Abstract
This study reports secondary outcome analyses from a past study of the Penn Resiliency Program (PRP), a cognitive-behavioral depression prevention program for middle-school aged children. Middle school students (N = 697) were randomly assigned to PRP, PEP (an alternate intervention), or control conditions. Gillham et al., (2007) reported analyses examining PRP’s effects on average and clinical levels of depression symptoms. We examine PRP’s effects on parent-, teacher-, and self-reports of adolescents’ externalizing and broader internalizing (depression/anxiety, somatic complaints, and social withdrawal) symptoms over three years of follow-up. Relative to no intervention control, PRP reduced parent-reports of adolescents’ internalizing symptoms beginning at the first assessment after the intervention and persisting for most of the follow-up assessments. PRP also reduced parent-reported conduct problems relative to no-intervention. There was no evidence that the PRP program produced an effect on teacher- or self-report of adolescents’ symptoms. Overall, PRP did not reduce symptoms relative to the alternate intervention, although there is a suggestion of a delayed effect for conduct problems. These findings are discussed with attention to developmental trajectories and the importance of interventions that address common risk factors for diverse forms of negative outcomes.
Keywords: adolescence, prevention intervention, conduct problems, internalizing symptoms
Children and adolescents who show conduct problems often also experience internalizing symptoms such as depression and anxiety. Considering population-based samples, children and adolescents diagnosed with either of the two primary conduct diagnoses marked by high rates of externalizing symptoms (Conduct Disorder and Oppositional Defiant Disorder) are over 6 times more likely to have a comorbid depression diagnosis and over 3 times more likely to have a comorbid anxiety diagnosis (Angold & Costello, 2001). While the source and sequencing of this comorbidity continues to be an important and nuanced debate, overlapping risk factors certainly signal, and may contribute to, maladaptive developmental processes involved in co-occurring externalizing and internalizing symptoms (Caron & Rutter, 1991; Loeber & Keenan, 1994). For example, biased cognitive styles increase risk for conduct problems and anxiety or depression (see Dodge, 1993). Problems also transact over development: symptoms at one point in time increase the likelihood of academic and social failures. These failures, in turn, can contribute to a variety of later symptom, such as externalizing and internalizing problems (Burt, Obradovic, Long, & Masten, 2008; Cicchetti, Rogosch, & Toth, 1994). Thus, programs that effectively target shared risk factors may help reduce the more immediate development of anxiety, depression, or conduct problems, while also helping to address maladaptive processes that exacerbate or lead to additional problems later in development.
During the past 20 years several cognitive-behavioral depression prevention programs have been developed for children and adolescents (Horowitz & Garber, 2006). Many of these programs include skills training in perspective taking, decision making, coping and emotion regulation, and other techniques that are also used to treat conduct problems in children and adolescents (see McMahon, Wells, & Kotler, 2006). Similarly, many of these programs include techniques such as assertiveness, relaxation, and cognitive restructuring that are components of effective treatments for generalized and social anxiety. Despite the overlap in techniques, little is known about the effects of adolescent depression prevention programs on conduct problems and a broader range of internalizing symptoms including anxiety, somatic complaints, and social withdrawal.
The Penn Resiliency Program (PRP), a cognitive-behavioral depression prevention program for middle school age students, was designed to target depression and also, to some extent, broader internalizing and externalizing symptoms that often co-occur with depression during adolescence. PRP includes training in all of the skills just mentioned. The program was developed for delivery by school teachers and counselors. In previous studies, it has been implemented after school or during the school day (e.g., in health class or advisory). The program aims to help students develop skills that can serve as coping resources to avoid, cope with, or otherwise address stressors as they transition into adolescence and beyond. Sessions involve discussions, skill training, and role-plays in the classroom setting, and homework to reinforce the program content. In this way, PRP responds to calls to utilize the school setting as a context for promoting positive youth development and bolstering later competence and resilience (e.g., Masten, Herbers, Cutuli, & Lafavor, 2008).
Several studies demonstrate PRP’s benefits on depressive symptoms. A meta-analytic review of PRP studies indicates that PRP produces small but reliable reductions in depressive symptoms (Brunwasser, Gillham, & Kim, 2009), but less is known about its effects on externalizing symptoms or internalizing symptoms other than depression (Gillham, Brunwasser, & Freres, 2007). The first published study of PRP found significant reductions (relative to a control group) in children’s conduct problems as reported by parents immediately following the intervention and six months later (Jaycox et al., 1994). An evaluation of PRP in Australia found significant reductions in self-reported anxiety symptoms for PRP participants relative to controls (Roberts et al., 2003, 2004). A pilot study evaluating the combination of PRP and a parent program found significant prevention of anxiety symptoms through a one year follow-up period (Gillham et al., 2006). However, a recent randomized controlled study of PRP found no overall effect of PRP on anxiety symptoms, although PRP significantly reduced anxiety symptoms among adolescents with average and higher levels of hopelessness at baseline (Gillham et al., 2012). While some evidence suggests that PRP reduces anxiety and conduct problems, at least in the short term, a more comprehensive analysis is needed to evaluate the program’s effects on children’s symptoms and behavior in multiple contexts over a longer period of time.
This paper examines PRP’s effects on behavior problems and internalizing symptoms as reported by adolescents, their parents, and teachers in a large longitudinal evaluation (Gillham, Reivich, et al., 2007). Past analyses of PRP’s effects on self-reported depression (the primary study outcome) showed that PRP significantly reduced depressive symptoms relative to no-intervention control in two schools but was not more beneficial than control in the third. No benefit was found for PRP over an alternative intervention, the Penn Enhancement Program (PEP) that was designed to control for intervention ingredients that are not specific to cognitive-behavioral interventions, such as social support and the discussion of stressors. The current paper uses data from this evaluation to examine PRP’s effects on secondary outcomes including adolescents’ internalizing symptoms (anxiety/depression, somatic complaints, social withdrawal) and externalizing (conduct) symptoms as reported by adolescents, their parents, and teachers. We hypothesize that students in the PRP intervention will show lower levels of both internalizing and externalizing symptoms beginning with the post assessment and continuing through the three years of follow-up compared to the PEP intervention and compared to controls.
Method
Participants
Detailed information about study participants and methods is reported elsewhere (Gillham, Reivich et al., 2007). Participants were 697 6th, 7th, and 8th graders (376 boys, 321 girls) who participated in longitudinal evaluation of two school-based interventions designed to prevent symptoms of depression in adolescents. Of the 684 participants who provided information about race or ethnicity, 512 (75%) were Caucasian, 62 (9%) African American, 24 (4%) Asian, 13 (2%) Latino, and 73 (11%) some other race/ethnicity. Informed consent was obtained from parents and assent from adolescents before completing any study procedures. This work was approved by the Institutional Review Board of the University of Pennsylvania.
Intervention Conditions
At each of three participating schools, adolescents from consenting families were randomly assigned to one of the three study conditions. Adolescents assigned to the Penn Resiliency Program (PRP) participated in a cognitive-behavioral group intervention that met one day each week after school for 12 weeks. PRP covers a variety of cognitive skills including identifying common emotions, understanding the link between thoughts and feelings, challenging maladaptive thinking styles by examining evidence and alternatives, and decatrophizing. Behavioral skills include assertiveness, problem-solving, relaxation, and other skills for coping with difficult emotions and experiences. Adolescents assigned to the Penn Enhancement Program (PEP) participated in an alternative group intervention involving leader-facilitated discussions and interactive activities and games. PEP was also a depression prevention intervention involving some components that are shared with PRP, such as social support, attention from group leaders, and the discussion of day-to-day problems that are common in adolescence. However, PEP lacked the intervention components specific to cognitive-behavioral therapy, setting it apart from PRP in these ways. Therefore, PEP was primarily viewed as a control for non-cognitive-behavioral intervention ingredients found in PRP. PEP also met one day each week after school for 12 sessions. Adolescents assigned to the control condition did not participate in a PRP or PEP group. For more information on the PRP and PEP interventions, see Gillham and colleagues (2007).
PRP and PEP groups were led by school teachers, school counselors, and graduate students in school psychology, education, and clinical psychology (not affiliated with the research team). Prior to implementation, group leaders participated in a 30-hr training workshop. Leaders also completed biweekly group supervision with the PRP and PEP developers. There were 19 PRP groups and 19 PEP groups, each containing between 6 and 14 children. Research team members lead one PRP group and one PEP group to accommodate scheduling difficulties and a shortage of group leaders at the schools. No difference was found in effects for school staff (teachers and counselors) versus graduate students and researchers.
Assessments and Measures
Adolescents, their parents, and one of their current academic teachers completed questionnaires before the interventions began, again approximately two weeks after the intervention (post), and at six month intervals for three years following the intervention. Current analyses are based on parallel forms of the Achenbach System of Empirically Based Assessments (ASEBA: Achenbach, 1991). Adolescents in all conditions completed questionnaires including the Youth Self Report Form (YSR). Parents received the Child Behavior Checklist (CBCL) at these same intervals. Families chose which parent completed the CBCL. Researchers invited one of the adolescents’ current teachers to complete the Teacher Report Form (TRF) at each assessment point. All three measures (YSR, CBCL, and TRF) include two major composite scores reflecting internalizing symptoms (somatic complaints, social withdrawal, and symptoms of anxiety/depression) and externalizing symptoms (aggressive and delinquent behaviors). The ASEBA measures are among the most widely used in psychological research with children around the world.
Statistical Analyses
Intent-to-treat analyses examined intervention effects on internalizing and externalizing symptoms as reported by adolescents, their parents, and teachers. YSR, CBCL, and TRF externalizing and internalizing raw scores violated normality assumptions. Corrective square root transformations were used for YSR and CBCL data while a natural log transformation was applied to TRF scores. We report Mixed Model Analyses of Covariance (MM ANCOVAs) testing for main effects of condition. Likelihood ratio tests indicated the unstructured covariance structure was the most appropriate. This was supported by similar decisions based on other model fit statistics such as the AIC and BIC criterion. Statistical contrasts compared the estimated marginal means for each pair of conditions from the overall MM ANCOVA. When MM ANCOVAs revealed significant intervention effects, ANCOVAs examined intervention effects at each assessment point, with baseline scores covaried. We used two-tailed alphas and calculated effect sizes based on Cohen’s d using the difference in estimated marginal means divided by the pooled standard deviation. Negative effect sizes indicate that PRP symptom scores were lower than control (or PEP) scores over the follow-up period. For PEP vs. control comparisons, negative effect sizes indicate lower scores in PEP than Control.
Attrition and missing data
As with many longitudinal designs, the current study faced challenges with retention and attrition. Considering self-report assessments, 301 adolescents produced valid YSR scores at the final 3-year assessment, and approximately half (n = 377; 54%) produced valid YSR scores for at least 6 of the 8 assessment points. For the CBCL, parents produced valid scores for 160 participants at the final 3-year assessment, and about half (n = 355; 51%) provided scores at 3 or more assessments. Teachers provided valid TRF scores for 161 participants at the final 3-year assessment, and nearly half (332; 48%) provided valid TRF scores for at least 4 assessments. Rates of attrition did not differ between conditions, nor did attrition rates impact the effects of condition group presented below. Analyses controlling for the number of assessments that participants completed produced similar findings. The number of missing data points was not related to demographic variables nor baseline symptom scores, suggesting that patterns of missingness met the assumptions of data missing at random (Schafer & Graham, 2002).
Missing data were imputed using PROC MI of SAS version 9.1. The imputation procedure estimates missing values through an iterative process: First, maximum likelihood estimates were derived through an expectation-maximization (EM) algorithm. These estimates were then used as a starting point for a Markov chain Monte Carlo (MCMC) method to create five imputed datasets (Schafer & Graham, 2002). These datasets were collapsed into a single dataset for analyses by taking the mean of each value. Analyses were run using imputed and non-imputed datasets. The magnitudes of effect sizes were comparable. Results from the imputed dataset are reported here.
Results
Baseline Differences
Groups did not differ at baseline with respect to age, grade, income, or parents’ combined level of education. The groups differed on parent’s report of internalizing symptoms on the CBCL at baseline; the PRP and PEP participants both scored higher than controls, but did not differ from each other (see Table I). On the CBCL externalizing scale, the PEP group was marginally higher than controls (see Table II), but no other group differences emerged at baseline. The groups did not differ on the internalizing or externalizing scales of the YSR and TRF. All analyses covary baseline internalizing and externalizing symptom scores to control for these differences as well as the covariance between and within internalizing and externalizing symptoms across contexts at the baseline assessment. Correlations between key variables are presented in Table III.
Table I.
Parent’s report of internalizing symptoms: CBCL Internalizing Score means and test statistics.
| Mean (5D) |
ANCOVA F-Statistic d (95% CI lower bound; upper bound) |
|||||
|---|---|---|---|---|---|---|
| PRP | PEP | Control | PRP vs. Control | PEP vs. Control | PRP VS. PEP | |
|
|
|
|||||
| Baseline | 10.34 (7.20) |
10.15 (7.96) |
8.38 (6.58) |
F (1, 464) = 8.93** d = 0.27 (0.09; 0.45) |
F (1, 463) = 7.08** d = 0.25 (0.06; 0.43) |
F (1, 461) = .10 d = 0.03 (−0.15; 0.21) |
| Post | 7.92 (6.70) |
7.93 (6.84) |
7.86 (6.31) |
F (1, 458)= 10.57** d = −0.19 (−0.30; −0.08) |
F (1, 457) = 9.87** d = −0.13 (−0.29; −0.07) |
F (1, 455) = .04 d = −0.01 (−0.12; 0.10) |
| 6 months | 7.67 (5.63) |
7.13 (5.99) |
7.42 (6.12) |
F (1, 458) = 2.12 d = 0.09 (−0.22; 0.04) |
F (1, 457) = 9.41** d =−0.20 (−0.32; −0.07) |
F (1, 455) = 2.78† d = 0.10 (−0.02; 0.23) |
| 12 months | 6.17 (5.30) |
6.40 (5.74) |
6.59 (5.76) |
F (1, 458) = 13.37*** d = −0.23 (−0.36; −0.10) |
F (1, 457) = 9.26** d = −0.20 (−0.32; −0.07) |
F (1, 455) = .26 d = −0.03 (−0.16; 0.09) |
| 18 months | 6.16 (5.14) |
6.55 (5.71) |
7.56 (5.68) |
F (1, 458) = 48.63*** d = −0.44 (−0.56; −0.32) |
F 11,457)= 39.24*** d = −0.37 (−0.49; −0.25) |
F (1, 455) = 1.41 d = −0.07 (−0.19; 0.05) |
| 24 months | 4.94 (4.79) |
5.46 (5.00) |
6.29 (5.17) |
F (1, 458) = 35.92*** d = −0.43 (−0.56; −0.29) |
F (1, 457)= 17.51*** d = −0.30 (−0.43; −0.16) |
F (1, 455) = 3.68† d = −0.13 (−0.27; 0.01) |
| 30 months | 5.53 (4.81) |
6.06 (5.75) |
7.03 (5.75) |
F (1, 458) = 31.11*** d = −0.41 (−0.55; −0.27) |
F (1, 457) = 21.24*** d =−0.34 (−0.47;−0.19) |
F (1, 455) = 1.27 d = −0.08 (−0.22; 0.06) |
| 36 months | 5.01 (4.69) |
5.45 (5.08) |
6.00 (5.04) |
F (1, 458) = 20.48*** d = −0.35 (−0.50; −0.21) |
F (1, 457)= 14.14*** d = −0.27 (−0.41; −0.13) |
F (1, 455) = 1.31 d = −0.08 (−0.23; 0.06) |
p < .1;
p < .05;
p < .01;
p < 001
Table II.
Parent’s report of externalizing symptoms: CBCL Externalizing Score means and test statistics.
| Mean (5D) |
ANCOVA F-Statistic d (95% CI lower bound; upper bound) |
|||||
|---|---|---|---|---|---|---|
| PRP | PEP | Control | PRP vs. Control | PEP vs. Control | PRP vs. PEP | |
|
|
|
|||||
| Baseline | 11.35 (8.64) |
11.95 (9.20) |
10.40 (8.27) |
F (1, 464) = 1.872 d = .13 (−.056; .31) |
F (1, 463) = 3.51† d = .18 (−.01; .36) |
F (1, 461) = .30 d = −.05 (−.23; .13) |
| Post | 10.33 (8.82) |
10.65 (8.79) |
10.33 (9.14) |
F (1, 458) = .86 d = −.05 (−.16; .05) |
F (1, 457) = 1.94 d = −.08 (−.18; .03) |
F (1, 455) = .26 d = .03 (−.08; .13) |
| 6 months | 9.26 (7.18) |
9.67 (7.43) |
9.88 (8.59) |
F (1, 458) = 5.11* d = −.12 (−.23; −.02) |
F (1, 457)= 5.59* d = −.12 (−.23; −.02) |
F (1, 455) = .01 d = .00 (−.10; .11) |
| 12 months | 8.73 (7.88) |
9.09 (8.32) |
9.07 (8.50) |
F (1, 458) = 2.10 d = −.08 (−.19; .03) |
F (1, 457) = 3.19† d = −.10 (−.21; .01) |
F (1, 455) = .09 d = −.02 (−.09; .13) |
| 18 months | 7.65 (6.53) |
8.88 (7.45) |
10.11 (8.62) |
F (1, 453) = 33.04*** d = −.36 (−.48; −.24) |
F (1, 457) = 18.41*** d = −.25 (−.37; −.13) |
F (1, 455) = 3.67† d = −.11 (−.23; .01) |
| 24 months | 6.59 (6.44) |
7.97 (7.17) |
9.31 (8.42) |
F (1, 458) = 44.31*** d = −.43 (−.56; −.31) |
F (1, 457) = 15.81*** d = −.25 (−.38; −.13) |
F (1, 455) = 9.41** d = −.18 (−.30; −.06) |
| 30 months | 6.96 (6.73) |
8.52 (7.72) |
9.91 (8.84) |
F (1, 458) = 50.89*** d = −.45 (−.58; −.33) |
F (1, 457) = 18.61*** d = −.28 (−.40; −.16) |
F (1, 455) = 8.57** d = −.18 (−.30; −.05) |
| 36 months | 5.72 (6.01) |
6.89 (6.50) |
8.50 (7.65) |
F (1, 458) = 58.69*** d = −.51 (−.64; −.39) |
F (1, 457) = 25.29*** d = −.33 (−.46; −.20) |
F (1, 455) = 8.96** d = −.18 (−.31; −.06) |
p < .1;
p < .05;
p < .01;
p %lt; .001
Table III.
Correlations among adolescent, parent, and teacher report measures at baseline
| 2. | 3. | 4. | 5. | 6. | |
|---|---|---|---|---|---|
| 1. YSR Internalizing |
.59*** | .26*** | .19*** | .14** | .04 |
| 2. YSR Externalizing |
-- | .18*** | .41*** | .09* | .33*** |
| 3. CBCL Internalizing |
-- | .61*** | .21*** | .12* | |
| 4. CBCL Externalizing |
-- | .13** | .39*** | ||
| 5. TRF Internalizing |
-- | .38*** | |||
| 6. TRF Externalizing |
-- |
p <.05;
p <.01;
p <.001
Adolescent Reported Outcomes: YSR
MM ANOVAs revealed no overall intervention effects on YSR internalizing (F (2, 688) = 2.30; ns) or externalizing scores (F (2, 688) = 0.71; ns).
Parent Reported Outcomes: CBCL
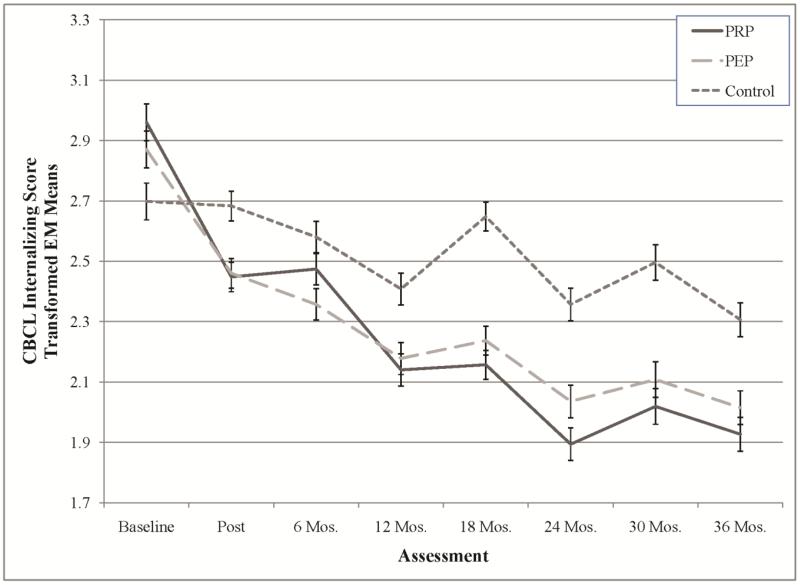
MM ANCOVA indicated an overall effect of condition on parent-reported internalizing symptoms (F (2, 688) = 21.66; p <.001). PRP and PEP reduced internalizing symptoms relative to no-intervention controls, but did not differ from each other: PRP v CON: t (688) = −6.03, d = −0.39, p <.01; PEP v CON: t (688) = −5.32, d = −0.34, p <.01, PRP v PEP, t (688) = −0.73, ns. ANCOVAs showed that PRP and PEP participants scored lower than controls on internalizing symptoms at all assessment points except 6 months post-intervention, but PRP and PEP groups did not significantly differ at any follow-up (see Table I and Figure 1).
Figure 1.
Square-root transformed CBCL internalizing score estimated marginal means by intervention condition. Error bars represent standard errors of the means. See Table 1 for corresponding test-statistics.
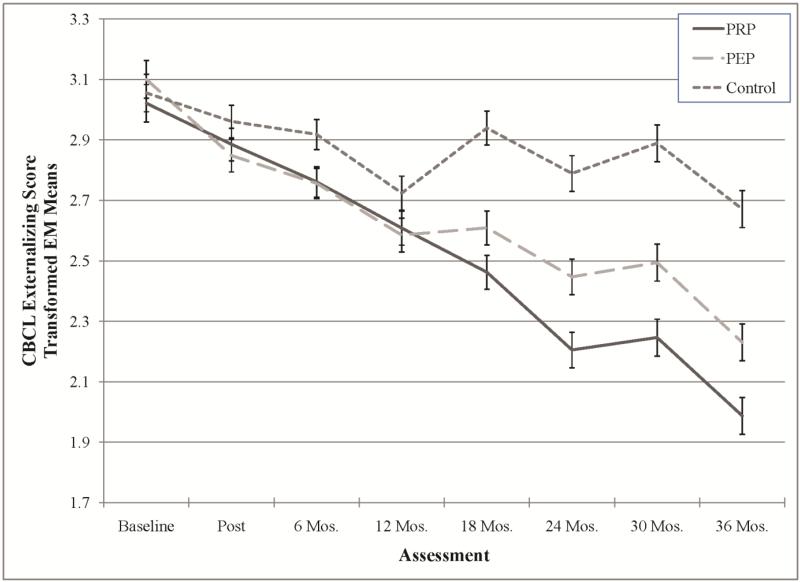
MM ANCOVA analyses also indicated an overall effect of intervention on parents’ report of externalizing symptoms (F (2, 688) = 10.33; p < .001). PRP and PEP reduced parents’ reports of externalizing symptoms relative to controls, but not relative to each other: PRP v CON: t (688) = −4.25, d = −0.28, p <.01; PEP v CON: t (688) = −3.54, d = −0.24, p <.01, PRP v PEP, t (688) = −0.04, d = −0.05, NS. ANCOVAs indicated that PRP reduced externalizing symptoms relative to PEP and to control groups at all assessment points beginning 2 years post-intervention through the end of follow-up (see Table II and Figure 2). [1]i
Figure 2.
Square-root transformed CBCL externalizing score estimated marginal means by intervention condition. Error bars represent standard errors of the means. See Table 2 for corresponding test-statistics.
Teacher Reported Outcomes: TRF
MM ANOVAs revealed no intervention effects on TRF internalizing (F (2, 688) = .00; NS) or externalizing scores (F (2, 688) = .69; NS).
Discussion
This study examined PRP’s effects on internalizing symptoms and externalizing symptoms as reported by adolescents, their parents, and their teachers. Contrary to our hypotheses, we did not find significant effects of PRP on self- or teacher-reports of adolescents’ internalizing and externalizing symptoms. However, we did find significant benefits of PRP on parents’ reports of both types of symptoms relative to controls.
These findings suggest that PRP produced benefits on adolescents’ symptoms and behavior that were observable to parents but not to teachers or to the behaviors the adolescents’ reported themselves. This inconsistency in findings by reporter is puzzling but consistent with a large body of research that documents limited agreement between self-, parent-, and teacher-reports of children’s and adolescents’ symptoms (De Los Reyes & Kazdin, 2005). This limited agreement was reflected in our sample as well; correlations between adolescent-, parent-, and teacher-reports of adolescents’ symptoms and behavior were statistically significant but small (see Table III). Adolescents, parents, and teachers observe behaviors in different contexts and likely have different comparison groups in mind when rating behavior. The PRP intervention may have had a more noticeable impact on behaviors at home than elsewhere. Furthermore, adolescents may view their own behavior differently across contexts, compared to parents or teachers reporting on behaviors at home or school, respectively. In any event, given the high attrition and the lack of significant results for adolescent and teacher reports, it will be important to replicate the parent report findings.
Parent reports suggest that changes in internalizing symptoms may precede changes in behavior problems. Effects on parents’ reports of adolescents’ internalizing symptoms (somatic complaints, social withdrawal, and depression/anxiety) appeared soon after the intervention (at the post assessment) and were significant for most assessments across the three years of follow-up. Effects on parents’ reports of adolescents’ conduct symptoms emerged about a year and a half after the intervention groups had ended.
We found limited evidence for PRP’s superiority relative to PEP. Considering overall effects, the PRP and PEP groups did not significantly differ with respect to either conduct or internalizing symptoms on any measure. While analyses examining symptom change across the entire follow-up revealed similar benefits for PRP and PEP, analyses examining individual assessment points revealed a small but significant reduction in conduct symptoms the PRP group relative to the PEP group beginning 2 years after the intervention. It may be that the PRP intervention continues to produce lower conduct symptoms past the third year, perhaps as the result of increased competence in adolescent transitions, but a longer period of follow-up would be needed to support this claim.
A delayed intervention effect during early and mid-adolescence is not unique to the current study (e.g., Hawkins, Guo, Hill, Battin-Pearson, & Abbott, 2001). Adolescence is a period of wide-reaching biological, psychological, and social transitions which may make it difficult to detect intervention effects (Masten, 2004). Furthermore, mid-adolescence is a period of increased risk for behavior problems, as evidenced by normative increases in poor conduct through mid-adolescence (Moffitt, 1993; Moffitt, 2006). It may be that the intervention effect for conduct problems is delayed until individuals enter mid-adolescence, a period of greater developmental risk for externalizing symptoms. It is also possible that PRP and PEP primarily benefit internalizing symptoms but, over time, reductions in these symptoms help to reduce externalizing symptoms perhaps because adolescents are more able to cope with difficult situations. Reductions in internalizing symptoms that are observable to others may also facilitate positive social interactions that protect against feelings of rejection and anger, and ultimately externalizing problems such as aggression. These interpretations call for future work on the meditational pathways and moderating factors that underlie the intervention effects.
Adolescence is a period of transition that carries increased risk for conduct, anxiety, and depression symptoms. Given the high rates of co-occurrence, empirically supported interventions that affect multiple types of symptoms are needed. Although studies of depression prevention programs in schools often do not examine effects on other types of psychopathology, some research suggests that depression prevention programs may also reduce anxiety, behavioral problems, and substance abuse (e.g., Hannan, Rapee, & Hudson, 2000; Lowry-Webster, Barrett & Lock, 2003; Stice, Rohde, Seeley, & Gau, 2008; Young et al., 2012). Given the high level of co-morbidity between depression and other difficulties (and the overlap between risk and protective factors), the assessment of a broad range of potential intervention effects is an important direction for future research.
The PRP intervention appears to reduce both parent-reported conduct and internalizing symptoms in adolescents relative to controls. However, PRP did not significantly reduce self- or teacher-reports of adolescents’ symptoms. As demonstrated by the current findings, it is important to include longitudinal follow-up and reports from multiple informants, as effects may differ over time and in different contexts. Future research should consider the processes through which interventions like PRP and PEP produce their effects, especially considering the limited evidence that the cognitive behavioral components of PRP had any effect beyond that of the non-cognitive behavioral PEP intervention. Attention to process will increase understanding of both positive and maladaptive developmental trajectories while suggesting even more effective ways of internalizing and externalizing problems across adolescence and into adulthood.
Acknowledgments
This project was supported by National Institute of Mental Health grant MH52270. We thank the adolescents, parents, school counselors, teachers, and other group leaders who participated in this project. The Penn Resiliency Program materials are available for use in research. Materials can be requested by e-mail to info@pennproject.org.
Footnotes
Past analyses found that the PRP intervention prevented depression symptoms in only two out of three participating sites (schools A and B versus C; Gillham et al., 2007). MM ANCOVAs that contain a School (A and B vs. C) × condition interaction term reveal that this is not the case with the reported CBCL internalizing symptom results (interaction term: F (2, 685) = 1.19, ns). However, similar to past depression findings, the PRP intervention was only effective in reducing CBCL externalizing symptom scores in schools A and B compared to school C (interaction term: F (2, 685) = 3.51, p < .05; Schools A and B: F (2, 425) = 12.49, PRP < PEP < Control; School C: F (2, 254) = 3.65, p < .05, PEP < Control, all other comparisons were not significant).
Disclosures: Drs. Gillham and Reivich are authors of the Penn Resiliency Program. The University of Pennsylvania has licensed the Penn Resiliency Program to Adaptiv Learning Systems. Drs. Reivich and Seligman own Adaptiv stock and could profit from the sale of this program. None of the other authors of this study has a financial relationship with Adaptiv.
Contributor Information
J. J. Cutuli, Department of Psychology, Rutgers University.
Jane E. Gillham, Department of Psychology, Swarthmore College
Tara M. Chaplin, Department of Psychology, George Mason University
Karen J. Reivich, Positive Psychology Center, University of Pennsylvania
Martin E. P. Seligman, Department of Psychology and Positive Psychology Center, University of Pennsylvania
Robert J. Gallop, Department of Mathematics and Applied Statistics, West Chester University
Rachel M. Abenavoli, Department of Human Development and Family Studies, Pennsylvania State University
Derek R. Freres, Positive Psychology Center, University of Pennsylvania
References
- Achenbach TM. Integrative guide for the 1991 CBCL/4-18, YSR, and TRF profiles. University of Vermont, Department of Psychiatry; Burlington, VT: 1991. [Google Scholar]
- Angold A, Costello EJ. The epidemiology of disorders of conduct: Nosological issues and comorbidity. In: Hill J, Maughan B, editors. Conduct disorders in childhood and adolescence. Cambridge University Press; Cambridge, UK: 2001. pp. 126–168. [Google Scholar]
- Brunwasser SM, Gillham JE, Kim E. A meta-analytic review of the Penn Resiliency Program’s effects on depressive symptoms. Journal of Consulting and Clinical Psychology. 2009;77:1042–1054. doi: 10.1037/a0017671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burt KB, Obradovic J, Long JD, Masten AS. The interplay of social competence and psychopathology over 20 years: Testing transactional and cascade models. Child Development. 2008;79:359–374. doi: 10.1111/j.1467-8624.2007.01130.x. [DOI] [PubMed] [Google Scholar]
- Caron C, Rutter M. Comorbidity in child psychopathology: Concepts, issues, and research strategies. Journal of Child Psychology and Psychiatry. 1991;32:1063–1080. doi: 10.1111/j.1469-7610.1991.tb00350.x. [DOI] [PubMed] [Google Scholar]
- Cicchetti D, Rogosch FA, Toth SL. A developmental psychopathology perspective on depression in children and adolescents. In: Reynolds WM, Johnston HF, editors. Handbook of depression in children and adolescents. Plenum Press; New York: 1994. pp. 123–142. [Google Scholar]
- De Los Reyes A, Kazdin AE. Informant discrepancies in the assessment of childhood psychopathology: A critical review, theoretical framework, and recommendations for further study. Psychological Bulletin. 2005;131:483–509. doi: 10.1037/0033-2909.131.4.483. [DOI] [PubMed] [Google Scholar]
- Dodge KA. Social-cognitive mechanisms in the development of conduct disorder and depression. Annual Review of Psychology. 1993;44:559–584. doi: 10.1146/annurev.ps.44.020193.003015. [DOI] [PubMed] [Google Scholar]
- Gillham JE, Brunwasser SM, Freres DR. Preventing depression early in adolescence: The Penn Resiliency Program. In: Abela JRZ, Hankin BL, editors. Handbook of Depression in children and adolescents. Guilford Press; New York: 2007. pp. 309–332. [Google Scholar]
- Gillham JE, Reivich KJ, Brunwasser SM, Freres DR, Chajon ND, Kash-MacDonald VM, Chaplin TM, Abenavoli RM, Matlin SL, Gallop RJ, Seligman MEP. Evaluation of a group cognitive-behavioral depression prevention program for young adolescents: A randomized effectiveness trial. Journal of Child and Adolescent Clinical Psychology. 2012;41:621–630. doi: 10.1080/15374416.2012.706517. doi: 10.1080/15374416.2012.706517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gillham JE, Reivich KJ, Freres DR, Chaplin TM, Shatté AJ, Samuels B, Elkon AGL, Litzinger S, Lascher M, Gallop R, Seligman MEP. School-based prevention of depressive symptoms: A randomized controlled study of the effectiveness and specificity of the Penn Resiliency Program. Journal of Consulting and Clinical Psychology. 2007;75:9–19. doi: 10.1037/0022-006X.75.1.9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gillham JE, Reivich KJ, Freres DR, Lascher M, Litzinger S, Shatté A, Seligman MEP. School-based prevention of depression and anxiety symptoms in early adolescence: A pilot of a parent intervention component. School Psychology Quarterly. 2006;21:323–348. [Google Scholar]
- Hannan AP, Rapee RM, Hudson JL. The prevention of depression in children: A pilot study. Behaviour Change. 2000;17:78–83. [Google Scholar]
- Hawkins JD, Guo J, Hill KG, Battin-Pearson S, Abbott RD. Long-term effects of the Seattle Social Development Intervention on school bonding trajectories. Applied Developmental Science. 2001;5:225–236. doi: 10.1207/S1532480XADS0504_04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horowitz JL, Garber J. The prevention of depressive symptoms in children and adolescents: A meta-analytic review. Journal of Consulting and Clinical Psychology. 2006;74:401–415. doi: 10.1037/0022-006X.74.3.401. [DOI] [PubMed] [Google Scholar]
- Jaycox LH, Reivich KJ, Gillham J, Seligman MEP. Preventing depressive symptoms in school children. Behaviour Research and Therapy. 1994;32:801–816. doi: 10.1016/0005-7967(94)90160-0. [DOI] [PubMed] [Google Scholar]
- Loeber R, Keenan K. Interaction between conduct disorder and its comorbid conditions: Effects of age and gender. Clinical Psychology Review. 1994;14:497–523. [Google Scholar]
- Lowry-Webster HM, Barrett PM, Lock S. A universal prevention trial of anxiety symptomology during childhood: Results at 1-year follow-up. Behaviour Change. 2003;20:25–43. [Google Scholar]
- Masten AS. Regulatory processes, risk, and resilience in adolescent development. Annals of the New York Academy of Sciences. 2004;1021:310–319. doi: 10.1196/annals.1308.036. [DOI] [PubMed] [Google Scholar]
- Masten AS, Herbers JE, Cutuli JJ, Lafavor TL. Promoting competence and resilience in the school context. Professional School Counseling. 2008;12(2):76–84. [Google Scholar]
- McMahon RJ, Wells KC, Kotler JS. Conduct problems. In: Mash EJ, Barkley RA, editors. Treatment of Childhood Disorders. 3rd ed Guilford; New York: 2006. pp. 137–270. [Google Scholar]
- Moffitt TE. Adolescence-limited and life-course-persistent antisocial behavior: A developmental taxonomy. Psychological Review. 1993;100(4):674–701. [PubMed] [Google Scholar]
- Moffitt TE. Life-course-persistent versus adolescence-limited behavior. In: Cicchetti D, Cohen DJ, editors. Developmental psychopathology, Volume 3: Risk, disorder, and adaptation. 2nd edition John Wiley and Sons; Hoboken, NJ: 2006. [Google Scholar]
- Roberts C, Kane R, Bishop B, Matthews H, Thompson H. The prevention of depressive symptoms in rural children: A follow-up study. International Journal of Mental Health Promotion. 2004;6:4–16. [Google Scholar]
- Roberts C, Kane R, Thomson H, Bishop B, Hart B. The prevention of depressive symptoms in rural school children: A randomized controlled trial. Journal of Consulting and Clinical Psychology. 2003;71:622–628. doi: 10.1037/0022-006x.71.3.622. [DOI] [PubMed] [Google Scholar]
- Schafer JL, Graham JW. Missing data: Our view of the state of the art. Psychological Methods. 2002;7:147–177. [PubMed] [Google Scholar]
- Stice E, Rohde P, Seeley JR, Gau JM. Brief cognitive-behavioral depression prevention program for high-risk adolescents outperforms two alternative interventions: A randomized efficacy trial. Journal of Consulting and Clinical Psychology. 2008;76:595–606. doi: 10.1037/a0012645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young JF, Makover HB, Cohen JR, Mufson L, Gallop RJ, Benas JS. Interpersonal psychotherapy-adolescent skills training: Anxiety outcomes and impact of comorbidity. Journal of Clinical Child & Adolescent Psychology. 2012;41:640–653. doi: 10.1080/15374416.2012.704843. [DOI] [PMC free article] [PubMed] [Google Scholar]