Abstract
Background/Aims:
Pneumatic dilatation (PD) is one of the effective treatments of achalasia. The aim of this study was to evaluate the efficacy of pneumatic dilation and patient satisfaction in Saudi achalasia patients.
Patients and Methods:
We have retrospectively recruited patients with confirmed achalasia, who underwent at least one dilatation session from January 1990 to January 2010 at a single tertiary center. Symptoms, including weight loss, dysphagia, retrosternal pain, and regurgitation, were assessed with the use of the Eckardt score (which ranges from 0 to 12, with higher scores indicating more pronounced symptoms). All patients were called and asked about their Eckardt score in addition to their satisfaction score post the dilatation procedure. The primary outcome was therapeutic success (Eckardt score ≤ 3) and patient satisfaction at the time of their calls. The secondary outcomes included the need for retreatment and the rate of complications.
Results:
A total of 29 patients were included, with a mean age of 40.30 (95% CI: 36.1-44.6) and 55.2% of them were males. The mean of the pre-dilatation Eckardt score was 8.3 (95% CI: 7.2-9.4), which dropped to 2.59 (95% CI: 1.7-3.5) after PD (P < 0.01) with a clinical remission of 76.7% after the first dilatation and a total failure in two patients (7%) after the third dilatation. The mean number of dilatations was 1.3 (95% CI: 1.1-1.5) where 50.7% required one dilatation, 19.2% required two dilatations, and 30.1% required three dilatations. The mean of the symptoms-free period was 53.4 months (SD 52.7, range 1-180) with symptoms recurring in 35% of patients within 2 years. The mean of post-PD patient satisfaction was 7.45 (95% CI: 6.2-8.7). Perforation, which was treated conservatively, occurred in one patient (3.5%), whereas bleeding occurred in two patients (7%). Age or gender was not found to be a predictor of Eckardt score improvement on multivariate linear regression analysis.
Conclusion:
PD is an efficacious procedure in Saudi achalasia patients with a very good overall patient satisfaction with 53.4 months of symptoms-free period after a successful dilatation.
Keywords: Achalasia, dilatation, eckdart score, esophagus, pneumatic dilatation
Achalasia is an esophageal motor disorder that is characterized clinically by dysphagia, chest pain, and regurgitation of undigested food. These symptoms result from the absence of esophageal peristalsis combined with a defective relaxation of the lower esophageal sphincter.[1] Currently, treatment consists mainly of endoscopic pneumatic dilation (PD) or laparoscopic Heller's myotomy (LHM). For many years, repeated endoscopic pneumatic dilation has been the treatment of choice, leading to therapeutic success in 70%-80% of cases.[2] Although the debate about the long-term efficacy of pneumatic dilatation remain, comparing pneumatic dilation to laparoscopic myotomy, Boeckxstaens et al. have recently showed no difference in symptoms or LES pressures in 200 patients at 2 years and suggest that graded dilation starting with a 30-mm balloon is a reasonable protocol for pneumatic dilation.[3] In this study, the rate of therapeutic success with pneumatic dilation was 90% after 1 year of follow-up and 86% after 2 years, as compared with a rate with LHM of 93% after 1 year and 90% after 2 years (P = 0.46).
There are no reported data about clinical characteristics or efficacy of pneumatic dilatation in Saudi achalasia patients. The aim of this study was to evaluate the long-term efficacy of pneumatic dilatation in Saudi achalasia patients and to identify their satisfaction post-PD.
PATIENTS AND METHODS
Study population
Records of achalasia patients at King Khalid University Hospital between 1990 and 2010 were identified through our endoscopy reports. The inclusion criteria were patient age 18 years or older with achalasia confirmed by manometry and those who underwent at least one single session of pneumatic dilatation (PD). The exclusion criteria were a prior esophageal or gastric surgery or insufficient chart data or patients who could not be contacted or refused to participate. Unfortunately, a large number of patients either opted to be excluded, or fulfilled the exclusion criteria. The diagnosis of achalasia was made on the basis of the absence of peristalsis and on impaired relaxation of the lower esophageal sphincter (nadir pressure of ≥ 10 mmHg during swallow-induced relaxation) on esophageal manometry. The following were recorded: Patients’ demographics, clinical symptoms, and details of therapeutic procedures (PD), including size of the balloon, number of PDs, and complications.
Cross-sectional follow-up evaluation
In May 2012, to determine clinical response or recurrence and patient satisfaction, a cross-sectional evaluation was performed by using a structured telephone interview. The interview included questions about the Eckardt score variables at the time of the call and the patients were asked about their level of satisfaction. Eckardt score is the sum of the symptom scores for dysphagia, regurgitation, and chest pain (with a score of 0 indicating the absence of symptoms, 1 indicating occasional symptoms, 2 indicating daily symptoms, and 3 indicating symptoms at each meal) and weight loss (with 0 indicating no weight loss, 1 indicating a loss of <5 kg, 2 indicating a loss of 5-10 kg, and 3 indicating a loss of >10 kg).[4] Thus, the maximum score on the Eckardt scale, indicating the most pronounced symptoms, is 12; patients were considered to have reached clinical remission if the total symptom score was ≤ 3. A symptom score >3 defined recurrence or failure to achieve clinical remission. Patient's post-PD satisfaction was rated according to a scale from 0 to 10 where 0 was not satisfied at all and 10 was very much satisfied.
Pneumatic dilation
Upper endoscopy was performed under conscious sedation. A Rigiflex balloon passed over a guidewire that was centered across the gastroesophageal junction under fluoroscopy or directly under endoscopy guidance and distended to 7-12 psi (to obliterate the waist) for 60 s. The smallest balloon (30 mm) was used first. For failures, a 35-mm balloon was used after at least 4 weeks, followed by a 40-mm balloon if necessary. The Institutional Review Board approved the study protocol in September 2011.
Statistical analysis
All patients who did not answer their calls or refused to participate in the study were excluded from the analysis. Categorical variables were compared with the use of the Chi-square test. Continuous variables are presented as means (with 95% confidence intervals) and were compared with the use of Student's t test. A P < 0.05 was considered statistically significant.
RESULTS
Eighty-five achalasia patients who had undergone pneumatic dilatation were reviewed. Fifty-six of them were excluded for these reasons: Incomplete data or refusal to participate in the study. A total of 29 patients were included, with a mean age of 40.30 (95% CI: 36.1-44.6), 55.2% of them were males. All patients presented with dysphagia (mean was 3.9 pre-dilatation which was dropped to 1.8 post-dilatation post PD, P < 0.01), 55.5% complained of daily regurgitation, 44.8% of patients lost more than 10 kg, 24.1% complained of daily heartburn and 20.7% complained of daily chest pain [Table 1].
Table 1.
Patients’ pre-dilatation characteristics
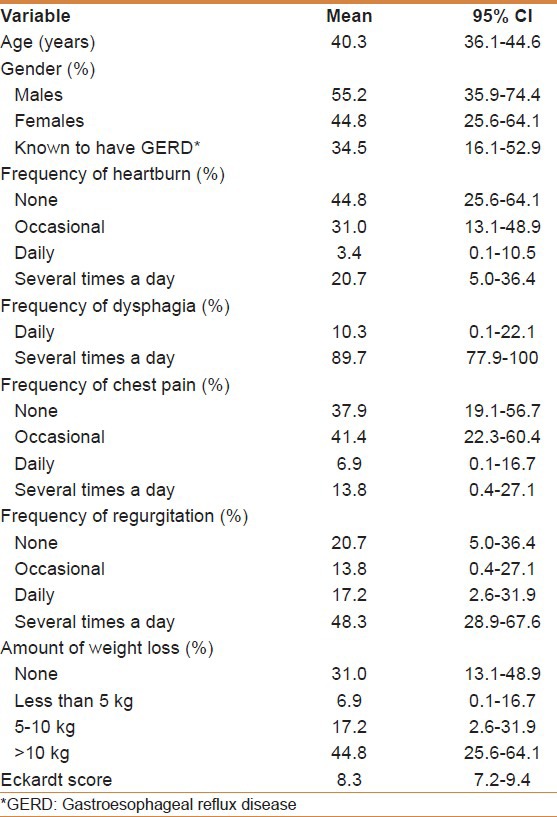
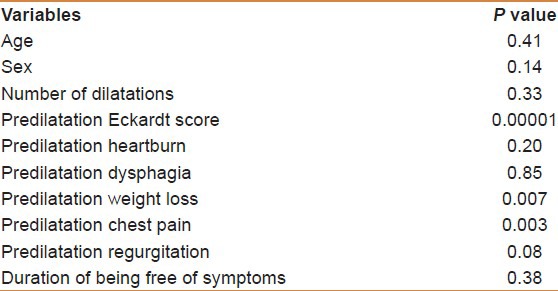
The mean of the pre-dilatation Eckardt score was 8.3 (95% CI: 7.2-9.4), which dropped to 2.59 (95% CI: 1.7-3.5) after PD (P < 0.01) with a clinical remission of 76.7% after the first dilatation and a total failure in two patients (7%) after the third dilatation [Table 2]. The mean number of dilatations was 1.3 (95% CI: 1.1-1.5), 50.7% required one dilatation, 19.2% required two dilatations, and 30.1% required three dilatations. The mean of the symptoms-free period was 53.4 months (SD 52.7, ranges 1-180) with symptoms recurring in 35% of patients within 2 years [Figure 1]. The mean of post-PD patient satisfaction was 7.45 (95% CI: 6.2-8.7) [Table 3]. Perforation, which happened after the first dilatation (35 mm) and was treated conservatively, occurred in 1 patient (3.5%), whereas minor bleeding occurred in two patients (7%). Neither age (above 40 years) nor gender was found to be a predictor of Eckardt score improvement on multivariate linear regression analysis [Table 4].
Table 2.
Clinical outcomes after pneumatic dilatation
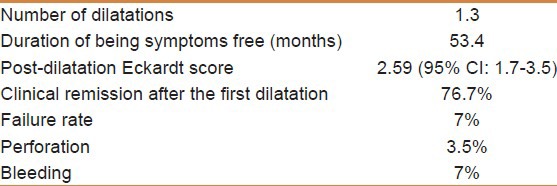
Figure 1.
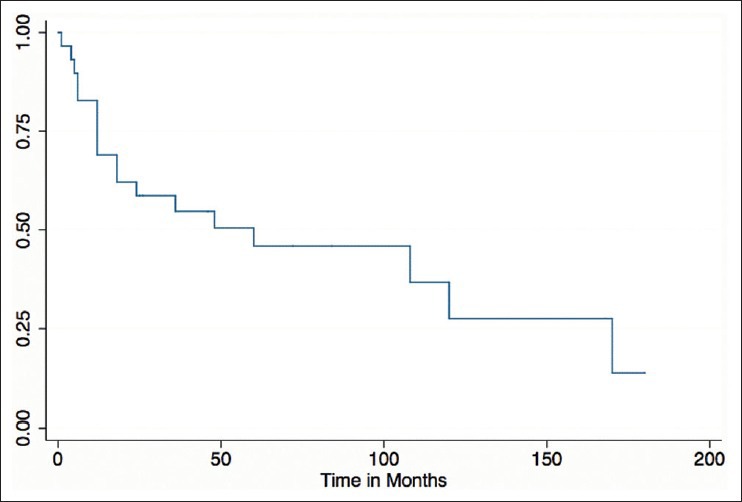
Symptoms-free period after pneumatic dilatation
Table 3.
The mean satisfaction score postdilatation stratified by symptoms
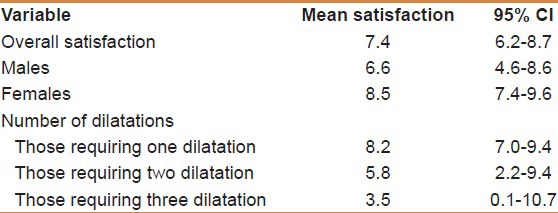
Table 4.
Predictors of improvement in Eckardt score on univariable linear regression
DISCUSSION
Pneumatic dilation and surgical myotomy are recommended as the most appropriate treatment choices to obtain long-term responsiveness.[1,5] Controlled trials that support this notion are almost nonexistent, which is mainly attributable to the low incidence of this disorder. Multiple trials have compared these methods, with different success rates, although the superiority between them is not well established. In a multicenter trial comparing PD to LHM, Boeckxstaens et al. had concluded that these two treatment modalities had equivalent therapeutic success after 2 years.[3] Yet, the long-term durability of either procedure is difficult to extrapolate.
Using a reduction in Eckardt symptom score to 3 or less as the criterion for treatment success, we found a very good success rate after one single PD (76.7%), which reached 93% after three dilatations with a long-term remission of 50% (a mean of 53.4 months of symptoms-free period) and an overall excellent satisfaction rate after PD. Although, the sample size was small, this is the first study addressing the efficacy and the patient satisfaction after PD in achalasia patients among Arabs. Among 209 patients (111 men; mean age, 51.2) with achalasia who were treated with three consecutive PD up to 40 mm, Huselmans et al. found that PD yielded good to excellent outcomes in 72% of patients after 70-month of follow up and treatment satisfaction in more than 80% of patients.[6] In this study, the effectiveness of treatment was evaluated by using a different method, symptom-based Vantrappen criteria, which describe treatment outcomes as excellent when the patient is completely free of symptoms and poor outcome when symptoms occur more than once a week, accompanied by weight loss or regurgitation.[7] In another long-term follow up study published by Karamanolis et al., 51% of their patients continued to be in clinical remission more than 15 years after the initial PD but it was obvious that the long term success rate of PD seems to drop progressively with time.[8] Again, to evaluate the effectiveness of PD, they have used a different grading system. Consistent with our findings, Allescher et al. have reported that 45% of patients treated successfully by PD were still symptom-free after 48 months.[9] Their study was a prospective one and had a sample size (n = 14). However, Kadakia and Wong reported a success rate of 79% with a mean follow up of 47 months,[10] and Katz et al. showed that even after a mean follow up of 6.5 years, PD was still successful in 85% in 72 patients.[11] This figure contrasts with the findings of West et al. who reported a success rate of 40% in patients treated more that 15 years ago.[12] The discrepancy between the success rates can be attributed mainly to the criteria used to define success. In particular, if efficacy is defined as the lack of need for any subsequent intervention, the success rate with pneumatic dilation is much lower than that with surgery. The use of repeated dilations to treat recurrent symptoms is, however, a generally accepted strategy in clinical practice and leads to excellent control of symptoms, even during long-term follow-up. In a meta-analysis of randomized controlled treatment trials for achalasia, Wang et al. showed that there were significant differences in remission rate (laparoscopic myotomy 95.0% vs. pneumatic dilation 77.8%, P = 0.001) and relapse rate (laparoscopic myotomy 5.1% vs. pneumatic dilation 35.71%, P = 0.007), indicating that laparoscopic myotomy offered better clinical result than pneumatic dilation.[13] However, this meta-analysis had been challenged by a large and more recent randomized prospective trial, where Boeckxstaens et al. showed that after 2 years of follow-up, LHM, as compared with PD, was not associated with superior rates of therapeutic success.[3]
The 2-year success rate of 58% in our patients treated with “on demand” PD is in agreement with previous publications showing efficacy ranging from 35% to 93%.[8,14,15] Variation of success rates is possibly due to different use of PD protocol “serial vs. on demand,” methods of assessment “Eckardt score vs. others” and different periods of follow-up.
Previous studies have identified younger age (<40 years) and higher pressure at the lower esophageal sphincter after treatment has been reported as predictors of a negative outcome with PD.[3,6,15] We did not find any significant predictors of negative outcome, which is probably secondary to the size of our sample.
A small number of complications encountered with PD. Longitudinal transmural perforation of the esophageal body above the lower esophageal sphincter is the major complication of PD, occurring in approximately 0.5%-6% of cases.[7,16] In our study, only one perforation occurred, which was treated conservatively.
A potential shortcoming of this study results from its retrospective design, small sample size, and its limitation to patients seen at a single center. Strengths of the study include the uniform treatment and follow-up modality, strict methodology, and the long-term follow-up of both efficacy and the patient satisfaction rate.
CONCLUSION
PD is an efficacious procedure in Saudi achalasia patients with a very good overall patient satisfaction with 53.4 months of symptoms-free period after a successful dilatation.
ACKNOWLEDGMENT
This project is supported by College of Medicine Research Center, Deanship of Scientific Research, King Saud University.
Footnotes
Source of Support: The authors extend their sincere appreciation to the Deanship of Scientific Research at King Saud University for its funding of this research through the Research Group Project number RGP-VPP-279
Conflict of Interest: None declared.
REFERENCES
- 1.Boeckxstaens GE. Achalasia. Best Pract Res Clin Gastroenterol. 2007;21:595–608. doi: 10.1016/j.bpg.2007.03.004. [DOI] [PubMed] [Google Scholar]
- 2.Ferguson MK. Achalasia: Current evaluation and therapy. Ann Thorac Surg. 1991;52:336–42. doi: 10.1016/0003-4975(91)91373-4. [DOI] [PubMed] [Google Scholar]
- 3.Boeckxstaens GE, Annese V, des Varannes SB, Chaussade S, Costantini M, Cuttitta A, et al. Pneumatic dilation versus laparoscopic Heller's myotomy for idiopathic achalasia. N Engl J Med. 2011;364:1807–16. doi: 10.1056/NEJMoa1010502. [DOI] [PubMed] [Google Scholar]
- 4.Eckardt VF. Clinical presentations and complications of achalasia. Gastrointest Endosc Clin N Am. 2001;11:281–92. vi. [PubMed] [Google Scholar]
- 5.Richter JE. Modern management of achalasia. Curr Treat Options Gastroenterol. 2005;8:275–83. doi: 10.1007/s11938-005-0020-1. [DOI] [PubMed] [Google Scholar]
- 6.Hulselmans M, Vanuytsel T, Degreef T, Sifrim D, Coosemans W, Lerut T, et al. Long-term outcome of pneumatic dilation in the treatment of achalasia. Clin Gastroenterol Hepatol. 2010;8:30–5. doi: 10.1016/j.cgh.2009.09.020. [DOI] [PubMed] [Google Scholar]
- 7.Vantrappen G, Hellemans J. Treatment of achalasia and related motor disorders. Gastroenterology. 1980;79:144–54. [PubMed] [Google Scholar]
- 8.Karamanolis G, Sgouros S, Karatzias G, Papadopoulou E, Vasiliadis K, Stefanidis G, et al. Long-term outcome of pneumatic dilation in the treatment of achalasia. Am J Gastroenterol. 2005;100:270–4. doi: 10.1111/j.1572-0241.2005.40093.x. [DOI] [PubMed] [Google Scholar]
- 9.Allescher HD, Storr M, Seige M, Gonzales-Donoso R, Ott R, Born P, et al. Treatment of achalasia: Botulinum toxin injection vs. pneumatic balloon dilation. A prospective study with long-term follow-up. Endoscopy. 2001;33:1007–17. doi: 10.1055/s-2001-18935. [DOI] [PubMed] [Google Scholar]
- 10.Kadakia SC, Wong RK. Graded pneumatic dilation using Rigiflex achalasia dilators in patients with primary esophageal achalasia. Am J Gastroenterol. 1993;88:34–8. [PubMed] [Google Scholar]
- 11.Katz PO, Gilbert J, Castell DO. Pneumatic dilatation is effective long-term treatment for achalasia. Dig Dis Sci. 1998;43:1973–7. doi: 10.1023/a:1018886626144. [DOI] [PubMed] [Google Scholar]
- 12.West RL, Hirsch DP, Bartelsman JF, de Borst J, Ferwerda G, Tytgat GN, et al. Long term results of pneumatic dilation in achalasia followed for more than 5 years. Am J Gastroenterol. 2002;97:1346–51. doi: 10.1111/j.1572-0241.2002.05771.x. [DOI] [PubMed] [Google Scholar]
- 13.Wang L, Li YM, Li L. Meta-analysis of randomized and controlled treatment trials for achalasia. Dig Dis Sci. 2009;54:2303–11. doi: 10.1007/s10620-008-0637-8. [DOI] [PubMed] [Google Scholar]
- 14.Zerbib F, Thétiot V, Richy F, Benajah DA, Message L, Lamouliatte H. Repeated pneumatic dilations as long-term maintenance therapy for esophageal achalasia. Am J Gastroenterol. 2006;101:692–7. doi: 10.1111/j.1572-0241.2006.00385.x. [DOI] [PubMed] [Google Scholar]
- 15.Eckardt VF, Gockel I, Bernhard G. Pneumatic dilation for achalasia: Late results of a prospective follow up investigation. Gut. 2004;53:629–33. doi: 10.1136/gut.2003.029298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Katz P. Achalasia: Two effective treatment options--let the patient decide. Am J Gastroenterol. 1994;89:969–70. [PubMed] [Google Scholar]


