Abstract
AIM
To determine the causative agents of fungal keratitis and study the predisposing factors over a period of ten years in a single tertiary care hospital.
METHODS
A retrospective analysis of fungal corneal ulcers was done from 2003-2012. Patients' clinical data were noted from the file records. Correlation of histopathological diagnosis was done with the report on fungal culture.
RESULTS
Mycotic keratitis was established in 44 cases by a positive fungal culture. Direct microscopic examination of potassium hydroxide (KOH) mounts revealed fungal elements in 39 cases while 40 cases showed fungus on Gram stained smears. Males (54.55%) were more commonly affected than the females (45.45%). The age ranged from 18 to 82 years. Most common age group to be involved was 41-60 years. Predisposing risk factors were seen in 34 (77.27%) cases. Most common findings on clinical examination were anterior chamber reaction and conjunctival injection seen in all the cases. Other common findings were stromal infiltration and hypopyon seen in 20 (45.45%) and 18 (40.91%) cases respectively. On histopathological examination the fungus was typed, as aspergillus in 34 cases while no definite typing was possible in 10 cases. The predominant isolate was aspergillus flavus (59.09%) followed by fusarium (15.91%). Mixed fungal and bacterial infection was seen in 3 (6.82%) cases.
CONCLUSION
Although culture is the gold standard for definitive diagnosis of fungal keratitis, direct microscopic examination of corneal scrapings or histomorphological evaluation of biopsies allow a rapid preliminary diagnosis. Early administration of antifungal treatment helps in preventing dreadful complications.
Keywords: mycotic keratitis, fungal, culture, infection, cornea
INTRODUCTION
Mycotic keratitis has been reported from many different parts of the world, with a worldwide reported incidence varying from 17% to 36% in various studies[1]. It is particularly common in tropical areas, where the incidence ranges between 14%-40% of all ocular mycoses, or of all cases of microbial keratitis[2]. The incidence in India is 44% to 47%[1]. Fungal corneal ulcer is common in India due to the tropical climate and a large agrarian population that is at risk[3]. Keratomycosis can be caused by as many as 60 species of fungi[4]. The time interval from trauma to clinical features varies depending on the organism, the size of inoculum and host resistance.
Such a corneal infection poses a challenge to the ophthalmologist because of its tendency to mimic other types of stromal inflammation[5]. Mycotic keratitis should be suspected in every patient with a corneal lesion and should be ruled out promptly to save sight and before commencing steroids and antibiotics. Use of empiric antifungal therapy is discouraged and a confirmatory diagnosis is recommended before institution of therapy[6].
The frequency and spectrum of fungi involved varies from place to place as several factors like climate, age, sex, geographical and socioeconomic conditions play a significant role in modulating the incidence and prevalence of fungal corneal infections[7],[8].
Among the important predisposing factors related to corneal ulcer are trauma (generally with plant materials), chronic ocular surface disease, contact lens usage, ocular surgery, corneal anesthetics abuse, diabetes mellitus, vitamin deficiency and immunodeficiencies[9],[10].
For laboratory diagnosis of mycotic keratitis, demonstration of fungal pathogens on direct microscopy and their isolation by culture is essential. Aim of the present study is to determine the etiological agents, predisposing factors and important diagnostic tests in keratomycosis in North India.
SUBJECTS AND METHODS
A retrospective analysis of fungal corneal ulcers was done in the last ten years (2003-2012). A brief clinical history including the history of trauma, occupation and use of topical/systemic antibiotics/corticosteroids were noted from the file records. The corneal tissue received in the pathology department was processed to study the histomorphology. Sections were stained with hematoxylin & eosin. Special stains for fungus, Periodic acid Schiff and Grocott, were done. The morphology of the fungal elements was studied and the typing was done wherever possible. The corneal scrapings sent to the microbiology department were used to prepare a wet mount with 10% potassium hydroxide (KOH). Also, lactophenol cotton blue staining and Gram staining were done and fungal elements were examined under the microscope. Inoculation on Sabourad's dextrose agar and blood agar plates was done at room temperature. The cultures were studied by the microbiologist. A correlation of histopathological diagnosis was done with the fungal culture report.
RESULTS
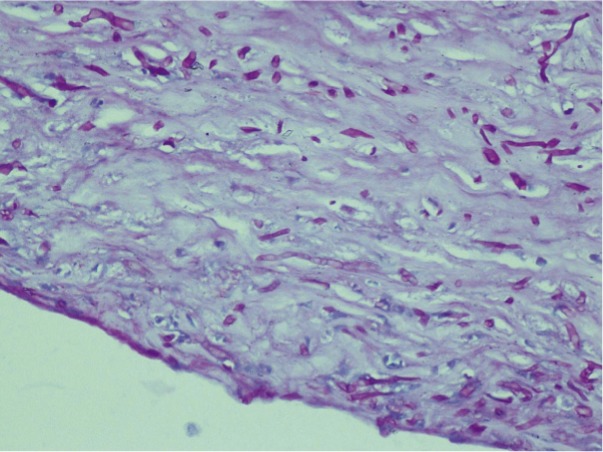
Mycotic keratitis was established in 44 cases by a positive fungal culture. Out of these, 24 were male and 20 were female. The age ranged from 18 to 82 years. Peak incidence of mycotic keratitis was observed in the month of April. Predisposing risk factors were noted in 34 patients. A prior history of trauma was seen in 26 cases. Clinical symptomatology of majority of the patients comprised of redness, watering, photophobia and ocular pain. History of topical antibiotic/steroid usage was seen in 08 cases. Use of contact lenses and prior ocular surgery was not found in any case. Most common findings on clinical examination were anterior chamber reaction and conjunctival injection seen in all the cases (Table 1). Other common findings were stromal infiltration and hypopyon seen in 20 (45.45%) and 18 (40.91%) cases respectively (Figures 1, 2). On histopathological examination septate, slender, branching hyphae were seen in 34 cases where the fungus was typed as aspergillus (Figures 3, 4) while no definite typing was possible in 10 cases.
Table 1. Slit lamp examination findings in mycotic keratitis patients.
| Signs | No. of the patients | % |
| Feathery infiltrate | 05 | 11.36 |
| Satellite lesions | 03 | 6.82 |
| Conjunctival injection | 44 | 100 |
| Immune rings | 01 | 2.27 |
| Endophthalmitis | 01 | 2.27 |
| Epithelial defect | 14 | 31.82 |
| Suppuration | 04 | 9.09 |
| Stromal infiltration | 20 | 45.45 |
| Anterior chamber reaction | 44 | 100 |
| Hypopyon | 18 | 40.91 |
| Vascularisation | 05 | 11.36 |
| Dry looking ulcer | 01 | 2.27 |
| Corneal thinning | 12 | 27.27 |
| Perforation | 10 | 22.73 |
(n=44)
Figure 1. Slit lamp photograph showing 5.5mm×4.5mm fungal corneal ulcer with dense stromal infiltrates, feathery margins, satellite lesions and dense thick immobile hypopyon.
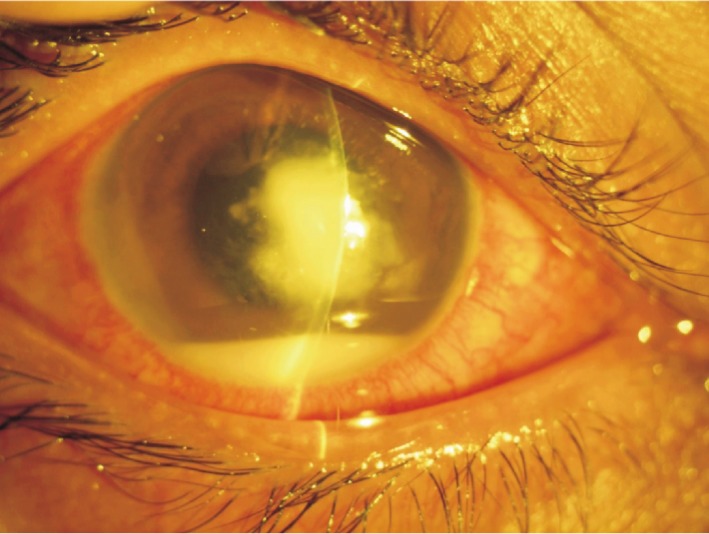
Figure 2. Slit lamp photograph (diffuse) showing fungal corneal ulcer with resolving dense stromal infiltrates with feathery margins.
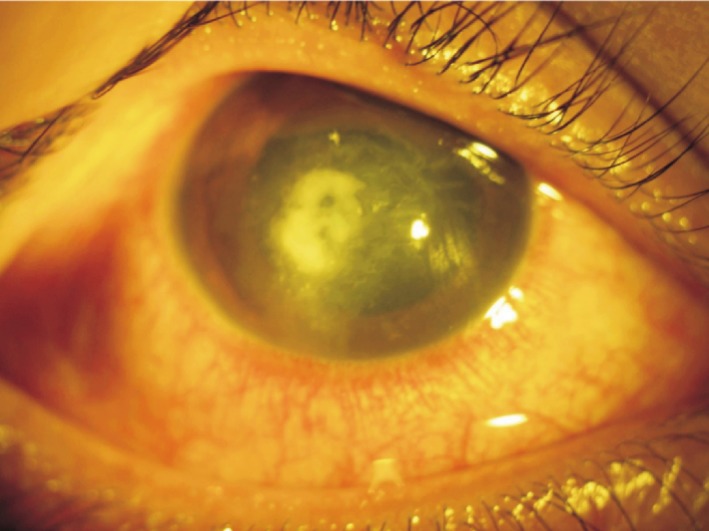
Figure 3. Photomicrograph showing septate slender hyphae in a case of mycotic keratitis (H&E, ×200).
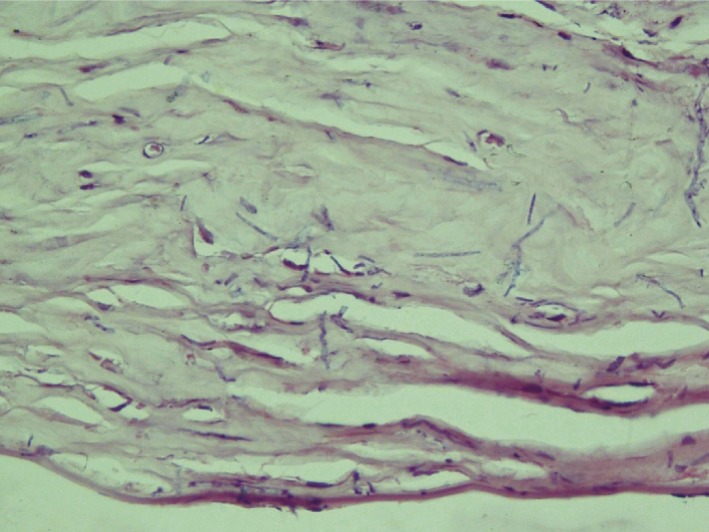
Figure 4. Fungal elements of aspergillus highlighted on periodic acid Schiff staining (PAS, ×200).
Direct microscopic examination of KOH mounts revealed fungal elements in 39 cases while 40 cases showed fungus on Gram stained smears. The KOH mount failed to show any fungal profiles in 05 culture positive cases. The sensitivity of the KOH mounts and Gram stained smears was 88.64% and 90.91%, respectively. The specificity was 98% each. Cases showing fungal elements on histopathology/KOH mounts but with sterile cultures were excluded from the study. Mixed fungal and bacterial infection was seen in three cases. The predominant isolate was aspergillus flavus followed by fusarium (Table 2).
Table 2. Fungal species isolated from corneal ulcer patients.
| Fungal isolate | No. of the patients | % |
| Aspergillus flavus | 26 | 59.09 |
| Fusarium | 07 | 15.91 |
| Aspergillus fumigatus | 05 | 11.36 |
| Rhizopus | 01 | 2.27 |
| Curvularia lunata | 02 | 4.54 |
| Alternaria | 01 | 2.27 |
| Phaeoacremonium parasiticum | 01 | 2.27 |
| Penicillium | 01 | 2.27 |
(n=44)
DISCUSSION
Mycotic keratitis responsible for corneal blindness is the second most common cause of blindness in the developing countries[11]. During many years in the past much emphasis was given to the trachoma diagnosis and treatment. It is only in the recent years that there has been a paradigm shift and stress is being given to fungal keratitis.
Males were affected more commonly than the females, which is usually the case[11],[12]. However, a higher incidence amongst the females is reported in some studies[13]. The disease was more common in the age group of 41-60 years which is in contrast to the observations by Chowdhary and Singh[11] where preponderance was seen between 31-40 years of age. The possible reason could be that our hospital caters to more patients who are from the rural background.
The major risk factors implicated in causation of fungal corneal ulcers include occupational farming, a history of trauma, use of topical/systemic antibiotics or steroids, immunocompromised states and diabetes mellitus[11],[14]. The most common predisposing factor found in our study was trauma to the cornea seen in 26 (59.09%) cases. The agents responsible for trauma were primarily thorns, tree branches and husk. Other studies have also found trauma to be the commonest predisposing factor in the spectrum of fungal keratitis. The percentage of corneal trauma has been reported to be as high as 42% by Chowdhary and Singh[11]. Injudicious use of topical antibiotics/steroids as an implicating factor was seen in 08 (18.18%) cases. Use of contact lenses by wearers practicing poor hygiene is another factor seen mostly in the developed world. Our study had no case with contact lens wear which is in congruence with some studies[3],[15].
On clinical examination mycotic ulcer has a central greyish-white elevated discoid ulcer with irregular fragmented, undermined edges, with a yellow line of demarcation. Satellite infiltrates are seen around the edge of the ulcer. Satellite lesions indicate extension of the fungus. Small sized ulcers may be associated with hypopyon[4]. Hypopyon was seen in 18 (40.90%) and satellite lesions in 03 (6.18%) cases out of total 44 cases in the present study. Fungal endophthalmitis was seen in one case which is usually infrequent and results in poor visual outcomes[16]. Clinical severity of corneal ulcer at presentation is a predictor of worst outcome[17].
A wide variety of fungi have been known to cause keratitis. The commonly implicated ones are aspergillus and fusarium[5],[11],[14],[18]-[22]. Various studies of mycotic keratitis implicate aspergillus species as the commonest incriminant (Table 3)[1],[11],[14],[15],[22]. The present study showed a much wider spectrum of fungi implicated in causation of fungal keratitis. Out of our 44 cases of mycotic keratitis the predominant fungal isolate was aspergillus flavus followed by fusarium. Both aspergillus fumigatus and aspergillus flavus have been almost equally implicated as the causative agents in mycotic corneal ulcers. Curvularia lunata was seen in 2 cases which is in congruence with the low prevalence reported in some studies[15]. A low prevalence of secondary bacterial infection (6.8%) was noted as observed in some studies[14].
Table 3. Comparative studies on mycotic keratitis.
| Place | Author | Year | No. of cases with fungal isolates | Organism 1 | Organism 2 |
| Sari | Shokohi et al[1] | 2004-2005 | 7 | Aspergillus fumigatus | Fusarium spp |
| Rajshahi | Akter et al[14] | 2006-2007 | 33 | Aspergillus fumigatus | Aspergillus flavus |
| Massachusetts | Jurkunas et al[20] | 2004-2007 | 46 | Fusarium spp | Candida albicans |
| Melbourne | Bhartiya et al[21] | 1996-2004 | 56 | Candida albicans | Aspergillus fumigatus |
| Amritsar | Arora et al[22] | 2009 | 40 | Aspergillus | Fusarium |
| Philadelphia | Yildiz et al[23] | 1999-2008 | 76 | Fusarium | Candida |
| Bangalore | Anusuya et al[24] | 2009-2011 | 38 | Fusarium spp | Aspergillus fumigatus |
| New Delhi | Chowdhary et al[11] | 1999-2001 | 191 | Aspergillus spp | Curvularia spp |
| Varanasi | Tilak et al[15] | 2004-2008 | 41 | Aspergillus flavus | Fusarium solani |
| Present study | 2003-2012 | 44 | Aspergillus flavus | Fusarium |
Based on the specific history and findings on clinical examination suggestive of fungal corneal ulcer or smear examination with fungal hyphae, antifungal agents were started. Natamycin (5%) was given hourly followed by ulcer debridement if required in mild superficial mycotic keratitis. In severe and deep mycotic keratitis, freshly prepared amphotericin (0.15%) at hourly intervals was added to the above regime with systemic intraconazole 100mg twice a day (BID) for 2 weeks. Topical drops were continued at least one week more after control of infection. For mixed infections confirmed on culture report, fortified cefazolin drops (5%) with fortified tobramycin (1.4%) were added along with antifungal treatment. If there was no improvement clinically then depending on the sensitivity report, treatment was modified. In recalcitrant cases repeated epithelial debridement was performed to enhance drug penetration. As supportive therapy, atropine 1% twice daily, anti-glaucoma medication; timolol maleate 0.5% BID with tablet vitamin C 500mg BID was given to all the patients. Patients not responding to medical treatment for 1 week or with perforating corneal ulcer underwent therapeutic penetrating keratoplasty.
To conclude, mycotic corneal ulcers are a preventable cause of blindness. They need to be suspected clinically followed by laboratory confirmation. The accurate identification of causative agent helps in planning an appropriate treatment strategy.
Acknowledgments
Conflicts of Interest: Punia RS, None; Kundu R, None; Chander J, None; Arya SK, None; Handa U, None; Mohan H, None.
REFERENCES
- 1.Shokohi T, Nowroozpoor-Dailami K, Moaddel-Haghighi T. Fungal keratitis in patients with corneal ulcer in Sari, Northern Iran. Arch Iranian Med. 2006;9(3):222–227. [PubMed] [Google Scholar]
- 2.Bharathi MJ, Ramakrishnan R, Vasu S, Meenakshi R, Palaniappan R. Epidemiological characteristics and laboratory diagnosis of fungal keratitis. A three-year study. Indian J Ophthalmol. 2003;51(4):315–321. [PubMed] [Google Scholar]
- 3.Nath R, Baruah S, Saikia L, Devi B, Borthakur AK, Mahanta J. Mycotic corneal ulcers in upper Assam. Indian J Ophthalmol. 2011;59(5):367–371. doi: 10.4103/0301-4738.83613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sudan R, Sharma YR. Keratomycosis: clinical diagnosis, medical and surgical treatment. JK Science. 2003;5(1):1–10. [Google Scholar]
- 5.Thomas PA. Fungal infections of the cornea. Eye (Lond) 2003;17(8):852–862. doi: 10.1038/sj.eye.6700557. [DOI] [PubMed] [Google Scholar]
- 6.Sharma S. Diagnosis of fungal keratitis: Current options. Expert Opin Med Diagn. 2012;6(5):449–455. doi: 10.1517/17530059.2012.679656. [DOI] [PubMed] [Google Scholar]
- 7.Chander J. 3rd ed. New Delhi: Mehta Publishers; 2009. Textbook of Medical Mycology; pp. 400–417. [Google Scholar]
- 8.Lin CC, Lalitha P, Srinivasan M, Prajna NV, McLeod SD, Acharya NR, Lietman TM, Porco TC. Seasonal trends of microbial keratitis in South India. Cornea. 2012;31(10):1123–1227. doi: 10.1097/ICO.0b013e31825694d3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Panda A, Satpathy G, Nayak N, Kumar S, Kumar A. Demographic pattern, predisposing factors and management of ulcerative keratitis: evaluation of one thousand unilateral cases at a tertiary care centre. Clin Experiment Ophthalmol. 2007;35(1):44–50. doi: 10.1111/j.1442-9071.2007.01417.x. [DOI] [PubMed] [Google Scholar]
- 10.Shukla PK, Kumar M, Keshava GB. Mycotic keratitis: an overview of diagnosis and therapy. Mycoses. 2008;51(3):183–199. doi: 10.1111/j.1439-0507.2007.01480.x. [DOI] [PubMed] [Google Scholar]
- 11.Chowdhary A, Singh K. Spectrum of fungal keratitis in North India. Cornea. 2005;24(1):8–15. doi: 10.1097/01.ico.0000126435.25751.20. [DOI] [PubMed] [Google Scholar]
- 12.Saha S, Banerjee D, Khetan A, Sengupta J. Epidemiological profile of fungal keratitis in urban population of West Bengal, India. Oman J Ophthalmol. 2009;2(3):114–118. doi: 10.4103/0974-620X.57310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kotigadde S, Ballal M, Jyothirlatha, Kumar A, Srinivasa Rao PN, Shivananda PG. Mycotic keratitis: a study in coastal Karnataka. Indian J Ophthalmol. 1992;40:31–33. [PubMed] [Google Scholar]
- 14.Akter L, Salam MA, Hasan B, Begum N, Ahmed I. Etiological agents of suppurative corneal ulcer: study of 56 cases. Bangladesh J Med Microbiol. 2009;3(2):33–36. [Google Scholar]
- 15.Tilak R, Singh A, Maurya OPS, Chandra A, Tilak V, Gulati AK. Mycotic keratitis in India: a five-year retrospective study. J Infect Dev Ctries. 2010;4(8):171–174. doi: 10.3855/jidc.309. [DOI] [PubMed] [Google Scholar]
- 16.Chhablani J. Fungal endophthalmitis. Expert Rev Anti Infect Ther. 2011;9(12):1191–1201. doi: 10.1586/eri.11.139. [DOI] [PubMed] [Google Scholar]
- 17.Prajna NV, Krishnan T, Mascarenhas J, Srinivasan M, Oldenburg CE, Toutain-Kidd CM, Sy A, McLeod SD, Zegans ME, Acharya NR, Lietman TM, Porco TC. Predictors of outcome in fungal keratitis. Eye (Lond) 2012;26(9):1226–1231. doi: 10.1038/eye.2012.99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ibrahim MM, Vanini R, Ibrahim FM, Fioriti LS, Furlan EMR, Rovinzano LMA, De Castro RS, E Faria E Sousa SJ, Rocha EM. Epidemiologic aspects and clinical outcome of fungal keratitis in southeastern Brazil. Eur J Ophthalmol. 2009;19(3):355–361. doi: 10.1177/112067210901900305. [DOI] [PubMed] [Google Scholar]
- 19.Wang L, Sun S, Jing Y, Han L, Zhang H, Yue J. Spectrum of fungal keratitis in central China. Clin Experiment Ophthalmol. 2009;37(8):763–771. doi: 10.1111/j.1442-9071.2009.02155.x. [DOI] [PubMed] [Google Scholar]
- 20.Jurkunas U, Behlau I, Colby K. Fungal keratitis: Changing pathogens and risk factors. Cornea. 2009;28(6):638–643. doi: 10.1097/ICO.0b013e318191695b. [DOI] [PubMed] [Google Scholar]
- 21.Bhartiya P, Daniell M, Constantinou M, Islam FMA, Taylor HR. Fungal keratitis in Melbourne. Clin Experiment Ophthalmol. 2007;35(2):124–130. doi: 10.1111/j.1442-9071.2006.01405.x. [DOI] [PubMed] [Google Scholar]
- 22.Arora U, Gill PK, Chalotra S. Fungal Profile of Keratomycosis. Bombay Hospital Journal. 2009;51(3):325–327. [Google Scholar]
- 23.Yildiz EH, Abdalla YF, Elsahn AF, Rapuano CJ, Hammersmith KM, Laibson PR, Cohen EJ. Update on fungal keratitis from 1999 to 2008. Cornea. 2010;29(12):1406–1411. doi: 10.1097/ICO.0b013e3181da571b. [DOI] [PubMed] [Google Scholar]
- 24.Anusuya devi D, Ambica R, Nagarathnamma T. The epidemiological features and laboratory diagnosis of keratomycosis. Int J Biol Med Res. 2013;4(1):2879–2883. [Google Scholar]


