Abstract
To investigate the alteration of c-Jun N-terminal kinase (JNK) activity after myocardial ischemia reperfusion injury (MIRI) and further explore the effect of naloxone postconditioning on MIRI. Forty male Sprague Dawley rats were randomly divided into five groups: sham operation (sham, n=8); ischemia reperfusion (IR, n=8); IR+naloxone 0.5 mg/kg (Nal L, n=8); IR+naloxone 1.0 mg/kg (Nal M, n=8); IR+naloxone 2.0 mg/kg (Nal H, n=8). Pathological changes of myocardial tissue were visualized by HE staining. The expression of p-JNK, and the apoptosis of cardiomyocytes were investigated with Western blotting and the TUNEL assay, respectively. Irregular arrangement and aberrant structure of myocardial fibers, cardiomyocytes with granular or vacuolar degeneration, and inflammatory cells infiltrating the myocardial interstitial regions characterized MIRI in the IR group. Signs of myocardial injury and inflammatory infiltration were less prominent in the Nal-treated groups. The expression of p-JNK in the sham group and in all Nal-treated groups was significantly lower than that in the IR group (p<0.01). The apoptosis index of cardiomyocytes in the IR group was significantly higher than in the sham group (p< 0.01). The apoptosis indices of cardiomyocytes in all Nal-treated groups were significantly reduced to 55.4%, 26.2%, and 27.6%, respectively, of the IR group (p< 0.01). This study revealed that Naloxone postconditioning before reperfusion inhibits p-JNK expression and decreases cell apoptosis, thus alleviating MIRI.
Keywords: Cell apoptosis, c-Jun N-terminal kinases (JNK), Ischemia reperfusion, Naloxone
INTRODUCTION
Among human diseases cardiovascular disease is a condition associated with the highest mortality rates, ischemic heart disease being the most prevalent diagnose [1]. Coronary occlusion may cause myocardial necrosis in the region of blood supply and aberrant heart function. The mortally affected cardiac muscle can be rescued by reopening infarct arteries and recovering the blood supply in ischemic tissue. Among the established methods are thrombolytic therapy, coronary angioplasty, and artery bypass grafting. Afterwards the cardiac function can be improved, however, reperfusion can trigger harmful pathophysiological responses and promote cell apoptosis. These side effects are known as myocardial ischemia reperfusion injury (MIRI).
To alleviate or remove reperfusion injury is a challenge to the clinician. Ischemic postconditioning (IPostC) was confirmed to protect heart and brain [2-4], but has been found difficult to conduct clinically. As an exogenous intervention, pharmacological postconditioning presented similar endogenous protective mechanism as IPostC. Pharmacological postconditioning has demonstrated many advantages, including predictability, controllability, safety, and convenient operation, suggesting that it can be used to clinically prevent ischemia reperfusion injury [5-7]. Naloxone is an opioid receptor antagonist and postconditioning with naloxone can alleviate focal cerebral ischemia reperfusion injury in rats [8] and ischemic acute kidney injury in the mouse [9]. Our previous study indicated that naloxone can relieve MIRI [10]. Herewith we present further research results that may add to the elucidation of the underlying mechanisms. We used three different dosage of naloxone (0.5, 1.0, 2.0 mg/kg) to investigate the relationship between dosage and response.
The c-Jun NH2-terminal kinase (JNK) signaling is an important element in mitogen-activated protein kinase (MAPK) signaling and has been shown to be involved in multiple physiological and pathological progressions. It has not reported yet whether naloxone postconditioning alleviates MIRI by affecting JNK signaling. In this study, the effect of naloxone postconditioning on JNK expression and activity after MIRI was investigated using a rat MIRI model. The findings on the protective mechanism can provide the experimental foundation for myocardial protection under ischemia reperfusion.
METHODS
Animals
The adult male Sprague Dawley (SD) rats ranging from 230 g to 270 g were provided by the experimental animal center of Xuzhou Medical College (Jiangsu, China; SYXK [Su] 2002-0038).
Reagents and apparatus
Naloxone hydrochloride (lot number: 0801171) was purchased from Beijing Hua Su Pharmaceutical Co. Ltd. A one-step terminal deoxynucleotidyl transferase dUTP nick end labeling (TUNEL) kit was obtained from Beyotime Institute of Biotechnology (Jiangsu, China). The primary antibodies specific for JNK and p-JNK were purchased from Cell Signal (USA). A refrigerated centrifuge (model 5804R) and a PowerPac™ HC vertical electrophoresis apparatus were obtained from Eppendorf (Germany) and Bio-Rad (USA), respectively. A LMS-2B dual-trace physiological recorder, an ALC-V8 artificial animal respirator, and a BX51 fluorescence microscope were purchased from Chengdu Instrument Factory (Sichuan, China), Shanghai Alcott Biotech Co. Ltd (Shanghai, China), and Olympus (Japan), respectively.
Test groups and treatments
Forty rats were randomly divided into five groups as follows: 1) sham operation (sham, n=8); 2) ischemia reperfusion (IR, n=8); 3) IR plus low-dose naloxone (Nal L, 0.5 mg/kg; n=8); 4) IR plus medium-dose naloxone (Nal M, 1.0 mg/kg; n=8); 5) IR plus high-dose naloxone (Nal H, 2.0 mg/kg; n=8). Rats in the sham group and in the IR group received equal volumes of physiological saline/normal saline while rats in the Nal groups received naloxone by a tail intravenous injection 10 min before reperfusion.
Establishment of myocardial ischemia reperfusion model
Rats were anesthetized with an intraperitoneal injection of 10% chloral hydrate at a dose of 3.5 ml/kg and fixed at supine position. The electrocardiogram (ECG) was observed using an LMS-2B dual-trace physiological recorder. The skin was slit at the center of the neck and the muscle was bluntly separated. The trachea was exposed and cut and the animal respirator was connected to the trachea. Respiratory support was given during the whole experiment. The skin was cut along the midclavicular line for 2 cm and the third rib was snipped. The pleura and pericardium were opened and the thymus was separated. The left anterior descending (LAD) of the coronary artery within the cardiac muscle guided by the vena coronaria sinistra was found between the auricula sinistra and the pulmonary conus. A 5-0 type atraumatic suture needle was passed by the myocardial surface, which was 2 cm below the root of the auricula sinistra, and the needle was withdrawn at the lateral pulmonary conus. By ligating the LAD 30 min, ischemia was produced followed by reperfusion of the myocardium for 2 h. The significant fall of ST segment of the ECG was selected as the reperfusion criterion. Rats in the sham group underwent the same surgical procedures except that the suture placed under the LAD was not tied.
Sample preparation
After the reperfusion rats were sacrificed by exsanguinating at the abdominal aorta and the left ventricular tissue was obtained. Half of the myocardial tissue was fixed using 10% formaldehyde solution and the paraffin-embedded sections were prepared. Another half of the myocardial tissue was washed with cold saline and stored at -80℃.
Protein extraction and Western blot analysis
The samples were ground with RIPA buffer and the mixture was centrifuged at 10,000 g for 15 min at 4℃. The supernatants were stored at -20℃ and the protein concentration was determined by Lowry assay. Totally, 100 µg of proteins were separated using 12% sodium dodecyl sulfate polyacrylamide gel electrophoresis (SDS-PAGE). The proteins were transferred to nitrocellulose membranes. After blocking with 5% BSA in Tris-buffered saline buffer, the membranes were then incubated overnight at 4℃ with primary antibodies. After five times washing for 3 min with washing buffer the membranes were incubated with secondary antibodies at a ratio of 1:1000 at room temperature for 2 h. After another five times washing for 3 min with washing buffer the membranes were shown by NBT/BCIP. The protein bands were scanned and quantified using Image J software. The relative expression of p-JNK was obtained by comparing the optical densities between target protein and β-actin.
Microscopy of myocardium
The paraformaldehyde-fixed myocardial tissues were embedded in paraffin, sliced into 4 µm thick sections, and stained with hematoxylin and eosin (HE). Immunostaining was performed on paraffin sections using a microwave-based antigen retrieval technique. The morphological changes of myocardial tissue were observed using a microscope.
Detection of apoptotic cardiomyocytes
Deoxynucleotidyl transferase-mediated dUTP nick end labeling (TUNEL) assay was performed on sections of paraffin-embedded tissue samples using an ApopTag Plus Peroxidase in situ Apoptosis Detection Kit (Chemicon, Temecula, CA). In summary, after digestion (5 mg/ml working strength Proteinase K, 15 min at room temperature) and quenching (3% H2O2 in methanol, 30 min) steps, equilibration buffer was applied directly to the sections for 5 min, and working strength TdT enzyme (at a concentration of 1:5 in reaction buffer) was then applied for 1 h at 37℃. Positive nuclei were visualized by applying peroxidase-conjugated anti-digoxigenin antibody for 30 min, followed by a 0.05% solution of 3,3'-diaminobenzidine tetrahydrochloride for 4 min. For negative controls, TdTenzyme was omitted. Slides were counterstained with methylene blue. For each myocardial, the number of apoptotic cardiomyocytes in 10 non-overlapping renal cortical fields was counted under ×400 magnification. The number of TUNEL-positive nuclei was averaged for each field. Myocardial apoptosis was represented as apoptosis index (AI) calculated as follows: AI=number of TUNEL-positive myocytes/total number of myocytes.
Statistical analysis
Data were presented as mean±standard deviation (SD) and analyzed using Statistical Product and Service Solutions (SPSS) version 13.0. Inter-group comparison was done by one-way analysis of variance (one-way ANOVA). Correlation analysis was performed using curve estimation. Differences were considered significant statistically when p<0.05.
RESULTS
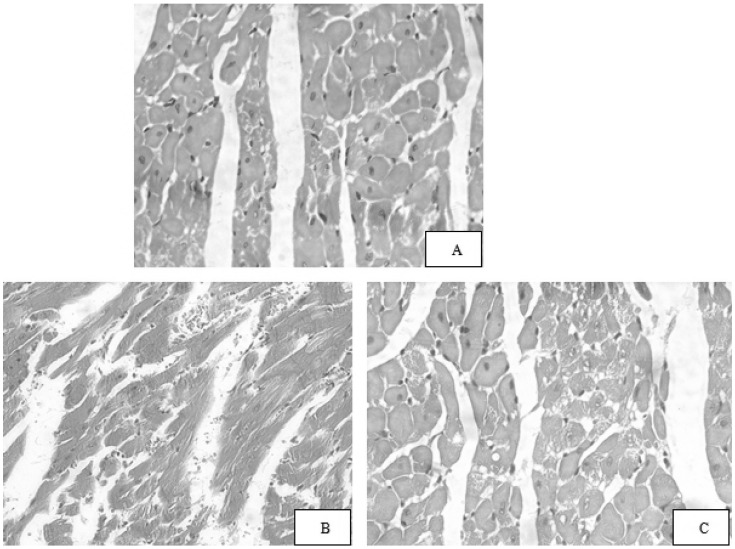
Pathological and morphological effects of naloxone postconditioning on MIRI rats
The myocardial structure of rats in the sham group was arranged regularly. The cells presented with normal size, clear boundaries and even coloration (Fig. 1A). The structure of myocardial fibers in the IR group presented aberrantly and in wavy arrangement. The cells were stained unevenly, some cardiomyocytes showed granular or vacuolar degeneration (Fig. 1B). The cardiomyocytes in Nal-treated groups, especially in the high- and medium-dose groups, presented with mild edema. Few cells showed granular degeneration (Fig. 1C).
Fig. 1.
Pathological and morphological effects of naloxone postconditioning on MIRI rats (HE staining, ×400). (A) Sham group, (B) IR group, (C) Nal M group. Sham group, shamoperated control group; IR, 30 min ischemia prior to 2 h reperfusion; Nal M, medium-dose naloxone group (1.0 mg/kg).
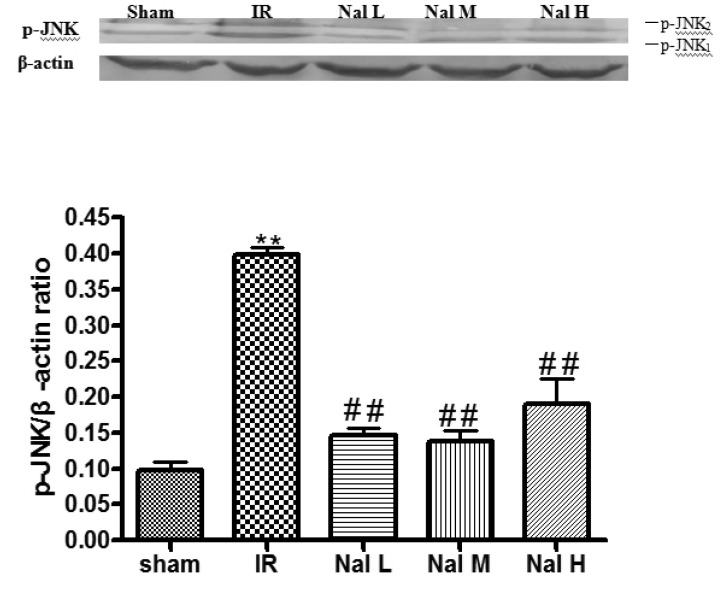
Effect of naloxone postconditioning on JNK and p-JNK protein expression in myocardial tissue of MIRI rats
JNK and p-JNK presented as two bands in each treatment group. They located at 46 kDa (p-JNK1) and 54 kDa (p-JNK2), respectively. The sham group showed weak p-JNK expression. p-JNK expression in the IR group was significantly higher than in the sham group (p<0.01). The p-JNK expression in the Nal L, Nal M, and Nal H groups significantly decreased to 47.6%, 34.5%, and 36.9% of the expression in the IR group, respectively (p<0.01). No significant difference was observed among these three naloxone-treated groups (p>0.05; Table 1 and Fig. 2).
Table 1.
Effect of naloxone postconditioning on p-JNK expression of MIRI rats (mean±SD, n=8)
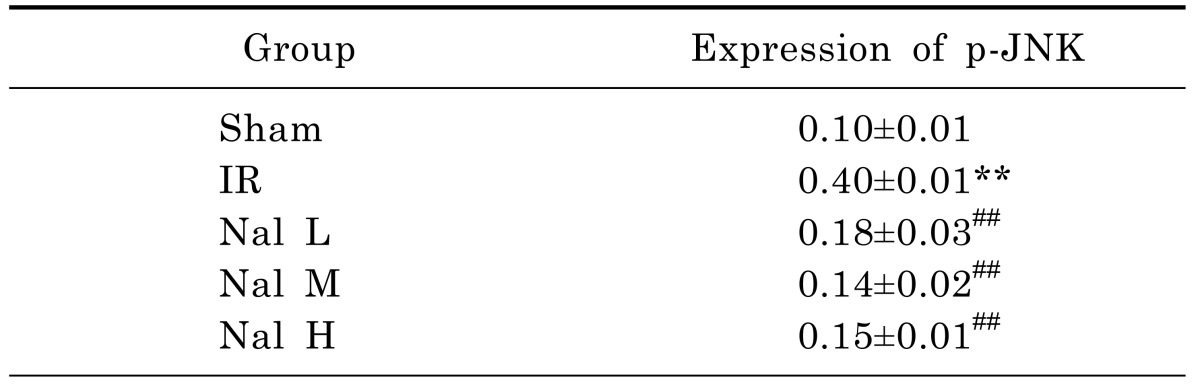
**Compared with sham group, p<0.01; ##Compared with IR group, p<0.01.
Fig. 2.
Effect of naloxone postconditioning on p-JNK protein expression of MIRI rats. **Compared with sham group: p<0.01; ##Compared with IR group: p<0.01. Sham group:sham-operated control; IR, 30 min ischemia prior to 2 h reperfusion; Nal L, Low-dose naloxone group (0.5 mg/kg); Nal M, Medium-dose naloxone group (1.0 mg/kg); Nal H, High-dose naloxone group (2.0 mg/kg).
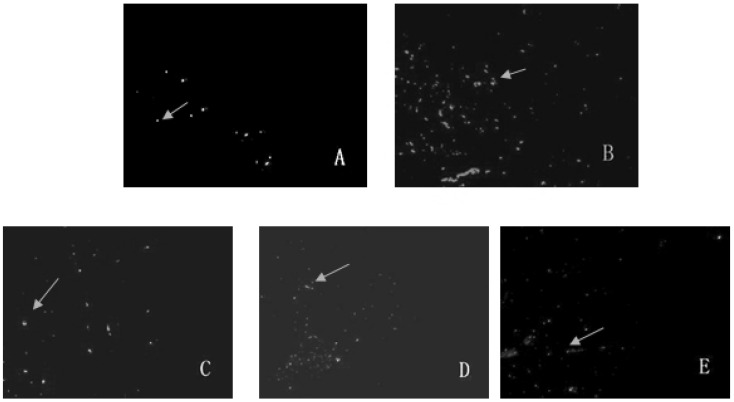
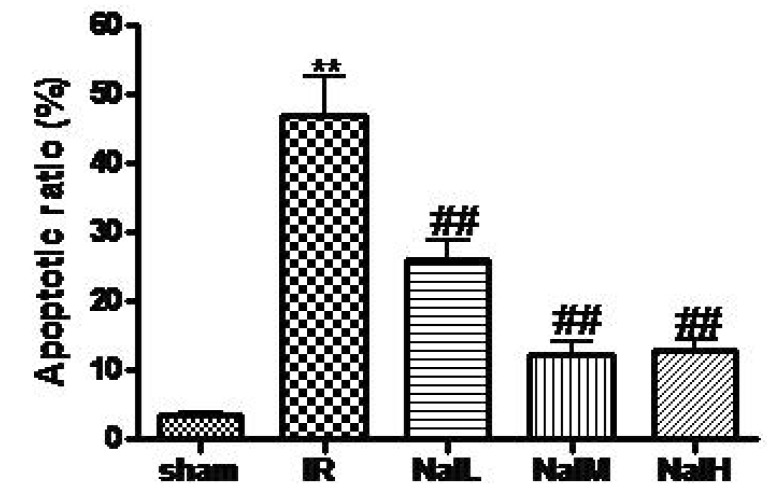
Effect of naloxone on myocardial apoptosis in MIRI
More apoptotic nuclei were found in myocardial tissue of the IR group than in that of the sham group. Apoptotic cells in the Nal L, Nal M, and Nal H groups significantly decreased. The AI of the Nal L, Nal M, and Nal H groups were significantly lower than the one of the IR group, i.e. 55.4%, 26.2%, and 27.6% of the AI of the IR group, respectively (p<0.01; Table 2 and Fig. 3 and 4).
Table 2.
Effect of naloxone postconditioning on cell apoptosis of MIRI rats (mean±SD, n=8)
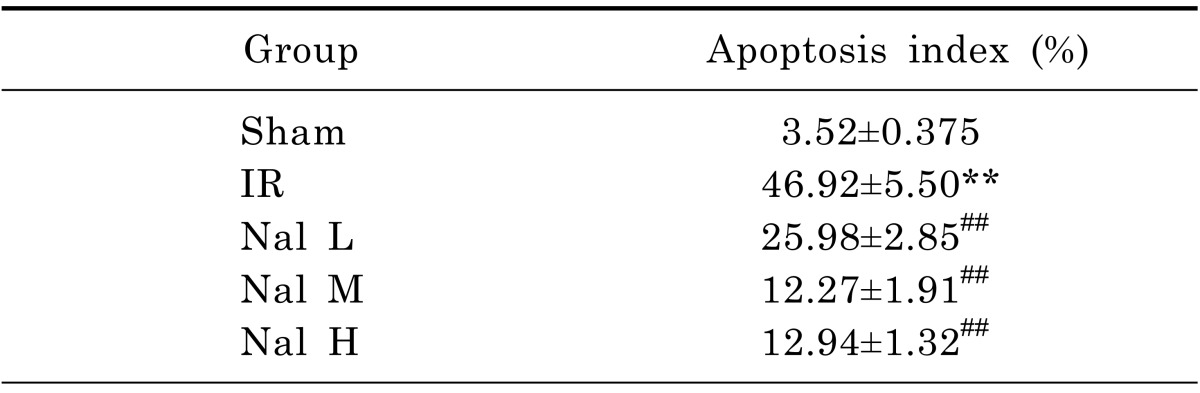
**Compared with sham group: p<0.01; ##Compared with IR group: p<0.01.
Fig. 3.
Effect of naloxone postconditioning on cell apoptosis of MIRI rats (×200). (A) Sham group, (B) IR group, (C) Nal L group, (D) Nal M group, (E) Nal H group. Sham group, sham-operated control; IR, 30 min ischemia prior to 2 h reperfusion; Nal L, Low-dose naloxone group (0.5 mg/kg); Nal M, Medium-dose naloxone group (1.0 mg/kg); Nal H, High-dose naloxone group (2.0 mg/kg).
Fig. 4.
Effect of naloxone postconditioning on the apoptosis indices of MIRI rats (mean±SD, n=8). **Compared with sham group: p<0.01; ##Compared with IR group: p<0.01. Sham, Sham-operated control; IR, 30 min ischemia prior to 2 h reperfusion; Nal L, Low-dose naloxone group (0.5 mg/kg); Nal M, Medium-dose naloxone group (1.0 mg/kg); Nal H, High-dose naloxone group (2.0 mg/kg).
Correlation between p-JNK expression and cardiomyocyte apoptosis
The correlation between p-JNK expression and cell apoptosis was examined by means of relevance analysis using the optical density of p-JNK and AI. A positive correlation between p-JNK and AI was demonstrated using curve estimation analysis (r=0.934; p<0.01).
DISCUSSION
Apoptosis is the programmed death of cells under physiological or pathological conditions, it was demonstrated that cell apoptosis plays an important role in MIRI [11]. It is well established that mitogen-activated protein kinase (MAPK) family members are involved in the induction of myocardial apoptosis in response to IR stimulation. It has been demonstrated that myocardial ischemia/reperfusion activates the two 'stress-responsive' MAPK subfamilies, namely, c-Jun N-terminal kinases (JNK) and p38 mitogen-activated protein kinases (p38-MAPKs), resulting in apoptosis. While p38-MAPK is activated by ischemia and this activation state is maintained during reperfusion, activation of JNK occurs only during reperfusion [12]. It was reported that JNK was activated at 1 min after reperfusion, the activation lasting for 3 h. The specific nuclei alterations related to cell apoptosis and chromatin breakage were observed suggesting that JNK signaling played a regulatory role in ischemia reperfusion injury, especially in cell apoptosis [13,14]. Actived JNK (p-JNK) was shown to promote cell apoptosis via multiple pathways. It can bind to the N-terminals of two transcriptional factors, ATF-2 and c-Jun, leading to phosphorylation of the active domains. ATF-2 and c-Jun can bind activator protein-1 (AP-1) and/or AP-1-like sites that are located on the promoters of many genes. The effect is an increase in the transcriptional activity of AP-1. Also, gene expression and protein synthesis can be promoted, and the proteins may promote cell apoptosis by acting on a certain link of the cell apoptosis pathway [15,16].
In our study, p-JNK protein expression was markedly upregulated and cell apoptosis indices dramatically increased in the IR group as compared with the sham group (p<0.01). Moreover, the cell apoptosis indices showed significantly positive correlation with p-JNK expression suggesting that JNK signaling was involved in the cardiomyocyte apoptosis induced by IR.
Pharmacological postconditioning plays a protective role by modulating endogenous protection mechanism between ischemia and reperfusion. Pharmacological postconditioning can be easily performed and it showed an important clinical application value. Naloxone is an antagonist of opioid receptors, i.e. it can specifically antagonize opioids and endogenous opioids, endorphins and enkephalins. It greatly contributed to basic research on antagonistic action of opioid receptors due to its high affinity to opioid receptors [17]. Furthermore, naloxone can reverse and break the toxicity of endogenous opioid peptides. It was confirmed that naloxone plays a substantial protective role in brain and renal ischemia-reperfusion injuries [8,9].
Furthermore, naloxone protected the reperfused cardiac muscle by inhibiting lipid peroxidation and release of inflammatory mediators and by improving the energetic metabolism [18,19]. In this study, p-JNK expression and cell apoptosis were significantly lower in ischemia-reperfusion myocardial tissues after naloxone treatment when compared with the IR group (p<0.01). Moreover, naloxone postconditioning can significantly improve the pathological injury of ischemia cardiac muscle.
In summary, JNK activation was involved in MIRI and cell apoptosis, and naloxone postconditioning protected the myocardium by inhibiting the activation of JNK and cardiomyocyte apoptosis, thus alleviating MIRI. Neverthless, many researchers have demonstrated that opioid agonist such as remifentanil [20,21] could protect against myocardial ischemia reperfusion injury. This interesting phenomenon may explain from two terms below: 1) there are many kinds of opioid receptors, such as ε,δ,µ,κ,σ, etc. Different receptors involve in different pharmacological effects, and which effect is prodominate has not been elucidated clearly yet [22]. 2) Kinds of animals and different experimental protocols may result in opposite results.
Our study primarily demonstrated that naloxone postconditioning can effectively protect the cardiac muscle against ischemia-reperfusion injury. Naloxone is a commonly used medicine, characterized by a low price and a few side effects. Hence, naloxone may produce huge economic and social benefit if extensively used for clinical prevention of MIRI.
ACKNOWLEDGEMENTS
This study was supported by a grant from the Bureau of Science and Technology, Xuzhou, China (XM08C117).
ABBREVIATIONS
- MIRI
myocardial ischemia reperfusion injury
- IPostC
ischemic postconditioning
- JNK
c-Jun NH2-terminal kinase
- MAPK
mitogen-activated protein kinase
- p38-MAPK
p38 mitogen-activated protein kinases
- TUNEL
terminal deoxynucleotidyl transferase dUTP nick end labeling
- IR
ischemia reperfusion
- LAD
left anterior descending
References
- 1.Sekikawa A, Horiuchi BY, Edmundowicz D, Ueshima H, Curb JD, Sutton-Tyrrell K, Okamura T, Kadowaki T, Kashiwagi A, Mitsunami K, Murata K, Nakamura Y, Rodriguez BL, Kuller LH. A "natural experiment" in cardiovascular epidemiology in the early 21st century. Heart. 2003;89:255–257. doi: 10.1136/heart.89.3.255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zhao ZQ, Corvera JS, Halkos ME, Kerendi F, Wang NP, Guyton RA, Vinten-Johansen J. Inhibition of myocardial injury by ischemic postconditioning during reperfusion: comparison with ischemic preconditioning. Am J Physiol Heart Circ Physiol. 2003;285:H579–H588. doi: 10.1152/ajpheart.01064.2002. [DOI] [PubMed] [Google Scholar]
- 3.Zhu M, Feng J, Lucchinetti E, Fischer G, Xu L, Pedrazzini T, Schaub MC, Zaugg M. Ischemic postconditioning protects remodeled myocardium via the PI3K-PKB/Akt reperfusion injury salvage kinase pathway. Cardiovasc Res. 2006;72:152–162. doi: 10.1016/j.cardiores.2006.06.027. [DOI] [PubMed] [Google Scholar]
- 4.Zhang W, Miao Y, Zhou S, Jiang J, Luo Q, Qiu Y. Neuroprotective effects of ischemic postconditioning on global brain ischemia in rats through upregulation of hippocampal glutamine synthetase. J Clin Neurosci. 2011;18:685–689. doi: 10.1016/j.jocn.2010.08.027. [DOI] [PubMed] [Google Scholar]
- 5.Penna C, Pasqua T, Perrelli MG, Pagliaro P, Cerra MC, Angelone T. Postconditioning with glucagon like peptide-2 reduces ischemia/reperfusion injury in isolated rat hearts: role of survival kinases and mitochondrial KATP channels. Basic Res Cardiol. 2012;107:272. doi: 10.1007/s00395-012-0272-6. [DOI] [PubMed] [Google Scholar]
- 6.Glembotski CC, Thuerauf DJ, Huang C, Vekich JA, Gottlieb RA, Doroudgar S. Mesencephalic astrocyte-derived neurotrophic factor protects the heart from ischemic damage and is selectively secreted upon sarco/endoplasmic reticulum calcium depletion. J Biol Chem. 2012;287:25893–25904. doi: 10.1074/jbc.M112.356345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chen S, Liu J, Liu X, Fu Y, Zhang M, Lin Q, Zhu J, Mai L, Shan Z, Yu X, Yang M, Lin S. Panax notoginseng saponins inhibit ischemia-induced apoptosis by activating PI3K/Akt pathway in cardiomyocytes. J Ethnopharmacol. 2011;137:263–270. doi: 10.1016/j.jep.2011.05.011. [DOI] [PubMed] [Google Scholar]
- 8.Liu Y, Liao X, Xue FS, Xu YC, Xiong J, Yuan YJ, Wang Q, Liu JH, Zhao JX. Effects of combined ischemic postconditioning, remote ischemic postconditioning and naloxone postconditioning on focal cerebral ischemia-reperfusion injury in rats. Zhonghua Yi Xue Za Zhi. 2011;91:1493–1497. [PubMed] [Google Scholar]
- 9.Mutoh J, Ohsawa M, Hisa H. Effect of naloxone on ischemic acute kidney injury in the mouse. Neuropharmacology. 2013;71:10–18. doi: 10.1016/j.neuropharm.2013.03.001. [DOI] [PubMed] [Google Scholar]
- 10.Zhang T, Zhou WD, Xia AZ, Gu SL. Effect of p38 MAPK on naloxone alleviating myocardial ischemia reperfusion injury in rats. West China J Pharm Sci. 2011;26:460–462. [Google Scholar]
- 11.Gottlieb RA, Burleson KO, Kloner RA, Babior BM, Engler RL. Reperfusion injury induces apoptosis in rabbit cardiomyocytes. J Clin Invest. 1994;94:1621–1628. doi: 10.1172/JCI117504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ferrandi C, Ballerio R, Gaillard P, Giachetti C, Carboni S, Vitte PA, Gotteland JP, Cirillo R. Inhibition of c-Jun N-terminal kinase decreases cardiomyocyte apoptosis and infarct size after myocardial ischemia and reperfusion in anaesthetized rats. Br J Pharmacol. 2004;142:953–960. doi: 10.1038/sj.bjp.0705873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hori M, Nishida K. Oxidative stress and left ventricular remodelling after myocardial infarction. Cardiovasc Res. 2009;81:457–464. doi: 10.1093/cvr/cvn335. [DOI] [PubMed] [Google Scholar]
- 14.Jiang CM, Xu CQ, Mi Y, Li HZ, Wang R, Li WM. Calcium-sensing receptor induced myocardial ischemia/reperfusion injury via the c-Jun NH2-terminal protein kinase pathway. Acta Cardiol Sin. 2010;26:102–110. [Google Scholar]
- 15.Matsumoto N, Imamura R, Suda T. Caspase-8- and JNK-dependent AP-1 activation is required for Fas ligand-induced IL-8 production. FEBS J. 2007;274:2376–2384. doi: 10.1111/j.1742-4658.2007.05772.x. [DOI] [PubMed] [Google Scholar]
- 16.Lee SE, Lim JW, Kim H. Activator protein-1 mediates docosahexaenoic acid-induced apoptosis of human gastric cancer cells. Ann N Y Acad Sci. 2009;1171:163–169. doi: 10.1111/j.1749-6632.2009.04716.x. [DOI] [PubMed] [Google Scholar]
- 17.Setoguchi D, Kakihana Y. Naloxone. Masui. 2013;62:5–9. [PubMed] [Google Scholar]
- 18.Zhou P, Dong CL, Niu RX, Wu JX, Li YH. The effects of naloxone in free oxygen radical during myocardial ischemia-reperfusion period. J Med Res. 2008;37:56–57. [Google Scholar]
- 19.Qin YH, Shen H, Yang YS, Wen TB, Li TD. Naloxone inhibits generation of IL-8 and TXA2 from Ischemic and reperfused myocardium. Pharmaceutical J Chin People's Liberation Army. 2008;24:23–25. [Google Scholar]
- 20.Wong GT, Li R, Jiang LL, Irwin MG. Remifentanil postconditioning attenuates cardiac ischemia-reperfusion injury via kappa or delta opioid receptor activation. Acta Anaesthesiol Scand. 2010;54:510–518. doi: 10.1111/j.1399-6576.2009.02145.x. [DOI] [PubMed] [Google Scholar]
- 21.Zhang Y, Irwin MG, Wong TM. Remifentanil preconditioning protects against ischemic injury in the intact rat heart. Anesthesiology. 2004;101:918–923. doi: 10.1097/00000542-200410000-00017. [DOI] [PubMed] [Google Scholar]
- 22.Weber TP, Raufbake C, Grosse Hartlage MA, Rolf N, Stypmann J, Van Aken H, Berendes E, Meissner A. Naloxone prevents increased atrial natriuretic peptide release during regional myocardial ischaemia and stunning in awake dogs. Br J Anaesth. 2002;88:87–93. doi: 10.1093/bja/88.1.87. [DOI] [PubMed] [Google Scholar]