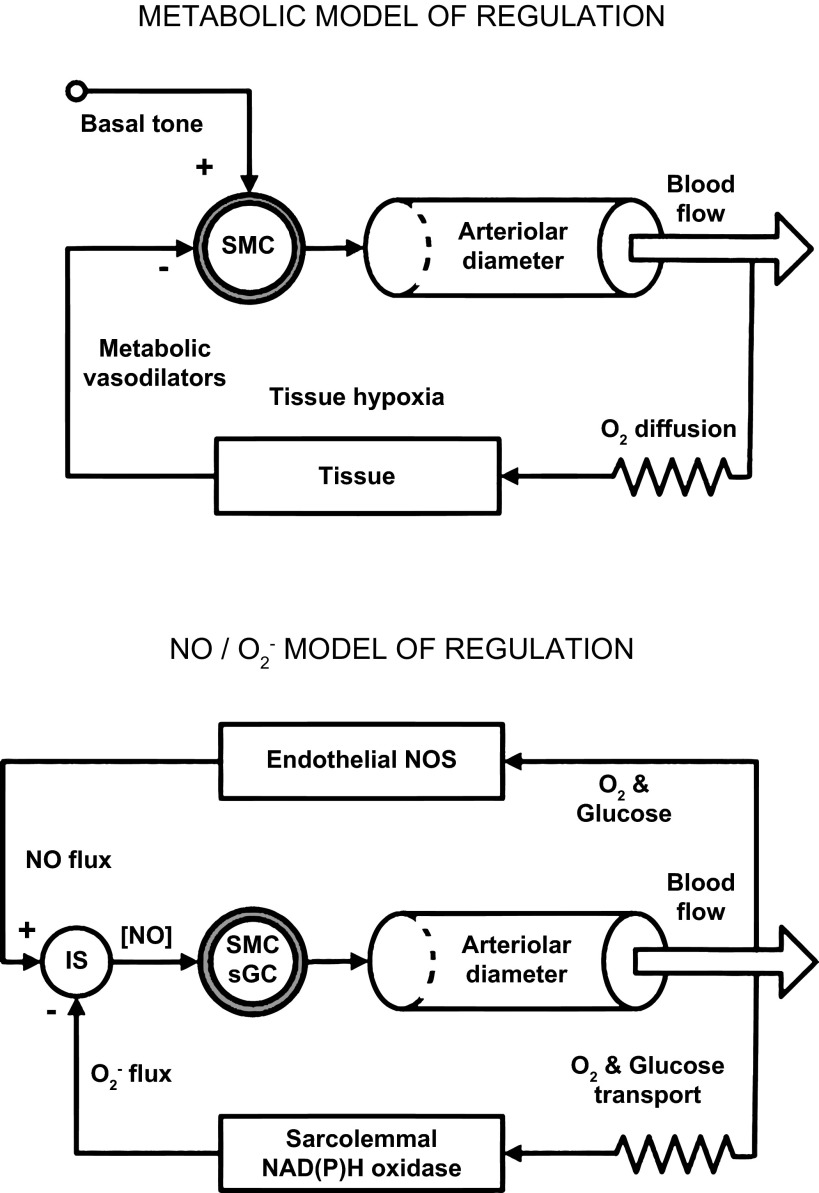
Fig. 1.
Top: metabolic model of regulation. When the O2 supply to a tissue whose activity increases is insufficient to meet the increased O2 demand, tissue hypoxia ensues and metabolic vasodilators are released from the active tissue into the interstitium, where they diffuse to the nearby arterioles, producing a negative feedback signal, causing them to dilate. The increased blood flow brings an elevated oxygen supply that relieves the tissue hypoxia (and the stimulus for producing the vasodilators). Bottom: NO/O2− model of regulation. When O2 and glucose content in the blood is sufficient, eNOS produces a constant flux of NO into the perivascular space. This provides a positive feedback signal for the smooth muscle cells (SMC) of the arteriolar wall. This NO flux serves as a reference signal (“set point”) and is constant if Po2 in the blood is high enough. Transport of O2 and glucose to parenchymal cells is restricted by diffusion and transmembrane glucose transporters. This is presented as a resistor in the diagram. The parenchymal cells and vascular wall are consumers of glucose and O2 and are sensors of their adequate supply. With sufficient or excessive delivery of glucose, the membrane NAD(P)H oxidase is supplied with its substrates NADH and NADPH from the cytosol to generate extracellular O2−. Thus the negative feedback signal reporting the achievement of a high level of supply is encoded as the rate of O2− emission into the interstitial space (IS). The periarteriolar NO concentration ([NO]) in the IS is determined by the interaction of NO and O2− fluxes. The superoxide flux depends on a sufficient supply of O2 and glucose to parenchymal cells, and the NO flux is determined by the high content of oxygen and glucose in blood. The interaction of these fluxes in the interstitial space is similar to the subtraction of part of the NO flux due to its neutralization by superoxide. The result of this subtraction is the error signal, represented as [NO] at the SMCs of the arteriolar wall. These cells serve as a controller of vascular wall tone via the soluble guanylyl cyclase (sGC) pathway, changing the inner diameter and hydraulic resistance of arterioles to adjust the local blood flow. At rest, the perivascular [NO] is low and arterioles are constricted. Activation of oxidative metabolism reduces the production of O2−, thus opening the arterioles with high [NO]. The presence of ecSOD in the interstitium accelerates removal of the residual O2− and accelerates the development of hyperemia.