Abstract
Synchronous tumours of different histological types involving the salivary gland are very rare. There have been cases reported in the literature of such tumours occurring in the parotid gland. A 52-year-old man presented with a 4-year history of gradually increasing painless swelling in the right submandibular region. The ultrasound scan of the neck showed features suggestive of a submandibular sialadenitis. The right submandibular gland was then surgically excised and sent for histopathological examination. The features showed a unique dual pathology of the submandibular gland, that is, a plasmacytoma and a pleomorphic adenoma. Such a synchronous double pathology involving the submandibular gland has not been reported in the literature. A review of the literature suggests a good prognosis for the extramedullary plasmacytoma, provided multiple myeloma is ruled out. In 18 months of follow-up, the patient has been asymptomatic with a negative myeloma workup.
Background
Salivary gland neoplasms are uncommon. They represent only 2–3% of the head and neck tumours. Salivary gland tumours of different histological types in a single gland are rare. They constitute less than 0.3% of all salivary gland neoplasms.1 2 The most common benign salivary gland neoplasm is a pleomorphic adenoma or a benign mixed tumour,3 with a 50% incidence in the submandibular gland. The most common dual pathology reported is a Warthin's tumour with a pleomorphic adenoma.4 5 There have been cases reported in the literature of a benign and a malignant tumour in the same gland, especially in the parotid gland.1–6 There are no reported cases in the literature of a combination of a plasmacytoma and a pleomorphic adenoma involving the submandibular gland. The diagnosis in this case was made following a complete surgical excision of the gland, which was the surgical treatment modality for both the tumours.
Extramedullary plasmacytomas (EMP) are rare plasma cell tumours of the head and neck region. They constitute less than 4% of the plasma cell tumours.7 They can involve any extramedullary organ or tissue. The most common site is the upper respiratory tract, especially the nose, the paranasal sinuses and the nasopharynx.7–10 Salivary gland EMP, especially of the submandibular gland, has not been commonly reported.7 It is considered as a separate disease entity, and therefore, it is important for the clinician to recognise EMP because of the distinct method of evaluation, treatment and prognosis.8 There is a possibility of progression to multiple myeloma in 10–30% of patients with EMP even though the incidence is much lower than of patients with medullary plasmacytoma.9 10 These patients require a long-term follow-up to rule out multiple myeloma as well as its recurrence.10
Case presentation
A 52-year-old male patient presented to the outpatient department of our tertiary care hospital with a 4-year history of a swelling in the right submandibular region. The swelling was painless and slowly progressive in nature. There was no increase in size of the swelling with intake of food. He had no other comorbid illnesses.
On examination, a 6×3 cm firm, smooth, mobile, non-tender swelling was palpable in the right submandibular region. It was bimanually palpable. The skin over the swelling was normal with no visible pulsations. There were no other swellings, and no lymph nodes were palpable. With the suspicion of a chronic submandibular sialadenitis, further investigations were made.
Investigations
Ultrasound of the neck showed an enlarged submandibular gland with heterogenous echotexture and increased vascularity, suggestive of a submandibular sialadenitis. A fine-needle aspiration cytology (FNAC) of the swelling was carried out which showed a few plasma cells but was inadequate for a definitive diagnosis. The routine blood investigations were normal.
Treatment
An excision biopsy of the right submandibular gland was carried out under general anaesthesia via a right upper cervical incision at the level of the hyoid bone. Intraoperatively, a well-encapsulated nodular mass was seen involving the right submandibular gland which was excised in toto with the entire gland and sent for histopathological examination (figure 1). The single nodular mass measured 6.5×6×4.5 cm, had a bluish appearance and weighed approximately 70 g. The postoperative period was uneventful.
Figure 1.
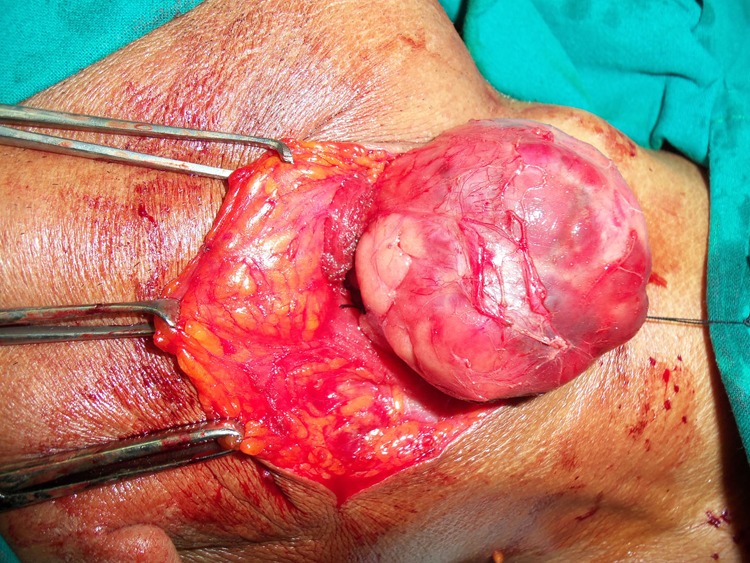
Intraoperative image of the swelling.
Outcome and follow-up
The histopathological examination of the salivary gland showed a partially circumscribed tumour composed of sheets of plasma cells that were pseudocompartmentalised by slender vascular channels (figure 2). The cells had eccentric nuclei with clock face chromatin and perinuclear hof. The tumour was seen infiltrating the adjacent salivary gland tissue. Some cells showed intracytoplasmic (Russel bodies) and intranuclear (Dutcher cells) inclusions. The immunohistochemical studies demonstrated a strong positivity for CD138, confirming a plasma cell origin (figure 3). The adjoining part of the salivary gland showed a small nodule (1×1 cm) which showed features of a pleomorphic adenoma (figure 4).
Figure 2.
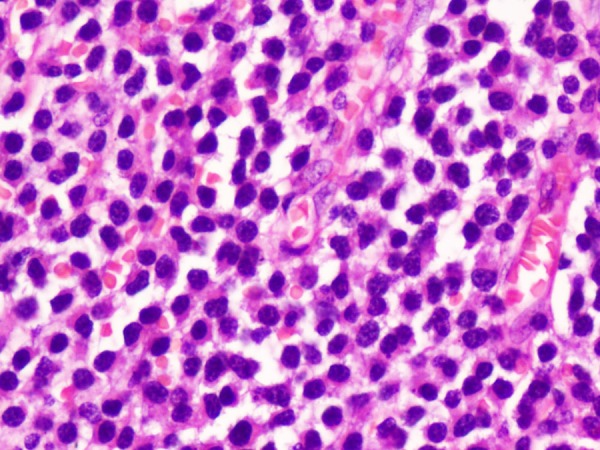
Sheets of plasma cells (H&E, ×400).
Figure 3.
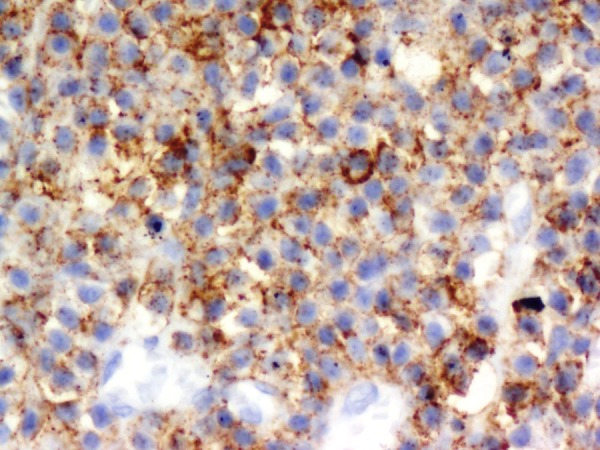
CD138 positivity (×400).
Figure 4.
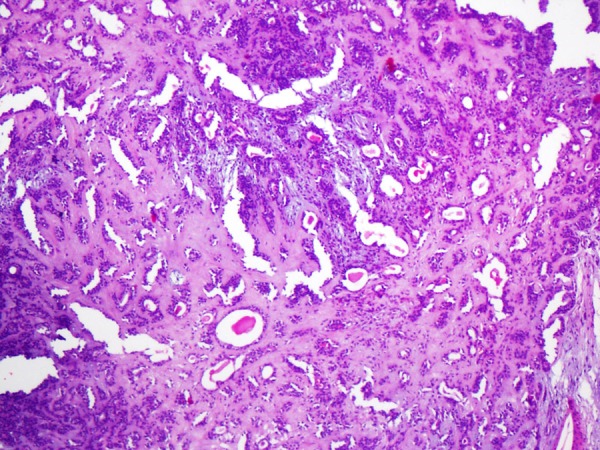
Pleomorphic adenoma (H&E, ×100).
In view of a diagnosis of plasmacytoma, the patient underwent a complete myeloma workup. A complete blood picture including a peripheral smear, serum biochemistry (serum calcium, uric acid, creatinine, serum proteins, liver function tests) and a protein immunoelectrophoresis was carried out. The reports revealed normal results. The urine analysis was negative for Bence-Jones proteins. The bone marrow aspirate and biopsy were normal. Thus, a multiple myeloma was ruled out. The final diagnosis of a solitary EMP with adjoining features of a pleomorphic adenoma of the right submandibular gland was made. The patient has been on follow-up for the past 18 months. The repeat multiple myeloma workup was negative.
Discussion
There have been many cases reported in literature of unilateral synchronous tumours of the parotid gland.1–6 Tanaka and Chen in 1953 were the first to describe a case of synchronous benign and malignant tumours involving the parotid gland.4 The most commonly reported combination is a Warthin's tumour with a pleomorphic adenoma (42%).2–4 Pleomorphic adenoma in combination with other tumours constitute less than 19%.5 In the salivary gland, coexistence of tumours of different histological type is rarely seen. According to Gnepp et al, such tumours constitute less than 0.3% of salivary gland neoplasms. No such synchronous tumours of different histological type have been reported in the submandibular gland.
The combination of a plasmacytoma and pleomorphic adenoma is unusual in the submandibular gland. These two tumours in the same gland are more likely to be two separate entities rather than a benign precursor for a malignant tumour. Pleomorphic adenoma being a benign tumour usually presents as a slow-growing painless swelling, commonly in the parotid gland.6 The treatment of choice is a complete surgical excision of the gland to prevent recurrence. The plasmacytomas, in contrast, are characterised by a neoplastic proliferation of plasma cells which may be medullary or extramedullary in nature.7 EMP may then be primary or secondary depending on whether or not they are associated with multiple myeloma at the time of presentation.7 Multiple myeloma represents the disseminated form of this disease classically characterised by the presence of an abnormal monoclonal protein (M band) in the blood and urine.7 10 Multiple myeloma is the commonest presentation of a plasma cell tumour.10
An EMP constitutes less than 1% of the head and neck tumours.7 9 Men are affected three to four times more than women. These tumours present in the sixth to seventh decade of life.7 Approximately, 80% of these arise in the submucosal tissue of the upper respiratory tract.7 10 Hence, it is important for a clinician to keep in mind plasmacytoma as one of the differential diagnosis for a swelling involving the head and neck region.7 A literature review has shown a better prognosis with an EMP and a lower rate of conversion to multiple myeloma in comparison with a medullary plasmacytoma (10–20%).9–11
The presentation of an EMP depends on its specific location in the head and neck region.7 In our case report, it presented as a non-tender upper neck swelling without any mass effect. The diagnosis of an EMP presents a diagnostic difficulty to the pathologist as well as the clinician.12 13 The diagnosis is usually made by histopathological examination.7 10 11 FNAC is not diagnostic as it fails to yield adequate tissue sample for complete diagnosis by histology or immunohistochemical staining.7 10 It often reveals clumps of plasma cells that may pose to be a diagnostic difficulty for the pathologist as it mimics other lesions such as reactive plasmacytic hyperplasia, plasma cell granuloma, pseudolymphoma and malignancies such as haematopoietic neoplasms, malignant melanoma, olfactory neuroblastoma, anaplastic carcinoma and metastases.7 10 13 The differentiation between plasmacytoma and polyclonal infiltrates of plasma cells can be achieved by biopsy and immunohistochemistry.7 10 Immunohistochemical staining will demonstrate the monoclonality of the plasma cells and can also rule out diseases such as undifferentiated carcinoma, melanoma and esthesioneuroblastomas.7 10 13
Further confirmation of a solitary EMP is required to rule out, by investigations, the presence of a systemic disease, that is, multiple myeloma. A complete myeloma workup includes a complete blood picture, serum biochemistry, protein and urine electrophoresis, a bone marrow aspirate and biopsy and a skeletal survey.7 10 13A negative myeloma workup will establish the diagnosis of a solitary EMP.
The treatment options that have been advocated in the literature for EMP include surgery, radiotherapy or both.7 10–12 Radiotherapy is the treatment of choice for EMP since it is a radiosensitive tumour.12 13 However, for a localised EMP, as in our case, surgery is an ideal option. Most of these tumours can be removed in toto as an excisional biopsy. Surgery can also be advocated for residual disease after radiotherapy.7 10 However, little is available in the literature about surgery as a single modality of treatment for EMP. Radiotherapy can be reserved for treatment failures or for recurrences.7 10 If the disease has disseminated, chemotherapy can be used, although little is known about its efficacy.7 8 11
A long-term follow-up is essential in all these cases to identify not only recurrences but also the progression to a systemic disease.10 12 13 Some authors have detected conversion to multiple myeloma 10–36 years after the initial treatment.10 The prognosis is good when multiple myeloma is ruled out.7 12 13 Approximately 10–30% of the patients with EMP may progress to a multiple myeloma.13
The course and prognosis of a dual pathology largely depends on the histological type of the neoplasm.4 In our case, one of the components was a plasmacytoma which requires a long-term follow-up. Whether pleomorphic adenoma was involved in the pathogenesis of the other is not known yet. Although, pleomorphic adenoma is a benign tumour, there have been reports of metastasis to distant organs. Recurrence of the tumour at the primary site is characteristic of most metastasising pleomorphic adenomas which can be prevented by aggressive surgical removal.14 In our case, as the two tumours were separated by a sizeable amount of normal salivary gland parenchyma, it can be recognised as two separate distinct type of neoplasms in the same gland. Following the complete surgical removal of the gland, our patient was disease free during the 18 months of follow-up.
Learning points.
Synchronous benign and malignant tumours can present in the submandibular gland.
Meticulous histopathological examination is required for the diagnosis.
Surgical excision is the treatment of choice for a localised disease.
Diagnosis of a plasmacytoma requires exclusion of multiple myeloma.
A long-term follow-up is required to recognise conversion to a systemic disease.
Footnotes
Contributors: SM drafted the article and was the principal investigator. KP reviewed the article. MV also reviewed the article and was also the pathologist for this case.
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Curry JL, Petruzelli GJ, McClatchey KD, et al. Synchronous benign and malignant salivary gland tumors in ipsilateral glands: a report of two cases and a review of literature. Head Neck 2002;24:301–6 [DOI] [PubMed] [Google Scholar]
- 2.Gnepp DR, Schroeder W, Heffner D. Synchronous tumours arising in a single major salivary gland. Cancer 1989;63:1219–24 [DOI] [PubMed] [Google Scholar]
- 3.Misselevich I, Podoshin L, Fradish M, et al. Salivary gland double tumor: synchronous ipsilateral pleomorphic adenoma and acinic cell carcinoma of the parotid gland. Ann Otol Rhinol Laryngol 1997;106:226–9 [DOI] [PubMed] [Google Scholar]
- 4.Tanaka S, Tabuchi K, Oikawa K, et al. Synchronous unilateral parotid gland neoplasms of three different histological types. Auris Nasus Larynx 2007;34:263–6 [DOI] [PubMed] [Google Scholar]
- 5.Stavirianos SD, McLean NR, Soames JV. Synchronous unilateral parotid neoplasms of different histological types. Eur J Surg Oncol 1999;25:331–2 [PubMed] [Google Scholar]
- 6.Herce-Lopez J, Salazar-Fernandez CI, Mayorga-Jimenez F, et al. Synchronous unilateral parotid neoplasms. A case report. Med Oral Patol Oral Cir Bucal 2009;14:E90–2 [PubMed] [Google Scholar]
- 7.Shah C, Roy D, Naronha B. Extramedullary plasmacytoma of the submandibular gland. J Laryngol Otol 2001;115:1023–5 [DOI] [PubMed] [Google Scholar]
- 8.Soesan M, Paccagnella A, Chiarion-Sileni V, et al. Extramedullaryplasmacytoma: clinical behaviour and response to treatment. Ann Oncol 1992;3:51–7 [DOI] [PubMed] [Google Scholar]
- 9.Susnerwala SS, Shanks JH, Bannerjee SS, et al. Extramedullary plasmacytoma of the head and neck region: clinicopathological correlation in 25 cases. Br J Cancer 1997;75:921–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Miller FR, Lavertu P, Wanamaker JR, et al. Plasmacytomas of the head and neck. Otolaryngol Head Neck Surg 1998;119:614–18 [DOI] [PubMed] [Google Scholar]
- 11.Kerr PD, Dort JC. Primary extramedullary plasmacytoma of the salivary glands. J Laryngol Otol 1991;105:687–92 [DOI] [PubMed] [Google Scholar]
- 12.Pahor AL. Extramedullary plasmacytoma of the head and neck, parotid and submandibular salivary glands. J Laryngol Otol 1977;91:241–58 [DOI] [PubMed] [Google Scholar]
- 13.Kapadia SB, Desai U, Cheng VS. Extramedullary plasmacytoma of the head and neck: a clincopathologic study of 20 cases. Medicine 1982;61:317–29 [DOI] [PubMed] [Google Scholar]
- 14.Raja V, China C, Masaki KH, et al. Benign metastasizing pleomorphic adenoma. J Clin Oncol 2002;20:2400–3 [DOI] [PubMed] [Google Scholar]


