depressive symptoms and lower life satisfaction, whereas early life other-oriented traumas were associated with lower depression and higher well-being. Collectively, these patterns of integrated resilience and vulnerability indicate that the relation between cumulative trauma exposure and post-traumatic outcomes may become more complex with age and that the extent of negative outcomes resulting from cumulative trauma exposure may depend on objective characteristics of the events including the target of the trauma. To date, however, it is unclear whether this mixed pattern of resilience and vulnerability for self-oriented compared to other-oriented traumas extends to PTSD in older adulthood.
The present study was designed to add to the literature concerning cumulative trauma in aging populations by examining the impact of cumulative trauma exposure on PTSD symptom severity in a large nonclinical sample of older adults in their 60s from the Baby Boom generation. We applied a life-span developmental framework to our study by examining the cumulative impact of all traumas experienced at every stage of the life course. We consider community-dwelling adults in their 60s an ideal population to examine the effects of cumulative trauma because they have lived long enough to potentially be exposed to many different types of trauma, they generally have intact cognitive abilities to report their experiences, and they are less likely to be suffering from chronic disease compared to older generations (Pruchno, 2012). Moreover, according to Life Course Theory (Elder, 1998), the historical timing and context of development shapes the way cohorts are differentially influenced by their life experiences. Thus, the extent to which data from other cohorts (i.e., Great Depression generation, Holocaust survivors) can be extrapolated to Baby Boomers is limited by Boomers’ experiences of important historical events at particular points in development (e.g., the Vietnam War as they transitioned to young adulthood which delayed education and family formation for many, the Civil Rights and gender equality movements of the 1960s, global economic insecurity as they face retirement). Furthermore, understanding how cumulative trauma impacts the lives of Boomers is growing more critical given recent demographic shifts that have resulted in Boomers comprising an increasingly disproportionate percentage of the population of the United States and Western Europe.
To extend previous research on cumulative trauma, we first examined whether the relation between cumulative trauma and PTSD symptom severity varied for self-oriented versus other-oriented events. Because different types of adversity subsumed within broad domains of cumulative trauma may differentially influence PTSD symptoms, events were further divided into various categories of cumulative exposure. In addition, the relation between cumulative trauma and PTSD symptom severity was compared to the predictive utility of individuals’ ratings of the severity of their most distressing trauma as indexed by the A1 PTSD diagnostic criterion [DSM-IV-TR, American Psychiatric Association (APA), 2000], according to which a person must have experienced, witnessed, or confronted “an event or events that involved actual or threatened death or injury, or a threat to the physical integrity of the self or others” (p. 467). The inclusion of the A1 criterion in the DSM-IV-TR and its retention in the DSM-V is based on research suggesting that events perceived as life-threatening are associated with more severe PTSD symptoms than non-life-threatening traumas (Kilpatrick et al., 1998; Ozer et al., 2003). However, considerable debate exists regarding how to best measure trauma severity and the utility of the A1 as a diagnostic requirement (Rubin & Feeling, 2013; Weathers & Keane, 2007).
Based on research showing that individual-differences contribute more variance in PTSD symptoms than objective characteristics of traumatic events (e.g., Weaver & Clum, 1995), several measures of individual-differences that have been linked to an elevated risk of PTSD were also examined. First, we compared cumulative trauma exposure to the personality domains included in the Five Factor Model (Costa & McCrae, 1992) based on reports of robust associations between certain personality traits and an elevated risk of PTSD. In particular, neuroticism, an enduring disposition characterized by high negative affect, has been shown to increase the likelihood of encountering negative and traumatic events (Lauterbach & Vrana, 2001; Magnus, Diener, Fujita, & Pavot, 1993; Specht, Egloff, & Schmukle, 2011) as well as PTSD symptom severity (Parslow, Jorm, & Christensen, 2006; Rubin, Berntsen, & Bohni, 2008a). Neuroticism increases the availability of memory for stressful events (Rubin et al., 2008a) and the tendency to interpret neutral or ambiguous stimuli in a negative or threatening manner (Costa & McCrae, 1990), which in turn may increase PTSD symptoms. Relations between PTSD and other personality traits have also been reported, including lower agreeableness, extraversion, and conscientiousness (Chung, Berger, & Rudd, 2007; Rubin, Boals, & Berntsen, 2008b). However, little research has examined the effects of personality on PTSD symptoms in older adults. Existing work has focused on neuroticism (van Zelst et al., 2003) or tested combat veterans (e.g., Davidson, Kudler, & Smith, 1987).
The second individual-difference factor examined in the present study is event centrality, or the perception of traumas as central to identity. Greater event centrality is thought to increase PTSD severity by enhancing the emotional salience of the trauma as well as the frequency and ease with which trauma memories come to mind (Berntsen & Rubin, 2006). Repeatedly re-experiencing the trauma through vivid intrusive memories or flashbacks that are typical of PTSD may also promote integration of the trauma memory into one’s autobiographical narrative, thereby increasing the likelihood that the event will be perceived as a highly salient turning point in the life story (Thomsen & Berntsen, 2008). Event centrality has emerged as a strong predictor of a wide-range of negative posttraumatic outcomes including symptoms of PTSD and depression (Berntsen & Rubin, 2006), lower self-esteem (Robinaugh & McNally, 2011), and poor physical health (Boals, 2010).
The third individual-difference factor examined in the present study was perceived social support based on findings that low social support is one of the strongest predictors of PTSD among trauma-exposed adults (Brewin et al., 2000; Ozer et al., 2003). According to the stress-buffering hypothesis (Cohen & Wills, 1985), supportive relationships help trauma survivors cope by assisting them in re-conceptualizing the event which decreases the likelihood of developing stress-related psychopathology. However, in an alternative account, the withdrawal and emotional numbing that is typical of PTSD can erode or impair interpersonal relations and over time reduce the availability and quality of social support (King, Taft, King, Hammond, & Stone, 2006). Understanding the impact of trauma on social support among older adults is especially important given the beneficial effects of social connectedness on well-being in older adulthood (Antonucci, 1991; Carstensen, 1992). Social support has also been cited as an important resource for older adults confronting stress and loss associated with aging, such as the death of significant others and life-threatening illness (Krause, 2001, 2005).
Four hypotheses were formulated based on the aforementioned literature. First, the relation between cumulative trauma exposure and PTSD symptoms was expected to be consistent with a dose-response model in which greater exposure to traumatic events throughout the life course would predict greater symptom severity in older adulthood. Second, cumulative trauma exposure was expected to be a stronger predictor of PTSD symptoms than the severity of individuals’ most distressing traumatic life event based on studies showing that lifetime cumulative trauma exerts a greater negative influence on psychological health than single, discrete traumas. Our third hypothesis maintained that individual-difference factors, including personality, event centrality, and social support would more strongly predict PTSD symptom severity than cumulative trauma based on prior studies showing that individual-differences typically account for greater variance in PTSD symptoms than objective event characteristics. Fourth, we hypothesized that self-oriented but not other-oriented traumas would predict PTSD symptom severity consistent with previous studies showing a detrimental effect of self-oriented events on psychological health and a beneficial effect of other-oriented events. Cumulative trauma was further divided into more distinct categories of events to explore which trauma categories were most strongly associated with greater PTSD symptom severity.
Method
Participants
Data were drawn from the 12th wave of the University of North Carolina Alumni Heart Study (UNCAHS), an ongoing longitudinal study of students who entered the University of North Carolina, Chapel Hill in 1964–1966 and their spouses (Siegler et al., 1992). Detailed information concerning recruitment procedures and participation rates of the UNCAHS are published elsewhere (Hooker, Hoppmann, & Siegler, 2010). Of the 3,682 individuals who completed the wave 12 questionnaire, our analyses were limited to the 3,420 respondents born in the 1940s to provide a more uniform age range of individuals belonging to the young-old period of older adulthood, and within this group to the 2,515 who reported their lifetime exposure to traumatic events at wave 12, completed measures of event centrality, social support, and PTSD symptoms at wave 12, and the NEO personality inventory previously during the study. Focusing our analyses on those born in the 1940s with the majority born in 1946–1949 allowed us to evaluate an important cohort at the crest of the Baby Boom (Carstensen & Hartel, 2006). An analysis comparing UNCAHS respondents included in the present report to those who were excluded due to missing data indicated that the groups did not differ on key demographic characteristics including income and marital status. Although the former group was slightly older and more educated, the sizes of the differences were small (birth year and education ηp2s were .02 and .01, respectively). Comparison of the gender compositions indicated that the group of respondents in the present analyses had a greater proportion of males, χ2 =128.72, p < .001.
The final sample included 805 females. Mean age was 60.83 (SD = 1.55). Participants were predominantly Caucasian (99.3%). Approximately 9% had less than a college degree, 18.37% had Bachelor’s degrees, 26.04% had Bachelor’s degrees plus additional training, 25.45% had Master’s degrees, and 21.59% had advanced degrees. The median annual household income reported in 2001–2002 was in the $70–99,999 range.
Measures
Traumatic events
The Traumatic Life Events Questionnaire (TLEQ; Kubany et al., 2000) assesses lifetime exposure to a wide-range of potentially traumatic events (Table 1). Participants reported the number of times they experienced each event using a 7-point scale. For the most serious occurrence of each event type, participants reported their age at the event and whether or not they experienced fear, helplessness, or horror during or immediately after the event. The TLEQ has strong psychometric properties and high convergent validity with structured clinical interviews (Kubany et al., 2000). Similar to epidemiological studies of trauma exposure that used mail surveys (e.g., Kessler et al., 1995), TLEQ items were modified to provide respondents extra privacy in reporting and to reduce redundancy. Specifically, one item (“Have you had any experiences like these that you feel you can’t tell about?”) was added, two items regarding miscarriage and abortion were combined, and four items concerning sexual assaults were collapsed to form one question. Participants were also asked whether or not the event met the DSM-IV-TR A1 criterion, which was analyzed as our measure of self-reported event severity. Our measure of cumulative exposure was defined as lifetime exposure to potentially traumatic events and was calculated by summing the number of events reported on the TLEQ.
Table 1.
Prevalence Rates of Traumatic Events
| Category | Potentially traumatic event | N (%) reported | N most distressing event |
|---|---|---|---|
| Death and illness | Unexpected death of loved one (O) | 1673 (66.52) | 779 |
| Illness or accident of loved one (O) | 1001 (39.80) | 239 | |
| Personal life-threatening illness (S) | 561 (22.31) | 345 | |
| Abortion/stillbirth (S/O) | 901 (35.83) | 110 | |
|
| |||
| Adult physical assault | Armed robbery to self or other | 237 (9.42) | 39 |
| Physical assault by stranger (S) | 168 (6.68) | 23 | |
| Witness attack or murder (O) | 135 (5.37) | 21 | |
| Death threat (S) | 393 (15.63) | 27 | |
| Intimate partner physical abuse (S) | 227 (9.03) | 31 | |
| Stalked (S) | 160 (6.36) | 16 | |
|
| |||
| Sexual assault | Touched sexually against will (S) | 309 (12.29) | 62 |
|
| |||
| Accidents and disaster | Motor vehicle accident (S) | 569 (22.62) | 162 |
| Natural disaster (S) | 178 (7.08) | 81 | |
| Other serious accident to self or other | 250 (9.94) | 51 | |
|
| |||
| Childhood violence | Childhood physical abuse (S) | 167 (6.64) | 26 |
| Witnessed family violence (O) | 316 (12.56) | 87 | |
|
| |||
| Warzone exposure | Warzone exposure | 266 (10.58) | 110 |
|
| |||
| Unclassified | Other distressing event | 614 (24.41) | 158 |
| Non-disclosed event | 132 (5.25) | 50 | |
Note. S = self-oriented event. O = other-oriented event. Abortion/stillbirth was classified as a self-oriented event for women and as an other-oriented event for men. Participants rated the PTSD symptom severity of their self-nominated most distressing traumatic life event.
TLEQ items were first classified as self-oriented (i.e., directed toward the self) or other-oriented (i.e., affected the self primarily through their impact on others). Five TLEQ items (Table 1) were not included in this classification because the subject of the event was unspecified. Separate proportion scores were calculated for each participant based on the number of self-oriented and other-oriented events.
TLEQ items were further grouped into six categories derived from classifications used in previous studies (Clancy et al., 2006; Dedert et al., 2009). The categories with the corresponding TLEQ items are listed in Table 1. Two TLEQ items (other life-threatening event, non-disclosed events) were not classified due to a lack of description. Proportion scores for each category were calculated for each participant.
PTSD symptom severity
The PTSD Checklist-Stressor Specific Version (PCL-S; Weathers, Litz, Huska, & Keane, 1994) is a 17-item measure of PTSD symptoms in reference to a specific event. Using 5-point scales (1=not at all, 5=extremely), respondents indicate whether a specific event produced each of the B, C, and D DSM-IV-TR PTSD symptoms during the previous month. The PCL has strong psychometric properties (Cronbach’s α = .94; Blanchard, Jones-Alexander, Buckley, & Forneris, 1996) and has been shown to have high agreement with clinician-diagnosed PTSD (r = .93). Cronbach’s α for the current sample was .93. Respondents completed the PCL-S in reference to the self-nominated TLEQ event that currently bothered them most. Ninety-eight participants did not identify the event for which they reported PTSD symptoms.
Personality
The NEO Personality Inventory (NEO; Costa & McCrae, 1992) assesses the Five-Factor Model of personality including the domains of neuroticism, extraversion, openness to experience, agreeableness, and conscientiousness. The NEO was administered twice in the UNCAHS (at baseline and in 1997; see Costa, Herbst, McCrae, & Siegler, 2000). Internal consistency for the domain scales ranged from 0.76 to 0.93 in the UNCAHS. Scores for adults are relatively stable with 3- to 6-year retest coefficients ranging from .63 to .83. Average t-scores for each domain were analyzed.
Event centrality
The Centrality of Event Scale (CES, Berntsen & Rubin, 2006) assesses the extent to which a trauma forms a central component of personal identity, a turning point in the life story, and a reference point for everyday inferences. Items were rated on 5-point scales (1=totally disagree, 5=totally agree). Respondents completed the 7-item version of the CES. Reported reliability is .88. Mean scores were analyzed.
Social support
Social support was assessed using an item from a measure of health and well-being in late and middle age (Siegler, 2004). Respondents rated “the support they receive from persons close” to them using a 4-point scale (1=poor, 4=excellent).
Procedure
UNCAHS members first received instructions to complete the wave 12 questionnaire online. Individuals who did not respond were mailed an identical paper survey up to three times. On the questionnaire, participants first answered questions concerning their health and social support, followed by the TLEQ. The CES and PCL were then completed in relation to the TLEQ event that currently bothered them most. All waves of the UNCAHS were approved by the Duke University Medical Center institutional review board.
Data Analysis
Hierarchical regressions were conducted to examine the impact of cumulative exposure on PCL severity scores in relation to known risk factors for PTSD, including event severity, personality, event centrality, and social support. The predictive utility of cumulative exposure to various categories of traumatic events was also examined. Hierarchical regressions permitted examination of the variance accounted for by each predictor. Education, gender, income, and marital status were entered first (step 1), followed by NEO domain scores (step 2), social support (step 3), event centrality scores (step 4), and cumulative trauma exposure (step 5). In a separate model with a subset of participants who rated the severity of their currently most distressing trauma (n = 1949), self-rated event severity was added on step 5 followed by cumulative exposure (step 6). Statistical significance was based on tests at the .05 level.
Results
Prevalence of Traumatic Events
The modal number of traumatic events was 2 and the mean was 6.15 (SD = 6.14, range = 1–56). Table 1 displays the frequency of each of the TLEQ events grouped into six event categories and the number of participants that nominated each event as their currently most distressing trauma.
Preliminary Analyses
The means (SDs) for variables included in the regressions were: agreeableness, 47.69 (9.74); conscientiousness, 51.87 (10.30); extraversion, 49.29 (9.52); neuroticism, 48.83 (9.97); openness, 53.11 (10.67); social support, 3.48 (.67); event centrality, 2.44 (1.23); PCL symptom severity; 22.74 (8.88); other-oriented events, .32 (.19); self-oriented events, .13 (.13); death and illness, .41 (.23); adult physical assaults, .09 (.14); childhood violence, .10 (.24); sexual assault, .12 (.33); accidents and disasters, .13 (.20); warfare exposure, .11 (.31). Approximately 58% of participants endorsed the A1 criterion for their most distressing event. Table 2 contains inter-correlations among predictor variables and PCL symptom severity scores. Significant associations emerged among PCL symptom severity scores and all socio-demographic variables. Cumulative exposure was associated with lower agreeableness, higher neuroticism, higher openness, lower social support, higher event centrality scores, greater event severity, and greater PCL severity scores.
Table 2.
Inter-correlations Among Predictor Variables and PTSD Symptom Severity
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Education | |||||||||||||
| 2. Gender | −.19*** | ||||||||||||
| 3. Income | .20*** | −.04* | |||||||||||
| 4. Marital status | .03 | −.03 | .28*** | ||||||||||
| 5. Agreeableness | −.13*** | .34*** | −.15*** | .05** | |||||||||
| 6. Conscientious | .08*** | −.06** | .18*** | .04* | −.18*** | ||||||||
| 7. Extraversion | −.08*** | .07*** | .16*** | .09*** | .06*** | −.07** | |||||||
| 8. Neuroticism | −.07*** | .25*** | −.13*** | −.09*** | .03* | .08** | −.21*** | ||||||
| 9. Openness | .17*** | .17*** | −.10*** | .14*** | .12*** | −.11*** | −.01 | .07*** | |||||
| 10. Social support | .05* | −.04* | .14*** | .21*** | .08*** | .08*** | .17*** | −.20*** | −.02 | ||||
| 11. Event centrality | −.03 | .19*** | −.11*** | −.12*** | .04* | −.01 | −.03 | .23*** | .14*** | −.11*** | |||
| 12. Cumulative | .00 | −.01 | −.09*** | −.10*** | −.13*** | −.02 | .00 | .09*** | .15*** | −.10*** | .27*** | ||
| 13. Event severity a | .00 | .03 | −.05* | −.03 | −.02 | −.02 | −.03 | .06** | .04* | −.02 | .29*** | .18*** | |
| 14. PCL severity | −.02 | .17*** | −.12*** | −.14*** | −.03 | −.06** | −.09*** | .33*** | .12*** | −.25*** | .56*** | .35*** | .17*** |
Note. Gender: 0 = male, 1 = female. Marital status: 0 = other, 1 = married. Cumulative = cumulative trauma exposure. PCL severity = PTSD Checklist symptom severity scores. Given that education is an ordinal variable, Spearman rank correlation coefficients are presented. All other values are Pearson correlation coefficients.
p ≤ .05,
p ≤ .01,
p ≤ .001.
n = 1949.
Main Analyses
Overall cumulative trauma exposure
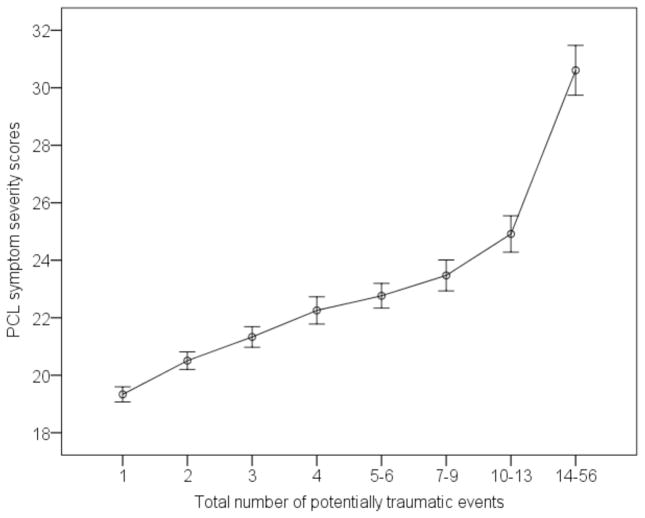
Table 3 presents results from a hierarchical regression testing the relation between cumulative exposure and PTSD symptom severity above and beyond other known predictors of PTSD. In the final model, cumulative exposure predicted greater PTSD symptom severity and increased the explained variance in PCL symptom severity scores from 39% to 42%. Figure 1 displays PCL severity scores as a function of cumulative exposure. As predicted, the relation between cumulative trauma exposure and PTSD symptom severity was consistent with a dose-response model.
Table 3.
Impact of Cumulative Trauma Exposure on PTSD Symptom Severity: Standardized Coefficients by Step (n = 2,515)
| Variables | Step 1 Demographics |
Step 2 Personality |
Step 3 Social support |
Step 4 Event centrality |
Step 5 Cumulative exposure |
|---|---|---|---|---|---|
| Education | .01 | .00 | .00 | .00 | .01 |
| Gender | .16*** | .11*** | .11*** | .04* | .05** |
| Income | −.08*** | −.05* | −.04 | −.01 | .00 |
| Marital status | −.11*** | −.07*** | −.05* | −.02 | −.01 |
| Agreeableness | −.10*** | −.08*** | −.07*** | −.04* | |
| Conscientiousness | −.08*** | −.06** | −.06*** | −.06*** | |
| Extraversion | −.03 | −.01 | −.02 | −.03 | |
| Neuroticism | .28*** | .26*** | .17*** | .17*** | |
| Openness | .07*** | .07*** | .03 | .00 | |
| Social support | −.16*** | −.14*** | −.13*** | ||
| Event centrality | .49*** | .45*** | |||
| Cumulative exposure | .20*** | ||||
|
| |||||
| ΔR2 | .05*** | .09*** | .02*** | .22*** | .03*** |
| R2 | .05 | .14 | .17 | .39 | .42 |
|
| |||||
| F (df) | 34.14*** (4, 2514) | 46.64*** (9, 2514) | 50.19*** (10, 2514) | 143.50*** (11, 2514) | 151.54*** (12, 2514) |
Note. Gender: 0 = male, 1 = female. Marital status: 1 = married, 0 = other.
p ≤ . 05,
p ≤ .01,
p ≤ .001
Figure 1.
PTSD Checklist (PCL) symptom severity scores as a function of the total number of events endorsed on the Traumatic Life Events Questionnaire. For the purpose of the figure, data points were combined into groups of 200 or more participants. The error bars represent +/− 1 standard error from the mean.
Regressions conducted to examine the predictive utility of cumulative exposure relative to participants’ ratings of the severity of their most distressing trauma revealed that, consistent with hypothesis 2, cumulative exposure significantly increased the explained variance in PTSD symptom severity (β = .20, p<.001), but self-rated event severity did not (β = −.01). The ΔR2 for cumulative exposure on step 6 was .03, F(1, 1935) = 115.48, p < .001. In contrast, when cumulative exposure was added on step 5 and self-rated event severity was added on step 6, ΔR2 on step 6 was .00, F(1, 1935) = .41. In a more conservative test of hypothesis 2, the index of cumulative exposure was restricted to TLEQ items for which participants endorsed the A1 criterion (i.e., cumulative A1 exposure). Results were not substantively changed. The regression equation in standardized betas for all variables significant at the ≤ .05 level was +.05 gender, −.06 agreeableness, −.07 conscientiousness, −.05 extraversion, +.17 neuroticism, −.12 social support, +.48 event centrality, −.04 event severity, +.15 cumulative A1 exposure [final model, F(13, 1935) = 102.02, p < .001, R2 = .40]. The ΔR2 for cumulative A1 exposure on step 6 was increased by .02, F(1, 1935) = 56.39, p < .001. In contrast, when cumulative A1 exposure was added on step 5 and event severity was added on step 6, ΔR2 on step 6 was .00, F(1, 1935) = 4.79, p < .05. These results suggest that the severity of participants’ most distressing life event had little to no observable association with PTSD symptom severity when cumulative trauma exposure was included in the model.
In partial support of hypothesis 3, event centrality and personality traits (entered as a group) explained more variance in PTSD symptom severity than cumulative trauma exposure.
Categories of cumulative trauma exposure
To examine whether cumulative exposure to self- versus other-oriented traumas differentially predicted PTSD symptom severity, proportion scores for cumulative self-oriented and other-oriented traumas replaced overall cumulative trauma exposure on step 5 of the regression model. In contrast to hypothesis 4, cumulative exposure to both other-oriented (β = .03, p < .05) and self-oriented traumas (β = .13, p < .001) predicted symptom severity [final model, F(13, 2514) = 129.45, p < .001, R2 = .40].
To explore the relation between cumulative exposure and PTSD symptom severity for more distinct categories of trauma, a final regression included proportion scores for cumulative exposure to the traumatic event categories on step 5. PCL severity scores were predicted by greater cumulative exposure to childhood violence (β = .09, p<.001), adult physical assaults (β = .07, p< .001), warzone exposure (β = .06, p<.01), sexual assaults (β = .05, p<.001), and death and illness (β = .03, p = .05), [final model, F(17, 2514) = 101.91, p < .001, R2 = .41].
Discussion
In the present study, greater exposure to traumatic events over the life course predicted more severe symptoms of PTSD in a nonclinical sample of adults in their 60s with a broad range of trauma histories. Our results extend previous research on the relation between cumulative trauma and PTSD by demonstrating that the cumulative burden of exposure to multiple traumatic events persists into older adulthood even among community-dwelling Baby Boomers who, based on their education and cohort membership, may have greater access to resources that protect against post-traumatic stress compared to other generations (Pruchno, 2012). Our results also revealed that although the self-rated severity of older adults’ currently most distressing trauma was positively correlated with PTSD symptoms, the association attenuated to non-significant levels in regression models with cumulative trauma exposure included. Moreover, when the measure of cumulative exposure was restricted to severe, life-threatening events, results further indicated that the severity of a single trauma did not explain unique variance in PTSD symptoms. Overall, our findings support a dose-response model, according to which the cumulative burden of lifetime trauma exposure is a stronger predictor of PTSD symptoms than the severity of a single traumatic event.
Our findings concerning individual-difference factors revealed that the extent to which older adults’ construed their most distressing trauma as central to their identity accounted for the largest percentage of explained variance in PTSD symptom severity. This finding corroborates previous studies in which subjective appraisals of traumas emerged as stronger predictors of post-traumatic outcomes compared to objective event characteristics, including whether or not the events were life-threatening (e.g., Boals & Schuettler, 2009; Kira et al., 2011; Martin, Cromer, DePrince, & Freyd, 2013). Notably, event centrality accounted for more variance in PTSD symptoms than low social support, which was identified as the strongest risk factor for PTSD in a previous meta-analysis (Brewin et al., 2000). Such results are commensurate with a core principle of Life Course Theory (Elder, 1998), which holds that the extent to which cumulative disadvantages negatively impact individuals’ developmental trajectories depends on their perceptions of their circumstances and their ability to mobilize resources. Additional research should seek to understand how event centrality impacts the aging process. According to Eriksonian theory (1982), the process of evaluating and accepting the events of one’s life is the primary developmental task of older adulthood. Our results suggest that treatments aimed at reducing the centrality of traumas as they are evaluated during the life review process (Butler, 2002) may be especially beneficial for older adult trauma survivors.
Our findings also add to the scarce literature concerning the impact of personality on PTSD among older adults. Of the five personality domains measured by the NEO, higher neuroticism scores emerged as the strongest predictor of PTSD symptom severity, followed by lower conscientiousness and lower agreeableness. Neuroticism is thought to increase the availability of memory for stressful events (Rubin et al., 2008a), which may in turn enhance and maintain PTSD symptoms. Neuroticism has also been linked to less adaptive coping strategies (Carver & Conner-Smith, 2010), increased symptom reporting (Coleman, 1997), and the tendency to interpret neutral or ambiguous stimuli in a negative manner (Costa & McCrae, 1990), all of which may influence the development of PTSD symptoms. In contrast, less is known about the mechanisms underlying the relations between other personality profiles and greater vulnerability to PTSD. Further research is needed to investigate the causal mechanisms underlying the relation between personality traits and PTSD symptomology in older adulthood.
Our study is the first to examine the potential differential impact of cumulative self- and other-oriented trauma exposure on PTSD symptom severity. Contrary to studies showing that cumulative other-oriented trauma is associated with positive post-traumatic outcomes, we found that cumulative exposure to both self-oriented and other-oriented traumas predicted greater PTSD symptom severity. The stronger association between PTSD symptoms and self-oriented traumas is consistent with studies in which a greater negative impact was found for self- compared to other-oriented events on depressive symptoms (Shmotkin & Litwin, 2009) and loneliness (Palgi et al., 2012). As noted by Shmotkin and Litwin (2009), compared to self-oriented traumas, other-oriented traumas may be accompanied by a greater sense of social responsibility to care for individuals directly impacted by the event. The heightened sense of responsibility to support others may in turn limit the severity of PTSD symptoms associated with other-oriented traumas, while promoting a greater sense of well-being as reported by Keinan et al. (2012) and (Shrira et al., 2012).
Our results concerning the extent to which cumulative trauma and PTSD symptom severity varied for more distinct categories of events revealed that greater cumulative exposure to childhood violence was the strongest predictor of PTSD symptom severity, followed by adult physical assaults, warzone exposure, sexual assaults, and death and illness. The finding that greater exposure to events involving physical violence in childhood and adulthood predicted greater PTSD symptom severity relative to other events is consistent with research by Breslau, Chilcoat, Kessler, and Davis (1999) in which assaultive violence among 18- to 45-year-olds conferred a higher risk of PTSD compared to other types of trauma. Our results add to this literature by showing that repeated exposure to assaultive violence throughout the lifespan has detrimental effects on mental health during older adulthood. This finding suggests that it may be important for clinicians to routinely assess lifetime exposure to assaultive violence when seeking to identify factors contributing to current distress among older adults.
Several limitations of this study should be noted. First, the UNCAHS is comprised of undergraduates who attended college in the 1960s. Although our relatively advantaged sample in terms of socio-economic status is typical of longitudinal studies, the underrepresentation of females, individuals with low education, and ethnic minorities limit the generalizability of our results to the general population. In spite of the select nature of our sample, results indicated that traumatic events and PTSD symptoms were not uncommon, even among a well-educated, predominantly male older adult sample for whom social and economic resources that may help protect against the negative effects of traumas may be readily available. Second, our findings may be subject to bias due to retrospective reports and defensive reporting given the perceived stigma of certain events. The majority of trauma research is, however, based on retrospective self-reports of uncertain validity. Research suggests that such reports are likely to promote underreporting (Hardt & Rutter, 2004), which may underestimate the negative consequences of cumulative trauma exposure. Finally, the correlational nature of our analyses prevents definitive conclusions regarding causal relations. Longitudinal and prospective studies are needed to delineate the causal relation between trauma, individual-differences, and PTSD symptoms. Despite these limitations, our findings underscore the importance of examining the broader context of lifetime trauma, as well as individual-differences in personality, stressor appraisal, and social support, when seeking to understand factors that influence post-traumatic stress among members of the Baby Boom generation.
Acknowledgments
Funding
This study was funded in part by the National Institute on Aging (R01-AG12458 and 5T32 AG000029-35), the National Heart Lung and Blood Institute (R01-HL55356), the National Institute of Mental Health (R01-MH066079), and the Duke Behavioral Medicine Research Center.
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4. Washington, DC: American Psychiatric Association; 2000. Text Revision. [Google Scholar]
- Anda RF, Felitti VJ, Bremner JD, Walker JD, Whitfield C, Perry BD, Giles WH. The enduring effects of abuse and related adverse experiences in childhood: A convergence of evidence from neurobiology and epidemiology. European Archives of Psychiatry and Clinical Neuroscience. 2006;256:174–186. doi: 10.1007/s00406-005-0624-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Antonucci TC. Attachment, social support, and coping with negative events in mature adulthood. In: Cummings EM, Greene AL, Karraker KH, editors. Life-span developmental psychology: Perspectives on stress and coping. Hillsdale, NJ: Lawrence Erlbaum Associates; 1991. pp. 261–276. [Google Scholar]
- Averill PM, Beck JG. Posttraumatic stress disorder in older adults: A conceptual review. Journal of Anxiety Disorders. 2000;14:133–156. doi: 10.1016/s0887-6185(99)00045-6. [DOI] [PubMed] [Google Scholar]
- Berntsen D, Rubin DC. The centrality of event scale: A measure of integrating a trauma into one’s identity and its relation to post-traumatic stress disorder symptoms. Behaviour Research and Therapy. 2006;44:219–231. doi: 10.1016/j.brat.2005.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berntsen D, Rubin DC. When a trauma becomes a key to identity: Enhanced integration of trauma memories predicts posttraumatic stress disorder symptoms. Applied Cognitive Psychology. 2007;21:417–431. [Google Scholar]
- Blanchard EB, Jones-Alexander J, Buckley TC, Forneris CA. Psychometric properties of the PTSD Checklist (PCL) Behaviour Research and Therapy. 1996;34:669–673. doi: 10.1016/0005-7967(96)00033-2. [DOI] [PubMed] [Google Scholar]
- Boals A. Autobiographical memories that have become central to identity: Gender differences in the Centrality of Events Scale for positive and negative events. Applied Cognitive Psychology. 2010;24:107–121. [Google Scholar]
- Boals A, Schuettler D. PTSD symptoms in response to traumatic and non-traumatic events: The role of respondent perception and A2 criterion. Journal of Anxiety Disorders. 2009;23:458–462. doi: 10.1016/j.janxdis.2008.09.003. [DOI] [PubMed] [Google Scholar]
- Breslau N, Chilcoat HD, Kessler RC, Davis GC. Previous exposure to trauma and PTSD effects of subsequent trauma: Results from the Detroit Area Survey of trauma. American Journal of Psychiatry. 1999;156:902–907. doi: 10.1176/ajp.156.6.902. [DOI] [PubMed] [Google Scholar]
- Breslau N, Kessler RC, Chilcoat HD, Schultz LR, Davis GC, Andreski P. Trauma and posttraumatic stress disorder in the community. Archives of General Psychiatry. 1998;55:913–917. doi: 10.1001/archpsyc.55.7.626. [DOI] [PubMed] [Google Scholar]
- Breslau N, Peterson EL, Schultz LR. A second look at prior trauma and the posttraumatic stress disorder effects of subsequent trauma: A prospective epidemiological study. Archives of General Psychiatry. 2008;65:431–437. doi: 10.1001/archpsyc.65.4.431. [DOI] [PubMed] [Google Scholar]
- Brewin CR, Andrews B, Valentine JD. Meta-analysis of risk factors for posttraumatic stress disorder in trauma-exposed adults. Journal of Consulting and Clinical Psychology. 2000;68:748–766. doi: 10.1037//0022-006x.68.5.748. [DOI] [PubMed] [Google Scholar]
- Butler RN. The life review. Journal of Geriatric Psychiatry. 2002;35:7–10. [Google Scholar]
- Carstensen LL. Social and emotional patterns in adulthood: Support for socioemotional selectivity theory. Psychology and Aging. 1992;7:331–338. doi: 10.1037//0882-7974.7.3.331. [DOI] [PubMed] [Google Scholar]
- Carstensen LL, Hartel CR. When I’m 64. Washington, DC. Committee on Aging Frontiers in Social Psychology, Personality, and Adult Developmental Psychology; Washington, DC: National Research Council/The National Academies Press; 2006. [Google Scholar]
- Carver CS, Conner-Smith J. Personality and coping. Annual Review of Psychology. 2010;61:679–704. doi: 10.1146/annurev.psych.093008.100352. [DOI] [PubMed] [Google Scholar]
- Chung MC, Berger Z, Rudd H. Comorbidity and personality traits in patients with different levels of posttraumatic stress disorder following myocardial infarction. Psychiatry Research. 2007;152:243–252. doi: 10.1016/j.psychres.2007.02.008. [DOI] [PubMed] [Google Scholar]
- Clancy CP, Graybeal A, Tompson WP, Badgett KS, Feldman ME, Calhoun PS, Beckham JC. Lifetime trauma exposure in veterans with military-related posttraumatic stress disorder: Association with current symptomatology. Journal of Clinical Psychiatry. 2006;67:1346–1353. doi: 10.4088/jcp.v67n0904. [DOI] [PubMed] [Google Scholar]
- Cohen S, Wills TA. Stress, social support, and the buffering hypothesis. Psychological Bulletin. 1985;98:310–357. [PubMed] [Google Scholar]
- Coleman PG. Personality, health, and ageing. Journal of the Royal Society of Medicine. 1997;90:27–33. doi: 10.1177/014107689709032s08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Costa PT, Herbst JH, McCrae RR, Siegler IC. Personality at midlife: Stability, intrinsic maturation, and response to life events. Assessment. 2000;20:365–378. doi: 10.1177/107319110000700405. [DOI] [PubMed] [Google Scholar]
- Costa PT, McCrae RR. Personality: Another “hidden factor” in stress research. Psychological Inquiry. 1990;1:22–24. [Google Scholar]
- Costa PT, McCrae RR. Revised NEO Personality Inventory (NEO PI-R) and NEO Five-Factor Inventory (NEO-FFI) Professional Manual. Lutz, FL: Psychological; 1992. [Google Scholar]
- Creamer M, Parslow R. Trauma exposure and posttraumatic stress disorder in the elderly: A community prevalence study. American Journal of Geriatric Psychiatry. 2008;16:853–856. doi: 10.1097/01.JGP.0000310785.36837.85. [DOI] [PubMed] [Google Scholar]
- Davidson J, Kudler H, Smith R. Personality in chronic post-traumatic stress disorder: A study of the Eysenck Inventory. Journal of Anxiety Disorders. 1987;1:295–300. [Google Scholar]
- Dedert EA, Green KT, Calhoun PS, Yoash-Gantz R, Taber KH, Mumford MM, Beckham JC. Association of trauma exposure with psychiatric morbidity in military veterans who have served since September 11, 2001. Journal of Psychiatric Research. 2009;43:830–836. doi: 10.1016/j.jpsychires.2009.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elder GH. The life course as developmental theory. Child Development. 1998;69:1–12. [PubMed] [Google Scholar]
- Erikson EH. The life cycle completed, a review. Norton; New York/London: 1982. [Google Scholar]
- Glaesmer H, Gunzelmann T, Braehler E, Forstmeier S, Maercker A. Traumatic experiences and post-traumatic stress disorder among elderly Germans: Results of a representative population-based survey. International Psychogeriatrics. 2010;22:661–670. doi: 10.1017/S104161021000027X. [DOI] [PubMed] [Google Scholar]
- Graziano R. Trauma and aging. Journal of Gerontological Social Work. 2003;40:3–27. [Google Scholar]
- Green BL, Goodman LA, Krupnick JL, Corcoran CB, Petty RM, Stockton P, Stern NM. Outcomes of single versus multiple trauma exposure in a screening sample. Journal of Traumatic Stress. 2000;13:271–286. doi: 10.1023/A:1007758711939. [DOI] [PubMed] [Google Scholar]
- Hardt J, Rutter M. Validity of adult retrospective reports of adverse childhood experiences: Review of the evidence. Journal of Child Psychology & Psychiatry. 2004;45:260–273. doi: 10.1111/j.1469-7610.2004.00218.x. [DOI] [PubMed] [Google Scholar]
- Hiskey S, Luckie M, Davies S, Brewin CR. The emergence of posttraumatic distress in later life: A review. Journal of Geriatric Psychiatry and Neurology. 2008;21:232–241. doi: 10.1177/0891988708324937. [DOI] [PubMed] [Google Scholar]
- Hooker K, Hoppmann C, Siegler IC. Personality: Life span compass for health. Annual Review of Gerontology and Geriatrics. 2010;30:201–232. [Google Scholar]
- Keinan G, Shrira A, Shmotkin D. The association between cumulative adversity and mental health: Considering does and primary focus of adversity. Quality of Life Research. 2012;21:1149–1158. doi: 10.1007/s11136-011-0035-0. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB. Posttraumatic stress disorder in the National Comorbidity Survey. Archives of General Psychiatry. 1995;52:1048–1060. doi: 10.1001/archpsyc.1995.03950240066012. [DOI] [PubMed] [Google Scholar]
- Kaup BA, Ruskin PE, Nyman G. Significant life events and PTSD in elderly World War II veterans. The Journal of Geriatric Psychiatry. 1994;2:239–243. doi: 10.1097/00019442-199400230-00008. [DOI] [PubMed] [Google Scholar]
- Kilpatrick DG, Resnick HS, Freedy JR, Pelcovitz D, Resick P, Roth S, van der Kolk B. Posttraumatic stress disorder field trial: Evaluation of the PTSD construct-Criteria A through E. In: Widiger T, Frances A, Pincus H, Ross R, First M, Davis W, Kline M, editors. DSM-IV Sourcebook. Washington, DC: American Psychiatric Press; 1998. pp. 803–844. [Google Scholar]
- Kimhi S, Hantman S, Goroshit M, Eshel Y, Zysberg L. Elderly people cope with the aftermath of war: Resilience versus vulnerability. American Journal of Psychiatry. 2012;20:391–401. doi: 10.1097/JGP.0b013e31821106b3. [DOI] [PubMed] [Google Scholar]
- King DW, Taft C, King LA, Hammond C, Stone ER. Directionality of the association between social support and posttraumatic stress disorder: A longitudinal investigation. Journal of Applied Social Psychology. 2006;36:2980–2992. [Google Scholar]
- Kira IA, Templin T, Lewandowski L, Ramaswamy V, Ozkan B, Abou-Mediane S, Alamia H. Cumulative tertiary appraisals of traumatic events across cultures: Two studies. Journal of Loss and Trauma. 2011;16:43–66. [Google Scholar]
- Kraaij V, de Wilde EJ. Negative life events and depressive symptoms in the elderly: A life-span perspective. Aging & Mental Health. 2001;5:84–91. doi: 10.1080/13607860020020681. [DOI] [PubMed] [Google Scholar]
- Krause N. Social support. In: Binstock RH, George LK, editors. Handbook of aging and the social sciences. San Diego, CA: Academic Press; 2001. pp. 272–294. [Google Scholar]
- Krause N. Lifetime trauma, emotional support, and life satisfaction among older adults. The Gerontologist. 2004;44:615–623. doi: 10.1093/geront/44.5.615. [DOI] [PubMed] [Google Scholar]
- Krause N. Exploring age differences in the stress-buffering function of social support. Psychology and Aging. 2005;20:714–717. doi: 10.1037/0882-7974.20.4.714. [DOI] [PubMed] [Google Scholar]
- Krause N, Shaw BA, Cairney J. A descriptive epidemiology of lifetime trauma and the physical health status of older adults. Psychology and Aging. 2004;19:637–648. doi: 10.1037/0882-7974.19.4.637. [DOI] [PubMed] [Google Scholar]
- Kubany ES, Leisen MB, Kaplan AS, Watson SB, Haynes SN, Owens JA, Burns K. Development and preliminary validation of a brief broad-spectrum measure of trauma exposure: The Traumatic Life Events Questionnaire. Psychological Assessment. 2000;12:210–224. doi: 10.1037//1040-3590.12.2.210. [DOI] [PubMed] [Google Scholar]
- Lauterbach D, Vrana S. The relationship among personality variables, exposure to traumatic events, and severity of posttraumatic stress symptoms. Journal of Traumatic Stress. 2001;14:29–45. [Google Scholar]
- Lloyd DA, Taylor J. Cumulative adversity and posttraumatic stress disorder: Evidence from a diverse community sample of young adults. American Journal of Orthopsychiatry. 2003;73:381–391. doi: 10.1037/0002-9432.73.4.381. [DOI] [PubMed] [Google Scholar]
- Magnus K, Diener E, Fujita F, Pavot W. Extraversion and neuroticism as predictors of objective life events: A longitudinal analysis. Journal of Personality and Social Psychology. 1993;65:1046–1053. doi: 10.1037//0022-3514.65.5.1046. [DOI] [PubMed] [Google Scholar]
- Martin CG, Cromer LD, DePrince AP, Freyd JJ. The role of cumulative trauma, betrayal, and appraisals in understanding trauma symptomatology. Psychological Trauma: Theory, Research, Practice, and Policy. 2013;5:110–118. doi: 10.1037/a0025686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ozer EJ, Best SR, Lipsey TL, Weiss DS. Predictors of posttraumatic stress disorder and symptoms in adults: A meta-analysis. Psychological Bulletin. 2003;129:52–73. doi: 10.1037/0033-2909.129.1.52. [DOI] [PubMed] [Google Scholar]
- Palgi Y, Shrira A, Ben-Ezra M, Shiovitz-Ezra S, Ayalon L. Self- and other-oriented potential lifetime traumatic events as predictors of loneliness in the second half of life. Aging & Mental Health. 2012;16:423–430. doi: 10.1080/13607863.2011.638903. [DOI] [PubMed] [Google Scholar]
- Parslow RA, Jorm AF, Christensen H. Associations with pre-trauma attributes and trauma exposure with screening positive for PTSD: Analysis of a community-based study of 2085 young adults. Psychological Medicine. 2006;36:387–395. doi: 10.1017/S0033291705006306. [DOI] [PubMed] [Google Scholar]
- Pruchno R. Not your mother’s old age: Baby boomers at age 65. The Gerontologist. 2012;52:149–152. doi: 10.1093/geront/gns038. [DOI] [PubMed] [Google Scholar]
- Robinaugh DJ, McNally RJ. Trauma centrality and PTSD symptom severity in adult survivors of childhood sexual abuse. Journal of Traumatic Stress. 2011;24:483–496. doi: 10.1002/jts.20656. [DOI] [PubMed] [Google Scholar]
- Rubin DC, Berntsen D, Bohni MK. A memory-based model of posttraumatic stress disorder: Evaluating basic assumptions underlying the PTSD diagnosis. Psychological Review. 2008a;115:985–1011. doi: 10.1037/a0013397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rubin DC, Boals A, Berntsen D. Memory in posttraumatic stress disorder: Properties of voluntary and involuntary, traumatic and non-traumatic autobiographical memories in people with and without PTSD symptoms. Journal of Experimental Psychology: General. 2008b;137:591–614. doi: 10.1037/a0013165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rubin DC, Feeling N. Measuring the severity of negative and traumatic events. Clinical Psychological Science. doi: 10.1177/2167702613483112. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schnurr PP, Lunney CA, Sengupta A, Spiro A. A longitudinal study of retirement in older male veterans. Journal of Consulting and Clinical Psychology. 2005;73:561–566. doi: 10.1037/0022-006X.73.3.561. [DOI] [PubMed] [Google Scholar]
- Schnurr PP, Spiro AS, Vielhauer MJ, Findler MN, Hamblen JL. Trauma in the lives of older men: Findings from the Normative Aging Study. Journal of Clinical Geropsychology. 2002;8:175–187. [Google Scholar]
- Seery MD, Holman EA, Silver RC. Whatever does not kill us: Cumulative lifetime adversity, vulnerability, and resilience. Journal of Personality and Social Psychology. 2010;99:1025–1041. doi: 10.1037/a0021344. [DOI] [PubMed] [Google Scholar]
- Shmotkin D, Litwin H. Cumulative adversity and depressive symptoms among older adults in Israel: The differential roles of self-oriented versus other-oriented events of potential trauma. Social Psychiatry and Psychiatric Epidemiology. 2009;44:989–997. doi: 10.1007/s00127-009-0020-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shrira A, Shmotkin D, Litwin H. Potentially traumatic events at different points in the life span and mental health: Findings from SHARE-Israel. American Journal of Orthopsychiatry. 2012;82:251–259. doi: 10.1111/j.1939-0025.2012.01149.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siegler IC. Middle Age Concerns Scale. Developed for UNC Alumni Heart Study. Behavioral Medicine Research Center, Duke University; Durham, NC: 2004. [Google Scholar]
- Siegler IC, Peterson BL, Barefoot JC, Harvin SH, Dahlstrom WG, Kaplan BH, Williams RB. Using college alumni populations in epidemiologic research: The UNC Alumni Heart Study. Journal of Clinical Epidemiology. 1992;45:1243–1250. doi: 10.1016/0895-4356(92)90165-j. [DOI] [PubMed] [Google Scholar]
- Specht J, Egloff B, Schmukle SC. Stability and change of personality across the life course: The impact of age and major life events on mean-level and rank order stability of the Big Five. Journal of Personality and Social Psychology. 2011;101:862–882. doi: 10.1037/a0024950. [DOI] [PubMed] [Google Scholar]
- Spitzer C, Barnow S, Volzke H, John U, Freyberger HJ, Grabe HJ. Trauma and posttraumatic stress disorder in the elderly: Findings from a German community study. Journal of Clinical Psychiatry. 2008;69:693–700. doi: 10.4088/jcp.v69n0501. [DOI] [PubMed] [Google Scholar]
- Thomsen DK, Berntsen D. The long-term impact of emotionally stressful events on memory characteristics and life story. Applied Cognitive Psychology. 2008;23:579–598. [Google Scholar]
- Turner RJ, Lloyd DA. Lifetime traumas and mental health: The significance of cumulative adversity. Journal of Health and Social Behavior. 1995;36:360–376. [PubMed] [Google Scholar]
- van Zelst WH, de Beurs E, Beekham ATF, Deeg DJH, van Dyck R. Prevalence and risk factors of posttraumatic stress disorder in older adults. Psychotherapy and Psychosomatics. 2003;72:333–342. doi: 10.1159/000073030. [DOI] [PubMed] [Google Scholar]
- Weathers FW, Keane TM. The Criterion A problem revisited: Controversies and challenges in defining and measuring psychological trauma. Journal of Traumatic Stress. 2007;20:107–121. doi: 10.1002/jts.20210. [DOI] [PubMed] [Google Scholar]
- Weathers FW, Litz BT, Huska JA, Keane TM. Unpublished scale available from the National Center for PTSD. 1994. The PTSD checklist (PCL) [Google Scholar]
- Weaver TL, Clum GA. Psychological distress associated with interpersonal violence: A meta-analysis. Clinical Psychology Review. 1995;15:115–140. [Google Scholar]