Abstract
Enterobius vermicularis is responsible for a variety of diseases but rarely affects the liver. Accurate characterisation of suspected liver metastases is essential to avoid unnecessary surgery. In the presented case, following a diagnosis of rectal cancer, a solitary liver nodule was diagnosed as a liver metastasis due to typical radiological features and subsequently resected. At pathological assessment, however, a necrotic nodule containing E vermicularis was identified. Solitary necrotic nodules of the liver are usually benign but misdiagnosed frequently as malignant due to radiological features. It is standard practice to diagnose colorectal liver metastases solely on radiological evidence. Without obtaining tissue prior to liver resection, misdiagnosis of solitary necrotic nodules of the liver will continue to occur.
Keywords: Liver, Misdiagnosis, Enterobius, Pinworms
Pinworm, Enterobius vermicularis, is considered the most common and least pathogenic of human helminthic infections.1 Residing primarily in the caecum, females migrate to the perineum nocturnally to lay eggs. Clinical associations are perineal discomfort and, less frequently, appendicitis or lower urinary tract symptoms in female patients.2,3 E vermicularis infections in the liver are extremely rare.4 The presented case involved liver resection for presumed colorectal liver metastasis (CRLM). Histological assessment, however, revealed an area of necrosis associated with E vermicularis infection.
Case history
A 44-year-old male with a 2-month history of rectal bleeding presented to his local hospital with abdominal pain and distension. He was a smoker, consumed moderate amounts of alcohol with a history of type 2 diabetes, hypertension and hypercholesterolaemia. Left-sided colonic obstruction was identified and at laparotomy a defunctioning colostomy was created proximal to a locally advanced rectal tumour (TNM stage T4NxMx). His staging computed tomography (CT) and magnetic resonance imaging (MRI) were reviewed at a dedicated hepatobiliary multidisciplinary meeting. A liver lesion consistent with a 2cm subcapsular CRLM was identified in segment 7 (Fig 1) with no further hepatic or extrahepatic disease.
Figure 1.
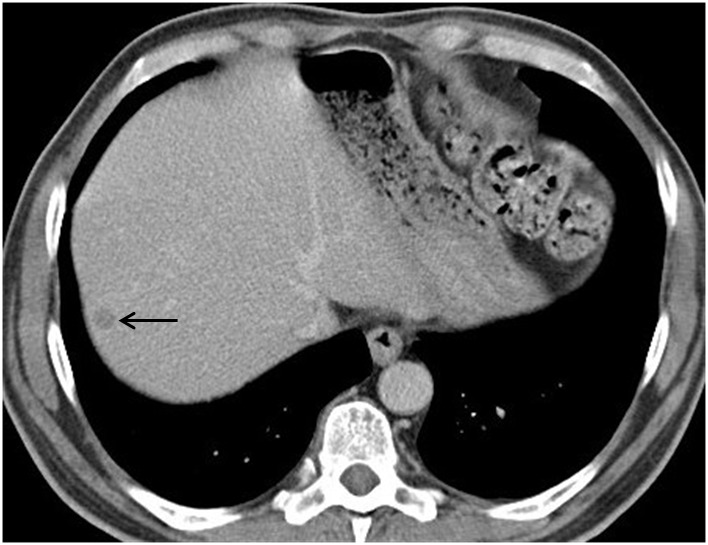
Contrast enhanced portal venous phase computed tomography demonstrating 2cm subcapsular lesion in segment 7 of the liver. The lesion displays typical low attenuation of a soft tissue mass characteristic of a colorectal liver metastasis.
Following completion of neoadjuvant chemoradiotherapy to downstage the pelvic disease, the patient underwent an uncomplicated non-anatomical liver resection. At this operation the liver was found to be macroscopically normal with the exception of the presumed CRLM. Intra-operative ultrasonography confirmed the presence of a hypoechoic lesion in keeping with appearances of a CRLM.
At pathological assessment, necrotic material was found in a fibrous capsule (Fig 2). The capsule was densely infiltrated by inflammatory cells, a high proportion of which were eosinophils. In the necrotic material multiple ova were observed, some of which were in a single worm (Fig 3). The ova are typical of E vermicularis, having both concave and convex surfaces. The specimen was excised completely with margins of normal liver. Prior to liver resection, the patient’s white cell and eosinophil count were normal (4.3 × 109/1 and 0.2 × 109/1; reference ranges: 3.5–9 × 109/1 and 0–0.5 × 109/1 respectively). There was no personal or family history of appendicectomy or perineal discomfort.
Figure 2.
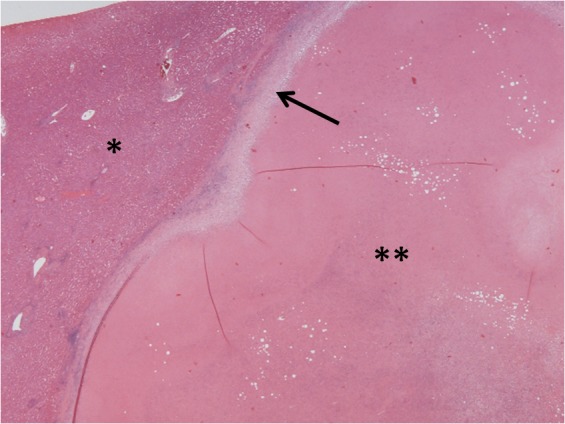
Haematoxylin and eosin stained section of normal liver (*) adjacent to the necrotic nodule (**) surrounded by a fibrous capsule (arrow)
Figure 3.
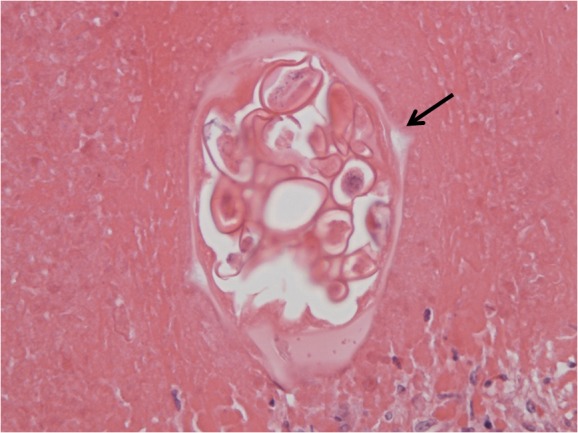
Haematoxylin and eosin stained cross-section of a female worm with its lateral alae (spine) marked by the arrow. Within the worm are several ova (one side concave, the other convex).
Discussion
Liver resection for CRLM is the standard of care when possible.5 A diagnosis is made on a background colorectal adenocarcinoma supported by findings from CT and MRI. Obtaining tissue from the hepatic metastasis to confirm the diagnosis is not performed routinely due to risks of needle track seeding and the high sensitivity and specificity of radiological findings to identify CRLM correctly. Typical features of CRLM on CT during the portal venous phase are of hypodense lesions. On MRI, appearances can be variable but the lesions typically exhibit a moderately high signal on T2 weighted images. On T1 sequences following gadolinium, they are of lower signal than the background parenchyma on the portal venous phase and often have rim enhancement in the arterial phase. In the present case, these features were observed, thus appearing very much like a CRLM.
E vermicularis infection can result in a variety of diseases that typically affect the gastrointestinal tract and perineum. In female patients this can be manifested as lower urinary tract symptoms and in children/adolescents as perineal discomfort.2 E vermicularis is an accepted cause of appendiceal pain where infection can obstruct the lumen of the appendix, creating appendiceal colic.3 Rarely, E vermicularis is found outside of the gastrointestinal tract in the peritoneum, fallopian tubes and liver.4,6,7 It is suggested that a breach in intestinal continuity permits translocation of the parasite out of the intestine.
The patient in the presented case had no history of an appendicectomy or perineal discomfort. The rectal tumour was locally advanced (T4) and presumably provided a route of access out of the patient’s intestine, possibly spreading to the liver via the peritoneal cavity. The subcapsular location of the nodule supports this hypothesis. Previously published cases of E vermicularis liver infection are very limited but tend to be misdiagnosed as hepatic metastases in patients with established malignancy.8 Two of these cases followed a diagnosis of colorectal tumour,9,10 suggesting an association. However, it is possible that routine staging/surveillance cross-sectional imaging will identify these asymptomatic lesions and it may be that they are truly incidental as one case followed a diagnosis of cutaneous melanoma.4
The lesion described in this report demonstrates features consistent with the solitary necrotic nodule of the liver (SNNL). SNNL typically consist of central necrosis surrounded by fibrosis. These are uncommon lesions that are usually benign and often misdiagnosed as metastases.11,12 In a review of 51 cases of SNNL, features on CT mimic those of CRLM with lesions being hypodense and demonstrating peripheral enhancement with arterial or portal phases in nearly 40% of cases.13
Conclusions
E vermicularis infection of the liver is exceptionally uncommon but has been reported previously following a history of colorectal carcinoma. It is unclear whether these asymptomatic liver lesions are being detected by coincidental cross-sectional imaging or whether there is a causal mechanism whereby the parasite may migrate from the intestine at the site of the tumour. The radiological features of E vermicularis infection in the liver mimic those of CRLM and of SNNL. For this reason, unless the fidelity or techniques of routine cross-sectional imaging change, benign liver lesions will continue to masquerade as metastases resulting in inappropriate intervention.
Acknowledgement
The authors would like to acknowledge and thank Professor Sebastian Lucas (Professor of Clinical Histopathology, King’s College London, UK) for his review and advice regarding E vermicularis infection of the liver in this case.
References
- 1.Surmont I, Liu LX.Enteritis, eosinophilia, and Enterobius vermicularis. Lancet 1995; 346: 1,167. [DOI] [PubMed] [Google Scholar]
- 2.MacPherson DW.Intestinal parasites in returned travelers. Med Clin North Am 1999; 83: 1,053–1,075 [PubMed] [Google Scholar]
- 3.Saxena AK, Springer A, Tsokas J, Willital GH.Laparoscopic appendectomy in children with Enterobius vermicularis. Surg Laparosc Endosc Percutan Tech 2001; 11: 284–286 [DOI] [PubMed] [Google Scholar]
- 4.Ng WS, Gallagher J, McCaughan G.‘Pinworm’ infection of the liver: unusual CT appearance leading to hepatic resection. Dig Dis Sci 2004; 49: 466–468 [DOI] [PubMed] [Google Scholar]
- 5.Tomlinson JS, Jarnagin WR, DeMatteo RPet al.Actual 10-year survival after resection of colorectal liver metastases defines cure. J Clin Oncol 2007; 25: 4,575–4,580 [DOI] [PubMed] [Google Scholar]
- 6.Gazvani MR, Emery SJ.Intraperitoneal Enterobius vermicularis infection: a case report. Infect Dis Obstet Gynecol 1996; 4: 28–30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Young C, Tataryn I, Kowalewska-Grochowska KT, Balachandra B. Enterobius vermicularis infection of the fallopian tube in an infertile female. Pathol Res Pract 2010; 206: 405–407 [DOI] [PubMed] [Google Scholar]
- 8.Lucas SB, Zaki SR, Portman BC.Other Viral and Infectious Diseases and HIV-related Liver Disease In: Burt A, Portmann B, Ferrell F, eds.MacSween's Pathology of the Liver. 6th edn.Edinburgh: Churchill Livingstone; 2011. pp435–444 [Google Scholar]
- 9.Daly JJ, Baker GF.Pinworm granuloma of the liver. Am J Trop Med Hyg 1984; 33: 62–64 [DOI] [PubMed] [Google Scholar]
- 10.Mondou EN, Gnepp DR.Hepatic granuloma resulting from Enterobius vermicularis. Am J Clin Pathol 1989; 91: 97–100 [DOI] [PubMed] [Google Scholar]
- 11.Deniz K, Coban G.Solitary necrotic nodule of the liver: always benign? J Gastrointest Surg 2010; 14: 536–540 [DOI] [PubMed] [Google Scholar]
- 12.Sundaresan M, Lyons B, Akosa AB. ‘Solitary’ necrotic nodules of the liver: an aetiology reaffirmed. Gut 1991; 32: 1,378–1,380 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zhou YM, Li B, Xu Fet al.Clinical features of solitary necrotic nodule of the liver. Hepatobiliary Pancreat Dis Int 2008; 7: 485–489 [PubMed] [Google Scholar]


