Abstract
Objective
Purging Disorder (PD), an Other Specified Feeding or Eating Disorder,1 is characterized by recurrent purging in the absence of binge eating. Though objectively large binge episodes are not present, individuals with PD may experience a loss of control (LOC) while eating a normal or small amounts of food. The present study sought to examine the role of LOC eating in PD using archival data from 101 women with PD.
Method
Participants completed diagnostic interviews and self-report questionnaires. Analyses examined the relationship between LOC eating and eating disorder features, psychopathology, personality traits, and impairment, in bivariate models and then in multivariate models controlling for purging frequency, age, and body mass index.
Results
Across bivariate and multivariate models, LOC eating frequency was associated with greater disinhibition around food, hunger, depressive symptoms, negative urgency, and distress and impairment.
Discussion
LOC eating is a clinically significant feature of PD and should be considered in future definitions of PD. Future research should examine whether LOC eating better represents a dimension of severity in PD or a specifier that may impact treatment response or course.
Purging disorder (PD) is an Other Specified Feeding or Eating Disorder characterized by “recurrent purging behavior to influence weight or shape… in the absence of binge eating.”1 The absence of a low body weight distinguishes PD from anorexia nervosa, and the absence of binge-eating episodes distinguishes PD from bulimia nervosa (BN). In the DSM, binge eating is defined by discrete episodes of loss of control (LOC) eating involving the consumption of an unusually large amount of food given context and time (usually two hours).1 LOC eating can be described as feeling unable to stop eating, as though eating were not preventable, or inevitable.2 By definition, women with PD do not have binge episodes; however, women with PD may experience a sense of LOC while consuming an amount of food that is not unusually large. These LOC eating episodes are called subjective binge episodes, contrasting them from the objectively large binge episodes as defined within the DSM. Research studies have varied in requiring3, excluding4,5 or not mentioning LOC eating in definitions of PD,6-8 making it unclear if LOC eating is related to the clinical presentation of PD. This study sought to evaluate the clinical significance of LOC eating in PD because this may have important implications for how PD should be defined within future editions of the DSM.
Across eating disorders, LOC eating includes both subjective and objective binge episodes and is associated with psychopathology and impairment in both community and clinical samples.9-12 Adults with LOC eating report greater eating pathology and general psychopathology than adults without LOC eating.12 Individuals with LOC eating experience greater impulsivity,13 anxiety,11 and depressive symptoms9,11 than those without LOC eating. Additionally, LOC eating is associated with a poorer quality of life.10,14 Based on these findings, LOC eating may be an important clinical feature of PD. However, prior studies of LOC eating across eating disorders do not distinguish the proportions of LOC eating episodes that are objective versus subjective binge episodes, given that LOC eating can include a range in amount of food consumed. Thus, it is uncertain if prior findings apply to LOC eating in PD in which LOC eating is constrained to an amount of food that is not more than what most people would eat.
To address this ambiguity, some prior work has directly examined the role of LOC eating in PD.15-17 In one study of PD, those with LOC eating reported more restraint, eating concern, shape concern, and weight concern than those without LOC eating.17 Additionally, the PD group with LOC eating reported more cognitive impairment and psychological distress than the PD group without LOC eating.17 These findings suggest that LOC eating is associated with a greater severity of illness. However, this sample included women who used purging and nonpurging (i.e., fasting, excessive exercise) compensatory methods, and analyses did not control for purging method or purging frequency. Therefore, this group was broader and more inclusive than PD as defined in the DSM,1 and differences attributed to LOC eating were potentially confounded by an association between LOC eating and use of purging (versus nonpurging) methods or purging frequency. As LOC eating and purging frequencies are correlated,12,18 increased purging, rather than LOC eating frequency, may explain the observed associations. Other work by Mond and colleagues, in which PD was restricted to those who used purging methods, did not find differences between PD with LOC eating and PD without LOC eating,16 suggesting LOC eating may have no effect on the severity of illness when purging methods are held constant. Finally, Brown and colleagues15 found that the frequency of LOC eating in PD was associated with Cluster B personality symptomatology and trait anxiety.15 However, like the studies by Mond and colleagues,16,17 Brown et al.15 did not control for purging frequency when examining associations between LOC eating frequency and personality features. Overall, examination of associations between LOC eating and clinical presentation of PD are inconclusive due to a lack of control for possible confounds.
The current study sought to address the importance of LOC eating in the clinical presentation of PD by examining the relationship between LOC eating frequency and measures of eating pathology, related psychopathology, personality, distress and impairment. To distinguish between correlates of LOC eating episodes and correlates of purging or other key covariates, significant bivariate associations were followed by multivariate models that controlled for key covariates, including purging frequency. Given discrepant findings and the limited literature on LOC eating in PD 15-17, we did not form a priori hypotheses regarding associations. Instead, exploratory analyses provide much needed data on the role of LOC eating in PD. If LOC eating is associated with eating pathology, related psychopathology, personality, and distress and impairment, LOC eating should be considered in defining the syndrome.
Methods
Procedure
Archival data from 101 women from four studies of PD7,19-21 were used for analyses. Participants completed a phone screen and were invited for an interview that was used to confirm eligibility. Although specific participation requirements differed by study, the procedures for the initial study visit were the same, and data for the current study come from diagnostic interviews and questionnaires. All studies required recurrent purging in the absence of objectively large binge episodes in women who were not underweight. To be eligible for inclusion in analyses for the current study, participants had to meet the following inclusion criteria consistent with the DSM-5 diagnosis:1 recurrent purging at least four times a month over the past three months, the undue influence of shape or weight on self-evaluation, normal body weight (BMI range >18.5 to <27 kg/m2), and absence of objectively large binge episodes.
Sample Characteristics
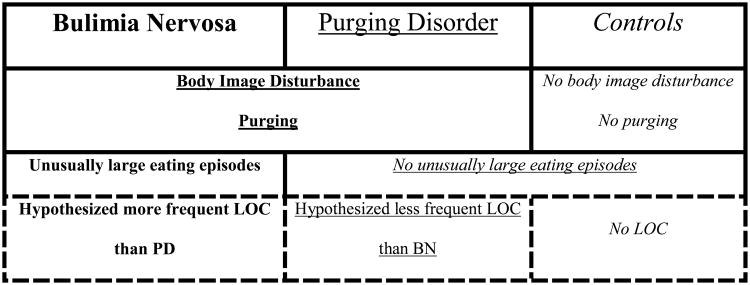
Women ranged in age from 18 to 42 years, with a mean (SD) age of 22.44 (5.27) years. Participants were mostly white (84.2%, n = 85), never married (84.2%, n = 85), and had completed part of college (73.3%, n = 74). Most participants were not currently seeking treatment (71.3%, n = 72), though a majority had sought treatment in their lifetime (59.4%, n = 60). BMI ranged from 18.52 to 26.75 kg/m2 (M = 22.27, SD = 1.94). Most participants reported LOC eating at a frequency of at least 1 time per week (61.4%, n = 62), and 22.8% (n = 23) reported no LOC eating in the past month (see Figure 1). Among those endorsing at least weekly LOC eating, LOC eating occurred on 4.54 (SD = 3.46) times per week. A majority of participants (92.1%, n = 93) reported using self-induced vomiting as a purging method, with 17.8% (n = 18) and 7.9% (n = 8) reporting laxative and diuretic misuse, respectively. These percentages exceed 100% because 17 participants (16.8%) reported the use of multiple purging methods. Participants reported engaging in purging behavior 5.66 (SD = 4.21) times per week.
Figure 1.
Distribution of number of loss of control eating episodes over the past 28 days.
Measures
Although all studies utilized a common assessment protocol for the first study visit, some measures differed across study; thus, sample size varies somewhat by measure.
Eating Pathology
Eating disorder diagnoses were made using the Eating Disorder Examination (EDE)2 in all participants. The EDE is a semi-structured interview that assesses eating disorder symptoms and features. Participants were asked about their largest binge episode to ensure the absence of objectively large binge episodes (<1,000 kcal within two hours).20 Thus, LOC eating involved subjective binge episodes in which participants endorsed feeling a loss of control over their eating, that they could not stop eating, could not prevent the episode from occurring, or that the episode was inevitable. Cronbach's alpha was .83 for total EDE score. Higher scores indicate greater pathology. Across studies, interrater reliability was excellent, with Pearons's r ranging from .996 to 1.0 for total EDE score. Kappa for diagnoses ranged from .91 to 1.0. At the interview, height and weight were measured with a digital scale and wall-mounted ruler. Participants removed shoes and any heavy outerwear or objects (keys, cell phones, etc…) from pockets before weighing but otherwise remained clothed. BMI was calculated in kg/m2.
The Three-Factor Eating Questionnaire (TFEQ)22 served as a self-report measure of eating pathology. The 51-item measure assesses three areas of eating behavior: cognitive restraint of eating, disinhibition around food, and hunger. The TFEQ discriminates between dieters and nondieters.22 The Disinhibition and Hunger subscales have positive associations with binge eating while the Restraint subscale has a negative correlation with binge eating in obese populations.23 In this sample, Cronbach's alpha was .86 for the Restraint, .81 for the Disinhibition, and .84 for the Hunger subscales.
The Body Shape Questionnaire is a 36-item questionnaire that inquires about body shape concerns in the past four weeks.24 Cronbach's alpha was .94 in the current sample. Greater scores indicate greater pathology.
Related Psychopathology and Personality Features
Comorbid psychopathology was assessed using the Structured Clinical Interview for DSM-IV (SCID).25 This semi-structured clinical interview was used to assess lifetime history of mood, anxiety, substance use, and impulse control disorders. Across studies, kappa was 1.00 for mood and substance use disorders, ranged from .76 to 1.00 for anxiety disorders, and ranged from .71 to 1.00 for impulse control disorders. All analyses reflect DSM-IV diagnoses.
The Beck Depression Inventory (BDI)26 is a 21-item measure of the intensity of depressive symptoms and distress. Cronbach's alpha for the current sample was .88.
The State-Trait Anxiety Inventory27 served as a measure of both current anxiety (state) and overall anxiety proneness (trait). Research supports the distinctiveness of the state and trait scales, with test-retest reliability higher in the trait (.91) than state (.73) scale.20 The 40-item instrument has internal consistency measures of .93 for state anxiety and .92 for trait anxiety in the current sample.
The Barratt Impulsiveness Scale (BIS-11) was available for 46 participants. The BIS-11 is a thirty-item questionnaire that assesses the personality construct of impulsivity.28 The BIS-11 differentiates between healthy populations and psychiatric populations.28 Cronbach's alpha was .85 for total score.
The UPPS Impulsive Behavior Scale (UPPS)29 was available for 55 participants. The UPPS is a 45-item scale consisting of four empirically derived factors: urgency, (lack of) premeditation, (lack of) perseverance, and sensation seeking.29 Internal consistency was .87 for urgency, .86 for lack of premeditation, .79 for lack of perseverance, and .92 for sensation seeking.
Distress and Impairment
The Global Assessment of Functioning (GAF) from the SCID25 measures symptom severity and impairment on a scale of 1-100 with anchors for every decile. Higher scores indicate better functioning, less impairment, and lower severity.
The Clinical Impairment Assessment (CIA)30 was available for 55 participants. This 16-item measure assesses impairment due to eating pathology over the past 28 days. Three-day test-retest reliability was .86 in a treatment sample.30 CIA scores were positively correlated with clinicians' rating of impairment, and scores differentiated those with a diagnosed eating disorder and from those who no longer met criteria.30 Cronbach's alpha in the current sample was .88.
Data Analytic Approach
Bivariate correlations were used to assess the relationship between LOC eating frequency in the past 28 days and eating pathology, related psychopathology, personality traits, distress, and impairment. Significant bivariate associations were followed up with separate multiple regression analyses. Logistic regression tested the role of LOC eating frequency as a predictor of presence of lifetime comorbid diagnoses. In all regression analyses, purging frequency over the past 28 days was used as a covariate because previous research indicates a positive relationship between bingeing and purging frequency in eating disorder samples12,18 and because LOC eating and purging were moderately correlated in the current sample (r = .34, p < .001). In addition, study, dummy coded, was used as a covariate to control for differences in eligibility criteria across studies from which participants' data were taken. Data source, rather than variables that differed between samples, was used to control for both observed and unobserved nuisance variables that may have differed between study cohorts. Finally, age and BMI were used as covariates due to their associations with outcome variables (e.g. sensation seeking, shape concerns). LOC eating was not associated with age (r = .07, p = .46) nor with BMI (r = .05, p = .63). The presentation of both bivariate associations and results from regression analyses with covariates permits interpretation of associations both with and without covariates. Missing data were deleted list-wise. Analyses were evaluated with an alpha level of .01 to reduce the likelihood of Type I error.
Results
Table 1 presents bivariate correlations between the predictor variables of LOC eating frequency and covariates and outcome measures of eating pathology, related psychopathology, personality traits, and distress and impairment.
Table 1. Bivariate associations between predictors (loss of control eating frequency and covariates) and eating pathology, related psychopathology, personality traits, and distress and impairment.
| N | Age | BMI | Purging | LOC Eating | |
|---|---|---|---|---|---|
| Restraint | 80 | .08 | -.01 | -.22 | -.22 |
| Disinhibition | 80 | -.05 | .21 | .06 | .35* |
| Hunger | 80 | -.10 | .18 | .03 | .29* |
| BSQ | 99 | .22‡ | .17 | .13 | .21‡ |
| EDE Total | 101 | .21‡ | .16 | -.03 | .20‡ |
| Lifetime Mood Disorders | 101 | .20 | -.07 | .10 | .16 |
| Lifetime Anxiety Disorders | 101 | .06 | -.00 | -.01 | .23‡ |
| Lifetime Substance Use Disorders | 101 | .19 | -.01 | .22‡ | .27* |
| Lifetime Impulse Control Disorders | 101 | .08 | .21‡ | .09 | .32* |
| BDI | 80 | -.03 | .01 | .25‡ | .32* |
| State Anxiety | 97 | -.04 | -.18 | .18 | .17 |
| Trait Anxiety | 96 | -.01 | -.08 | .21‡ | .15 |
| BIS-11 | 46 | .12 | -.06 | -.09 | .07 |
| Negative Urgency | 55 | -.21 | .13 | .09 | .44** |
| Lack Premeditation | 55 | -.07 | .28‡ | -.09 | .25 |
| Lack Perseverance | 55 | -.05 | .18 | .02 | -.06 |
| Sensation Seeking | 55 | -.42** | .15 | .18 | .20 |
| CIA | 55 | .16 | .06 | -.03 | .39* |
| GAF | 99 | -.19 | .15 | -.17 | -.34* |
Note: LOC eating = loss of control eating frequency over the past 28 days; BMI = body mass index; purging = purging frequency over the past 28 days; BSQ = Body Shape Questionnaire; EDE = Eating Disorder Examination; BDI = Beck Depression Inventory; BIS-11 = Barratt Impulsiveness Scale; CIA = Clinical Impairment Assessment; GAF = Global Assessment of Functioning;
p < .05;
p < .01;
p < .001
Eating Pathology
LOC eating frequency was not associated with dietary restraint (p = .05), but did demonstrate a moderate positive relationship with both disinhibition (p =.002) and hunger (p = .008). At a trend level, LOC eating frequency was associated with body shape concerns as measured by the BSQ (p = .04) and with eating disorder severity as measured by the EDE (p = .04). Multivariate models controlling for purging frequency, age, and BMI supported significant associations between LOC eating and disinhibition (β = .40, t(73) = 3.21, p = .002) and hunger (β = .37, t(73) = 2.96, p = .004).
Related Psychopathology
LOC eating frequency was not significantly associated with lifetime mood disorders (p = .11), but was associated with lifetime anxiety disorders at a trend level, p = .02 (see Table 1). In addition, LOC eating frequency was significantly associated with increased prevalence of both lifetime substance use (p = .006) and impulse control disorders (p = .001). LOC eating frequency exhibited a significant positive relationship with current depressive symptoms (BDI; p = .004), but not with current anxiety symptoms (p = .10).
Multivariate logistic regression models controlling for purging frequency, age, and BMI revealed that, at a trend level, LOC eating frequency was associated with greater likelihood of lifetime substance use disorders (adjusted OR = 1.06, 95% CI = 1.01- 1.11, p = .02, N = 101) and lifetime impulse control disorders (adjusted OR = 1.06, 95% CI = 1.01 – 1.11, p = .02, N = 101). In addition, LOC eating remained significantly associated with BDI scores (β = .33, t(79) = 2.70, p = .009), controlling for covariates.
Personality Features
LOC eating was associated with greater negative urgency (p < .001), but not with trait anxiety (p = .15), BIS-11 (p = .64) scores, or other facets of impulsivity including (lack of) premeditation (p = .06), (lack of) perseverance (p = .69), and sensation seeking (p = .51) (see Table 1). Multivariate regression supported that LOC eating remained significantly associated with negative urgency (β = .49, t(49) = 3.92, p < .001), controlling for covariates.
Distress and Impairment
Those who reported more frequent LOC eating endorsed significantly greater eating disorder-related distress and impairment as measured by the CIA (p = .003) and poorer overall functioning as measured by the GAF (p = .001) (see Table 1). In multivariate models controlling for covariates, LOC eating was significantly associated with greater current impairment due to eating disorder symptoms as measured by the CIA (β = .38, t(49) = 2.82, p = .007) and overall functioning and measured by the GAF (β = - .30, t(91) = -2.71, p = .008).
Discussion
Results indicate that LOC eating is a clinically significant feature in PD. LOC eating is associated with disinhibition, hunger, depressive symptoms, negative urgency, distress and impairment above and beyond the effects of age, BMI, and purging frequency in PD. Given these associations, LOC eating within PD appears to be a marker of severity. Thus, assessing frequency of LOC eating in PD would provide highly relevant information in clinical settings and may be considered for inclusion in defining PD in diagnostic systems.
Previous research suggests that binge frequency is associated with disinhibition and hunger,12,23 providing some evidence that correlates of LOC eating are similar between those with DSM-defined binge episodes and those with subjective binge episodes. LOC eating was associated with body shape concerns and eating disorder severity at a trend level. This is in contrast to previous work that found LOC eating in PD was associated with greater body image disturbance and eating disorder severity.17 It may be that we failed to find significant associations because of our stringent p-values to minimize Type I error.
Depressive symptoms have been associated with LOC eating in numerous studies.9,11,12 Our findings both replicate and extend this association for women who do not consume an objectively large amount of food during LOC eating. In contrast to our findings, previous research has indicated that LOC eating was associated with anxiety11,15 whereas we found no association when controlling for purging frequency. Prior research did not control for purging behaviors, which are significantly correlated with anxiety in PD.15 Thus, purging in PD may be more closely associated with anxiety and increased arousal whereas LOC eating may be more closely associated with the combination of lower arousal with negative affect.31 In regards to comorbidity, LOC eating frequency was associated with disorders marked by impulsivity at a trend level. It may be that negative urgency is a vulnerability factor for both LOC eating and problems with substance use,32 gambling,32 and compulsive buying.33
LOC eating was associated with only one dimension of impulsivity: negative urgency. The pattern of associations is consistent with a meta-analysis finding the largest effects size for associations between bulimic symptoms and urgency (r = .40) compared with other aspects of impulsivity, which had smaller effects (r's = .08 - .20)34. Moreover, negative urgency is associated with bulimic symptoms in clinical35 and non-clinical settings,32 and our results suggest that this association is to the experience of LOC during binge episodes. In contrast to findings regarding negative urgency, the present study observed no associations between LOC eating and the BIS-11. Taken together, findings suggest that the facets of impulsivity measured by the BIS-11, (lack of) premeditation, (lack of) perseverance, and sensation seeking may not be related to LOC eating in PD.
This study benefited from a large community-based sample of women with PD and well-validated, multi-method measures of eating pathology, psychopathology, and personality traits. The use of both interview and questionnaire measures aids in reducing error due to relying solely on either method. This was the first study to examine LOC eating in PD controlling for purging frequency as well as other important covariates, allowing a robust test of what is uniquely associated with LOC eating. Results should be interpreted with limitations in mind. These data are cross-sectional, and neither temporal order nor causation can be inferred. Additionally, findings may not generalize to clinical samples. Due to differing recruitment criteria, findings using study as a covariate in combined samples may not reflect what would have been found in a single sample. As such, more research is needed in larger community and clinical samples. Future research should examine LOC eating and its correlates prospectively in order to determine temporal sequence. Understanding temporal sequence may aid in identifying what factors maintain or promote LOC eating. For example, increased negative affect may lead to increased LOC eating or increased LOC eating may lead to increased negative affect. Alternatively, a transactional relationship may exist such that negative affect and LOC eating influence each other over time.
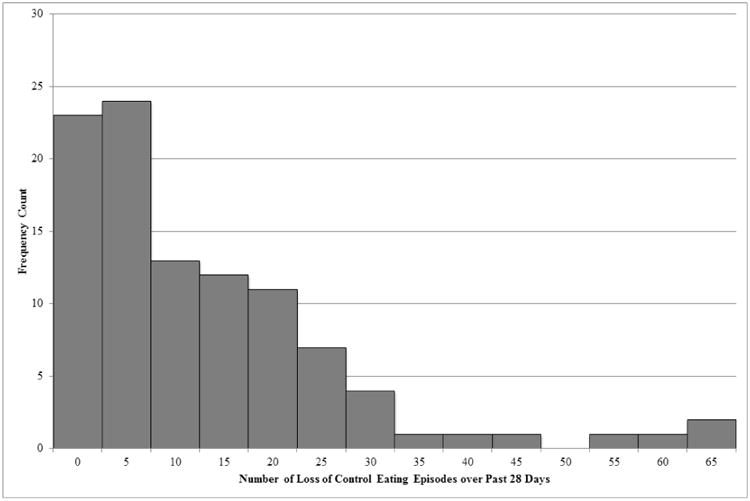
In addition to representing a severity dimension within PD, LOC eating may reflect a severity dimension across bulimic syndromes. When interpreting current findings in the context of patterns of differences previously found between PD, BN, and healthy controls, LOC eating is the only feature that can vary in both presence and frequency among all three groups (see Figure 2). Women with BN may potentially experience more frequent LOC eating than women with PD because women with BN experience both objective binge episodes and subjective binge episodes, women with PD may only experience subjective binge episodes,3,7 and controls, by definition, do not experience LOC eating. Women with BN tend to report more disinhibition,6,7,20 hunger,7,20 depressive symptoms,6-8,36 and impulsivity3,36 than women with PD, who report more disinhibition,6,7,20 hunger,7,20 depressive symptoms,7,8 and impulsivity7,15,36 than controls. As disinhibition, hunger, depressive symptoms, and impulsivity vary in severity across levels of frequency of LOC eating, individual differences in LOC eating may underlie these group differences on these variables.
Figure 2.
Overlapping features of bulimia nervosa, purging disorder, and non-eating disorder controls. Dashed lines represent hypothesized differences. Bold font indicates a feature of bulimia nervosa, underlined font indicates a feature of purging disorder, and italicized font indicates a feature of non-eating disordered controls. Multiple typographies (e.g. type both bolded and underlined) indicate the feature is common to both groups (e.g. bulimia nervosa and purging disorder). LOC = loss of control eating. PD = purging disorder. BN = bulimia nervosa.
This study focused on correlates of LOC eating frequency and suggests that it is a marker of a severity dimension; future research should examine if LOC eating in PD may reflect a specifier. Not all individuals with PD experience LOC eating episodes, and a “with LOC eating” specifier may be indicated in future definitions of PD if LOC eating frequency moderates treatment response. In this case, a specifier may easily and quickly communicate information about severity, eating disorder symptoms, mood, and personality disturbances and would inform treatment. Mixture modeling would establish whether LOC eating loads onto a latent severity dimension, demarcates categorically distinct latent classes, or both.37 Whether LOC eating identifies latent dimension or a latent category, LOC is a significant feature within PD and should be considered in future definitions of the syndrome.
Acknowledgments
This work was supported by R01 MH61836, R03 MH61320 (Keel) and F31 MH085456 (Haedt-Matt) from National Institute of Mental Health. We would also like to thank Dr. Thomas Joiner and Dr. Jon Maner for their thoughtful feedback.
References
- 1.American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th. Arlington, VA: American Psychiatric Association; 2013. [Google Scholar]
- 2.Cooper Z, Fairburn C. The Eating Disorder Examination: A semi-structured interview for the assessment of the specific psychopathology of eating disorders. Int J Eat Disord. 1987;6(1):1–8. [Google Scholar]
- 3.Keel PK, Mayer SA, Harnden-Fischer JH. Importance of size in defining binge eating episodes in bulimia nervosa. Int J Eat Disord. 2001;29(3):294–301. doi: 10.1002/eat.1021. [DOI] [PubMed] [Google Scholar]
- 4.Gauvin L, Steiger H, Brodeur J. Eating-disorder symptoms and syndromes in a sample of urban-dwelling Canadian women: Contributions toward a population health perspective. Int J Eat Disord. 2009;42(2):158–165. doi: 10.1002/eat.20590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Haedt AA, Keel PK. Comparing definitions of purging disorder on point prevalence and associations with external validators. Int J Eat Disord. 2010;43(5):433–439. doi: 10.1002/eat.20712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Roberto CA, Grilo CM, Masheb RM, White MA. Binge eating, purging, or both: Eating disorder psychopathology findings from an internet community survey. Int J Eat Disord. 2010;43(8):724–731. doi: 10.1002/eat.20770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Keel PK, Haedt A, Edler C. Purging disorder: An ominous variant of bulimia nervosa? Int J Eat Disord. 2005;38(3):191–199. doi: 10.1002/eat.20179. [DOI] [PubMed] [Google Scholar]
- 8.Keel PK, Wolfe BE, Gravener JA, Jimerson DC. Co-morbidity and disorder-related distress and impairment in purging disorder. Psychol Med. 2008;38:1435–1442. doi: 10.1017/S0033291707001390. [DOI] [PubMed] [Google Scholar]
- 9.Colles SL, Dixon JB, O'Brien PE. Loss of control is central to psychological disturbance associated with binge eating disorder. Obesity. 2008;16(3):608–614. doi: 10.1038/oby.2007.99. [DOI] [PubMed] [Google Scholar]
- 10.Jenkins PE, Conley CS, Rienecke Hoste R, Meyer C, Blissett JM. Perception of control during episodes of eating: Relationships with quality of life and eating psychopathology. Int J Eat Disord. 2012;45(1):115–119. doi: 10.1002/eat.20913. [DOI] [PubMed] [Google Scholar]
- 11.Shomaker LB, Tanofsky-Kraff M, Elliott C, Wolkoff LE, Columbo KM, Ranzenhofer LM, et al. Salience of loss of control for pediatric binge episodes: Does size really matter? Int J Eat Disord. 2010;43(8):707–716. doi: 10.1002/eat.20767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Latner JD, Hildebrandt T, Rosewall JK, Chisholm AM, Hayashi K. Loss of control over eating reflects eating disturbances and general psychopathology. Behav Res Ther. 2007;45(9):2203–2211. doi: 10.1016/j.brat.2006.12.002. [DOI] [PubMed] [Google Scholar]
- 13.Hartmann AS, Czaja J, Rief W, Hilbert A. Personality and psychopathology in children with and without loss of control over eating. Compr Psychiatry. 2010;51(6):572–578. doi: 10.1016/j.comppsych.2010.03.001. [DOI] [PubMed] [Google Scholar]
- 14.Latner JD, Vallance JK, Buckett G. Health-related quality of life in women with eating disorders: Association with subjective and objective binge eating. J Clin Psychol Med S. 2008;15(2):148–153. doi: 10.1007/s10880-008-9111-1. [DOI] [PubMed] [Google Scholar]
- 15.Brown TA, Haedt-Matt AA, Keel PK. Personality pathology in purging disorder and bulimia nervosa. Int J Eat Disord. 2011;44(8):735–740. doi: 10.1002/eat.20904. [DOI] [PubMed] [Google Scholar]
- 16.Mond JM, Hay P, Rodgers B, Owen C, Crosby R, Mitchell J. Use of extreme weight control behaviors with and without binge eating in a community sample: Implications for the classification of bulimic-type eating disorders. Int J Eat Disord. 2006;39(4):294–302. doi: 10.1002/eat.20265. [DOI] [PubMed] [Google Scholar]
- 17.Mond JM, Hay PJ. Use of extreme weight-control behaviors in the absence of binge eating with and without subjective bulimic episodes: A community-based study. Int J Eat Disord. 2010;43(1):35–41. doi: 10.1002/eat.20667. [DOI] [PubMed] [Google Scholar]
- 18.Edler C, Haedt AA, Keel PK. The use of multiple purging methods as an indicator of eating disorder severity. Int J Eat Disord. 2007;40(6):515–520. doi: 10.1002/eat.20416. [DOI] [PubMed] [Google Scholar]
- 19.Keel PK, Jimerson DC, Haedt-Matt A, Hildebrandt B, McCormick L, McBane A. Satiety deficits and binge eating: Does greater understanding of component processes identify better treatment approaches?. Paper presented at: Society for Research in Psychology; 2012 Oct 4-7; Ann Arbor, MI. [Google Scholar]
- 20.Keel PK, Wolfe BE, Liddle RA, De Young KP, Jimerson DC. Clinical features and physiological response to a test meal in purging disorder and bulimia nervosa. Arch Gen Psychiatry. 2007;64(9):1058–1066. doi: 10.1001/archpsyc.64.9.1058. [DOI] [PubMed] [Google Scholar]
- 21.Matt AAH. unpublished dissertation. Iowa City (IA): The University of Iowa; 2012. Ecological momentary assessment of purging disorder. [Google Scholar]
- 22.Stunkard AJ, Messick S. The Three-Factor Eating Questionnaire to measure dietary restraint, disinhibition and hunger. J Psychosom Res. 1985;29(1):71. doi: 10.1016/0022-3999(85)90010-8. [DOI] [PubMed] [Google Scholar]
- 23.Lowe MR, Caputo GC. Binge eating in obesity: Toward the specification of predictors. Int J Eat Disord. 1991;10(1):49–55. [Google Scholar]
- 24.Cooper PJ, Taylor MJ, Cooper Z, Fairburn CG. The development and validation of the Body Shape Questionnaire. Int J Eat Disord. 1987;6(4):485–494. [Google Scholar]
- 25.First M, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV Axis I Disorders-- patient ed (SCID-I/P) New York: New York State Psychiatric Institute; 1995. [Google Scholar]
- 26.Beck AT, Ward CD, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Arch Gen Psychiatry. 1961;4(6):561–571. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- 27.Speilberger CD, Gorusch RL, Lushene R, Vagg PR, Jacobs GA. The State-Trait Anxiety Inventory. Palo Alto, CA: Consulting Psychologists Press; 1983. [Google Scholar]
- 28.Patton JH, Stanford MS, Barratt ES. Factor structure of the Barratt Impulsiveness Scale. J Clin Psychol. 1995;51(6):768–774. doi: 10.1002/1097-4679(199511)51:6<768::aid-jclp2270510607>3.0.co;2-1. [DOI] [PubMed] [Google Scholar]
- 29.Whiteside SP, Lynam DR. The Five Factor Model and impulsivity: Using a structural model if personality to understand impulsivity. Pers Indiv Differ. 2001;30(4):669–689. [Google Scholar]
- 30.Bohn K, Doll HA, Cooper Z, O'Connor M, Palmer RL, Fairburn CG. The measurement of impairment due to eating disorder psychopathology. Behav Res Ther. 2008;46(10):1105–1110. doi: 10.1016/j.brat.2008.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Heller W, Nitschke JB. The puzzle of regional brain activity in depression and anxiety: The importance of subtypes and comorbidity. Cognition & Emotion. 1998;12(3):421–447. [Google Scholar]
- 32.Fischer S, Smith GT. Binge eating, problem drinking, and pathological gambling: Linking behavior to shared traits and social learning. Pers Indiv Differ. 2008;44(4):789–800. [Google Scholar]
- 33.Williams AD, Grisham JR. Impulsivity, emotion regulation, and mindful attentional focus in compulsive buying. Cognitive Ther Res. 2012;36(5):451–457. [Google Scholar]
- 34.Fischer S, Smith GT, Cyders MA. Another look at impulsivity: A meta-analytic review comparing specific dispositions to rash action in their relationship to bulimic symptoms. Clin Psychol Rev. 2008;28(8):1413–1425. doi: 10.1016/j.cpr.2008.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Anestis MD, Smith AR, Fink EL, Joiner TE. Dysregulated eating and distress: Examining the specific role of negative urgency in a clinical sample. Cognitive Ther Res. 2009;33(4):390–397. [Google Scholar]
- 36.Fink EL, Smith AR, Gordon KH, Holm-Denoma J, Joiner TE. Psychological correlates of purging disorder as compared with other eating disorders: An exploratory investigation. Int J Eat Disord. 2009;42(1):31–39. doi: 10.1002/eat.20556. [DOI] [PubMed] [Google Scholar]
- 37.Keel PK, Crosby RD, Hildebrandt TB, Haedt-Matt AA, Gravener JA. Evaluating new severity dimensions in the DSM-5 for bulimic syndromes using mixture modeling. Int J Eat Disord. 2013;46(2):108–118. doi: 10.1002/eat.22050. [DOI] [PMC free article] [PubMed] [Google Scholar]