Abstract
Purpose
To characterize cognition in individuals with germline PTEN mutations (N=23) as well as in PTEN mutation-negative individuals with classic Cowden Syndrome or Bannayan-Riley-Ruvalcaba Syndrome (N=2).
Methods
Twenty-five individuals completed a comprehensive neuropsychological evaluation. One sample t-tests and effect sizes were used to examine differences in participant test scores compared with normal controls. Composite scores were created for each patient within each of the cognitive domains assessed and classified as above average, average, or below average according to normative standards. Chi-square analyses compared these classifications to expected proportions in normal control samples.
Results
The mean IQ was in the average range, and there was a wide range of intellectual functioning (extremely low to very superior). However, scores were lower than expected on measures of motor functioning, executive functioning, and memory recall suggesting a pattern of frontal lobe dysfunction in a large subset of participants.
Conclusion
This is the first study to characterize cognition in individuals with PTEN mutations and associated syndromes using a comprehensive neuropsychological battery. Contrary to previous association with intellectual disability, mean IQ was average, and there was a broad range of intellectual abilities. Specific evidence of frontal lobe dysfunction may have implications for treatment compliance and cancer surveillance and warrants further investigation.
Keywords: PTEN, PTEN Hamartoma Tumor Syndromes, Cowden Syndrome, Bannayan-Riley-Ruvalcaba Syndrome, Cognition, Neuropsychology
INTRODUCTION
PTEN (OMIM+601728), is a major tumor suppressor gene located on 10q23.3 with a documented role in heritable and sporadic malignancies. Germline PTEN mutations have been found to occur in a subset of several seemingly disparate clinical syndromes including Cowden syndrome (CS, OMIM 158350) and Bannayan-Riley-Ruvalcaba syndrome (BRRS, OMIM 153480) (reviewed in Zbuk and Eng, 20071). Irrespective of syndrome, individuals carrying germline PTEN mutations are umbrellaed under the term PTEN hamartoma tumor syndrome (PHTS) 1, 2. CS is an autosomal dominant disorder characterized by multiple hamartomas and a high risk of malignancies, with increased lifetime risks for female breast cancer (85%), epithelial thyroid cancer (35%), endometrial cancer (28%), renal cancer (34%), colorectal cancer (9%), and melanoma (6%)3. While the neoplastic risks have recently been reasonably well characterized, the neurobehavioral phenotype remains unknown.
Despite the fact that developmental delay, intellectual disability, and CNS anomalies have been associated with PHTS and related syndromes in family studies and small case series4–12, no known studies have systematically investigated the cognitive characteristics of these patients. The goal of this exploratory study was to characterize cognition in individuals with known PTEN mutations as well as in individuals with classic CS and BRRS who do not have PTEN mutations.
MATERIALS AND METHODS
Participants
Participants were recruited from an ongoing prospective observational study of PHTS, Cowden and Cowden-like individuals. Eligible participants were informed about the current cognitive study and invited to participate if they met the following inclusion criteria: 1) had undergone PTEN mutation analysis and a pathogenic mutation was detected, either through Cleveland Clinic research or clinical laboratories (N=23), or 2) in the absence of a deleterious PTEN mutation, presented with strong phenotypic features consistent with a diagnosis of CS or BRRS as outlined for CS by the International Cowden Consortium13 and for BRRS by disease-specific expert consensus14 (N=2). All research participants were required to travel to Cleveland, Ohio for study participation.
A total of 25 research participants were prospectively enrolled in this Institutional Review Board approved study (IRB No. 07-289) between July 2007 and July 2012 and provided informed consent for participation. All participants (20 adults, 5 children) completed a neuropsychological assessment as part of their participation in this research study. Parental consent was obtained for the participation of children with assent from the child. Adults ranged in age from 23 to 60 years (M=43.95, SD=12.19) and had a mean education level of 16.25 (SD=2.36). The five children in the study were ages 5, 5, 14, 16, and 17. Given their young age, the cognitive battery administered to the 5 year-olds did not include assessment of all cognitive domains. Twenty-three participants had an identified PTEN mutation. Of the two mutation negative research participants, one had classic BRRS and one had classic CS. Given that most research participants in the study had PTEN mutations (92%), this series will hereinafter be referred to as PHTS. Demographic and health characteristics for the participants are summarized in Table 1 and detailed phenotypic features in Supplemental Table S1.
Table 1.
Participant Demographic and Health Data
| Range | Mean (SD) | |
|---|---|---|
| Age | ||
| Children (n=5) | 5 – 17 | 11.40 (5.94) |
| Adults (n=20) | 23 – 60 | 43.95 (12.19) |
| Education | ||
| Adults (n=20) | 12 – 21 | 16.25 (2.36) |
| FSIQ (n=24) | 65 – 135 | 103.21 (17.17) |
| Number | Percent | |
| Sex | ||
| Male | 7 | 28% |
| Female | 18 | 72% |
| PTEN Mutation Status | ||
| Positive | 23 | 92% |
| Negative | 2 | 8% |
| Phenotype | ||
| Cowden Syndrome | 1 | |
| BRRS | 1 | |
| Brain MRI Findingsa | ||
| Negative/Nonspecific Findings | 3 | 21% |
| Venous Anomoly/Angioma Only | 1 | 21% |
| +Cystic Lesion | 2 | |
| Lhermitte Duclos Diseaseb | 2 | 15% |
| Chiari I Malformation Only | 2 | 21% |
| +Cystic Lesionb | 1 | |
| Meningiomab | 2 | 15% |
| Perinatal Ischemia | 1 | 7% |
| Prior Brain Surgery/Resection | 4 | 16% |
| Cerebellar Tumor | 2 | |
| Arachnoid Cyst | 1 | |
| Meningioma | 1 | |
| Cancer History | 14 | 56% |
| Breast Only | 4 | |
| Thyroid Only | 1 | |
| Breast and Thyroid | 3 | |
| Breast and Other Cancer(s)c | 3 | |
| Thyroid and Other Cancer(s)d | 2 | |
| Other Cancer(s)e | 1 | |
| Cancer Treatmentsf | 14 | 100% |
| Surgery Only | 7 | |
| + Chemotherapy Only | 2 | |
| + Radiation Only | 2 | |
| + Chemotherapy and Radiation | 3 | |
FSIQ=Full Scale IQ;
Results of brain MRI were available for 14 participants – reported percentages are based on these subjects only;
Counts include subjects who underwent prior brain surgery/resection;
uterine, skin, colorectal, and/or salivary;
uterine and/or skin;
prostate, lung, and skin;
Results are reported only for those subjects who had previously been diagnosed with cancer – related percentages are based on these subjects only.
Four participants had a history of brain surgery. Two had resection of cerebellar tumors [one with confirmed Lhermitte-Duclos disease (LDD) and one with probable LDD], one had a brain stem meningioma with hydrocephalus treated with surgical resection and ventriculoperitoneal (VP) shunt, and one had an arachnoid cyst treated with surgery and VP shunt placement. Brain MRIs were completed on an additional 10 research participants as part of their clinical care and were available for review. Of those, the most common findings were venous anomaly/angioma, Chiari I malformation, or cystic lesion. See Tables 1 and S1 for more information.
Fourteen research participants had a history of cancer not involving the CNS for which they underwent surgery. In addition, two research participants completed chemotherapy, two participants underwent radiation, and three participants had both chemotherapy and radiation. Cancer types and treatments are outlined in Table 1.
Genetic Analyses
Germline DNA was extracted in the Genomic Medicine Institute’s Genomic Medicine Biorepository and analyzed in a research laboratory (CE) for PTEN DGGE or Lightscanner-based mutational scanning (99% sensitive in Eng lab hands). Samples with variations via mutation scanning were re-PCR’ed and Sanger sequenced in the Genomics Core Facility, Cleveland Clinic. Large deletions and rearrangements were detected by MLPA and confirmed by quantative PCR.
Measures
All study participants completed a neuropsychological assessment that included clinical and structured diagnostic interviews conducted by a board-certified neuropsychologist (RB, JC, or JH) as well as a comprehensive cognitive battery that included measures of intellectual functioning, attention/concentration, visuomotor processing speed, language, executive functioning, visuospatial skills, memory recall, memory recognition, academic skills, and motor functioning. See Supplemental Tables S2 and S3 for a list of cognitive measures included in the neuropsychological assessment. All measures were scored according to their published test manuals using age-corrected and, when appropriate, education-corrected norms. To allow for comparison across measures, all test scores were transformed to standard scores with a mean of 100 and a standard deviation of 15. Higher standard scores reflect better performance. A summary of the cognitive data is provided in Table S2.
Analyses
Composite scores were created for each patient within each of the cognitive domains assessed (e.g., language, executive functioning) by summing standard scores of the completed measures within the cognitive domain and dividing the sum by the total number of measures within that domain. See Supplemental Table S3 for a list of the individual cognitive measures included in each domain.
One sample t-tests examined differences between test scores from individuals with PHTS and normative data obtained from control samples in published test manuals (normative mean standard score = 100, standard deviation = 15) on domain composites as well as on the individual subtests within each domain. Then, each participant’s domain scores were categorized as Above Average, Average, or Below Average using a one standard deviation (i.e., ±15 points) cutoff from the mean (i.e., 100). Chi-square analyses with exact tests were then computed for each cognitive domain to determine whether the proportion of participants within each of the three test performance categories differed significantly from expected proportions in the normal population (i.e., 16% Above Average, 68% Average, and 16% Below Average). Identical sub-analyses were performed on the individual measures within each cognitive domain.
RESULTS
One sample t-tests revealed that mean scores among individuals with PHTS were significantly lower than control samples in the Motor [t(22)=−5.02, p<.001, d=-.94) and Executive Functioning [t(22)=−3.67, p=.001, d=-.70] domains with large and medium effect sizes, respectively. There was also a similar trend in the Memory Recall domain [t(24)=−1.80, p=.085, d=−38], albeit with a smaller effect size. No significant differences were observed between individuals with PHTS and normal controls on any of the other cognitive domain scores. See Table 2.
Table 2.
Mean (SD) scores of PHTS subjects on neuropsychological domains and magnitude (Cohen’s d) of difference from the normal population. PHTS subjects show large, significant differences for the motor and executive functioning domains.
| Domain | PHTS | PHTS vs. population controls | |
|---|---|---|---|
| M (SD) | t (p) | Cohen’s d | |
| Intelligence | 103.2 (17.2) | 0.92 (.370) | .20 |
| Attention/Working Memory | 102.6 (16.4) | 0.73 (.474) | .17 |
| Processing Speed | 98.8 (12.9) | −0.46 (.651) | −.09 |
| Language | 97.1 (15.3) | −0.95 (.351) | −.19 |
| Executive Functioning | 90.3 (12.7) | −3.67 (.001) | −.70 |
| Visuospatial | 97.9 (15.6) | −0.66 (.514) | −.14 |
| Memory Recall | 94.0 (16.7) | −1.800 (.085) | −.38 |
| Memory Recognition | 100.2 (14.7) | 0.08 (.935) | .01 |
| Academic Skills | 104.6 (14.4) | 1.53 (.140) | .31 |
| Motor | 87.2 (12.2) | −5.02 (<.001) | −.94 |
Note. Population controls M=100, SD=15
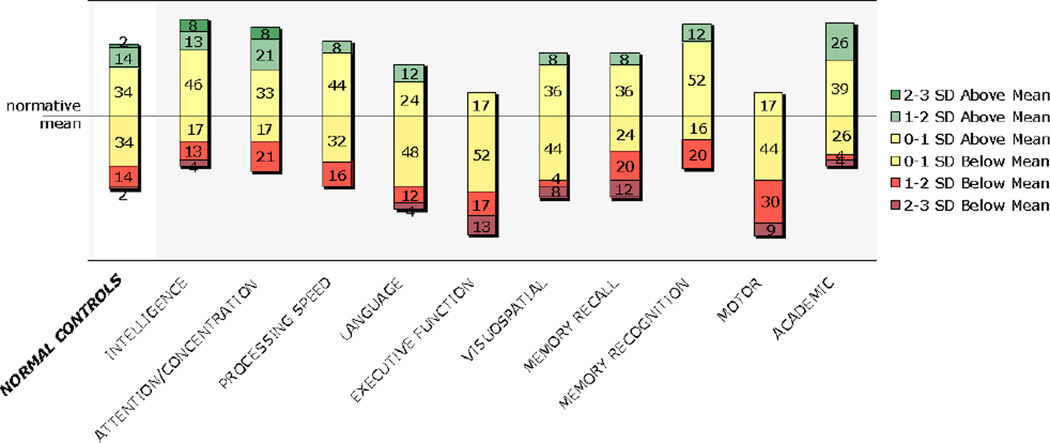
Chi-square analyses with exact tests revealed that more individuals with PHTS had reduced performance in the domain of Motor Functioning [χ2(2)=9.41, p=.009] compared to expected proportions in normal controls. There were also similar trends in Memory Recall [χ2(2)=5.24, p=.068] and Executive Functioning [χ2(2)=4.72, p=.097]. The proportion of PHTS individuals within each of the three performance groups did not significantly differ from that of normal controls on other cognitive domains assessed. See Figure 1.
Figure 1.
Cognitive performance of individuals with PHTS on composite domain scores compared to expected proportions in normal controls.
Numbers represent the percentage of patients falling within each score category. SD=standard deviation.
When individual tests within the Motor Functioning composite were examined, a larger proportion of individuals with PHTS had reduced fine manual dexterity compared to normal controls (Grooved Pegboard Test, p=.000). Of note, 7 participants demonstrated reduced performance with only one hand, while 10 participants demonstrated reduced manual dexterity bilaterally. Only 6 research participants in this sample had normal range manual dexterity scores bilaterally. Within the Executive Functioning composite, there was a greater than expected proportion of individuals with reduced performance on a measure of phonemic verbal fluency (Controlled Oral Word Association Test, p=.002) and a trend in this direction on a novel problem-solving task (Wisconsin Card Sorting Test, Perseverative Errors, p=.094). Finally, examination of measures within the Memory Recall composite revealed a larger percentage of individuals with reduced performance on the immediate recall trials of a word list learning task (Rey Auditory Verbal Learning Test, p=.009) and a trend in this direction on the delayed recall trial of this measure (p=.059). See Tables 2, S2, and S3 for a summary of results on all measures.
Examination of the overall cognitive profiles of each individual in this study revealed that three participants (12%) had rather global cognitive impairments across domains, including borderline to extremely low Full Scale Intelligence Quotients (FSIQ). Two of these research participants had a history of resected cerebellar tumor. FSIQ for the remaining participants (n=22) ranged from low average to very superior (standard score 80–135; M=107.38, SD=13.67). As noted above, the two youngest children in the study, both of whom were 5 years old, received relatively limited cognitive batteries given the test measures available for their age group. Therefore, cognitive profiles across all domains could not be examined for these two children. Of the adolescent and adult participants with low average or better FSIQ scores (n=20), the most commonly observed findings were reduced performance on measures of manual dexterity and/or executive functioning (EF). Specifically, 7 participants (35%) demonstrated reduced dexterity bilaterally, while 5 demonstrated reduced dexterity with only one hand (3 dominant, 2 nondominant). Most research participants demonstrated reduced performance on one (n=10) or two (n=3) EF measures. Of these, one patient underwent removal of an arachnoid cyst with placement of a VP shunt. Only one participant with low average or better FSIQ demonstrated low performance on all four measures of EF. This patient had a history of brain stem meningioma with hydrocephalus treated with VP shunt and surgical resection. Most individuals with low average or better IQ demonstrated intact performance on measures of academic ability, memory, naming, semantic fluency, visuospatial skills, and motor speed.
While four of the research participants in this study had brain surgeries/tumor resections that may have impacted their cognitive test performance, the overall pattern of results did not substantially change when data were re-analyzed following exclusion of these individuals. In fact, 72% of the remaining adolescent/adult participants had reduced manual dexterity with at least one hand, 89% had reduced performance on at least one measure of executive functioning, and 47% had reduced performance on at least one measure of memory recall. Further, there was not a higher incidence of reduced performance on these tasks in research participants with a history of cancer or those who had undergone prior cancer treatments (i.e., chemotherapy, radiation). Therefore, the cognitive findings in this study are not driven by effects of prior surgical or medical interventions. While there do not appear to be any obvious cognitive differences between individuals who are positive versus negative for a PTEN mutation, given the small sample size of mutation-negative participants (N=2) it was not possible to adequately examine cognitive differences as a function of PTEN mutation. Nevertheless, all analyses were re-run after excluding the two mutation-negative research participants, and the overall pattern of results remained unchanged.
DISCUSSION
This is the first study to examine cognitive functioning in individuals with PHTS and related syndromes using a comprehensive neuropsychological battery that assesses a wide range of cognitive domains. The existent literature has suggested an association between PHTS and developmental and/or intellectual disability4, 6, 10. However, most studies have based this conclusion on reported developmental history rather than formal assessment (i.e., intelligence testing) in individuals, family studies, or small case series comprised primarily of children. Clearly, the current study demonstrates a much wider range of intellectual capacity in individuals with PHTS than has previously been appreciated. In fact, there were only three individuals in the current study with FSIQ scores falling within the range seen in intellectual disability (i.e., borderline to extremely low scores), two of whom had undergone prior brain surgery. The remaining participants, who constituted 88% of the study sample, had FSIQ scores in the low average to very superior ranges. These findings are consistent with the observations of Miles and colleagues (1984) who reported that “true mental retardation was not a regular manifestation” (p. 231) in their sample of patients with BRRS10.
The pattern of findings in this study also suggests increased prevalence of frontal lobe dysfunction in individuals with PHTS. There were a larger proportion of individuals with PHTS with reduced performance on select measures of executive, motor, and memory functioning than would be expected in the normal population. Specifically, these research participants showed greater difficulty on measures of phonemic verbal fluency and fine manual dexterity than normal controls as well as perseverative responding on a measure of novel problem-solving. All of these measures have been associated with disruption of frontal lobe circuits15. Further, the memory difficulties observed in the study participants were restricted to free recall tasks rather than recognition memory measures. This memory pattern suggests a retrieval-based deficit rather than a primary encoding issue, providing further support for frontal lobe dysfunction16.
Results of available MRI studies suggest a high prevalence of brain anomalies (e.g., vascular malformations, cysts, tumors) in our study participants. In fact, there were imaging abnormalities reported in 79% of those research participants on whom MRI was available. This rate may not be representative of the entire sample given that MRI studies were conducted only in individuals where it was clinically indicated (i.e., 56% of this sample). Nevertheless, our findings are consistent with the few imaging studies reported in the literature7, 17. Lok and colleagues7 found cerebral abnormalities on brain MRI in 7 of 20 patients with Cowden syndrome who had no clinical indication of neurological dysfunction. Venous and cavernous angiomas were the most frequent abnormalities, followed by Lhermitte-Duclos disease, and one had a meningioma. While most of the observed neuroimaging abnormalities are generally considered to be “benign,” it is possible that they contributed to the cognitive findings.
While the overall pattern of test findings observed in this study is most consistent with frontal lobe dysfunction, we cannot rule out cerebellar dysfunction as a contributing factor given its role in many aspects of motor and cognitive functioning18–20. As noted, dysplastic gangliocytoma of the cerebellum (i.e., LDD) is often observed in individuals with PTEN mutations and, in adults, is considered pathognomonic for CS21–23. At least two research participants in the current study had confirmed/probable LDD; however, we cannot be sure of the actual prevalence of cerebellar abnormalities in this sample given that neuroimaging was not available for many research participants. Future studies that include neuroimaging will be required to make firm conclusions regarding the prevalence of brain anomalies, including LDD, in this population and their potential relationship to cognitive functioning.
Regardless of the underlying cause of the frontal lobe dysfunction observed, these cognitive difficulties may have important implications for treatment compliance and compliance with cancer surveillance in patients with PHTS. Executive functioning and memory retrieval difficulties may make it difficult for patients to organize and recall information provided to them by their physicians and to remain vigilant with treatment and surveillance recommendations. If future investigations provide corroborating evidence for a frontal lobe pattern of cognitive dysfunction, cognitive rehabilitation may be indicated, in at least a subset of individuals, to improve treatment compliance.
A limitation of the current study is that all participants were recruited as volunteers who were able to travel to Cleveland for research participation and willing to participate in completing an approximately 4 hour battery of cognitive testing. Thus, it is unknown the extent to which our sample is reflective of the larger PHTS population. Regardless, results suggest that intellectual disability is less common that previously reported. Further, there is no reason to suspect that volunteers would be more likely to display the observed pattern of frontal dysfunction than non-volunteers; in fact, we would hypothesize that this study captured a higher-functioning subset of adults given the organizational abilities needed to coordinate travel to Cleveland for participation. Future studies will be needed to replicate the current study findings, to examine the potential impact of cognitive dysfunction on treatment compliance, and to determine whether cognitive rehabilitation therapies used in other patient groups with frontal lobe dysfunction are effective in a PHTS population.
Supplementary Material
ACKNOWLEDGEMENTS
The authors wish to express their sincere thanks to the participants in this study for volunteering their time to be a part of this research. The authors also wish to thank Richard Naugle, Ph.D. and Imad Najm, M.D. at Cleveland Clinic for providing the resources necessary to complete this work
Dr. Eng is the Sondra J. and Stephen R. Hardis Endowed Chair of Cancer Genomic Medicine at the Cleveland Clinic and an ACS Clinical Research Professor.
Footnotes
CONFLICTS OF INTEREST
Drs. Frazier and Eng are PI and co-PI, respectively, of a sponsored research agreement from IntegraGen to study SNP markers in autism spectrum disorders. Dr. Busch, Dr. Chapin, Ms. Mester, Ms. Ferguson, and Dr. Haut declare no potential conflict of interest.
REFERENCES
- 1.Zbuk KM, Eng C. Cancer phenomics: RET and PTEN as illustrative models. Nat Rev Cancer. 2007;7:35–45. doi: 10.1038/nrc2037. [DOI] [PubMed] [Google Scholar]
- 2.Marsh DJ, Kum JB, Lunetta KL, et al. PTEN mutation spectrum and genotype-phenotype correlations in Bannayan-Riley-Ruvalcaba syndrome suggest a single entity with Cowden syndrome. Hum Mol Genet. 1999;8:1461–1472. doi: 10.1093/hmg/8.8.1461. [DOI] [PubMed] [Google Scholar]
- 3.Tan MH, Mester JL, Ngeow J, et al. Lifetime cancer risks in individuals with germline PTEN mutations. Clin Cancer Res. 2012;18:400–407. doi: 10.1158/1078-0432.CCR-11-2283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hanssen AMN, Werquin H, Suys E, Fryns JP. Cowden syndrome: report of a large family with macrocephaly and increased severity of signs in subsequent generations. Clin Genet. 1993;44:281–286. doi: 10.1111/j.1399-0004.1993.tb03901.x. [DOI] [PubMed] [Google Scholar]
- 5.Higgenbottom MC, Schultz P. The Bannayan syndrome: An autosomal dominant disorder consisting of macrocephaly, lipomas, hemangiomas, and risk for intracranial tumors. Pediatrics. 1982;69:632–634. [PubMed] [Google Scholar]
- 6.Cohen MM., Jr Mental deficiency, alterations in performance, and CNS abnormalities in overgrowth syndromes. Am J Med Genet C Semin Med Genet. 2003;117C:49–56. doi: 10.1002/ajmg.c.10013. [DOI] [PubMed] [Google Scholar]
- 7.Lok C, Viseux V, Avril MF, et al. Brain magnetic resonance imaging in subjects with Cowden syndrome. Medicine. 2005;84:129–136. doi: 10.1097/01.md.0000158792.24888.d2. [DOI] [PubMed] [Google Scholar]
- 8.Longy M, Lacombe D. Cowden disease. Report of a family and review. Ann Génét. 1996;39:35–42. [PubMed] [Google Scholar]
- 9.Lynch NE, Lynch SA, McMenamin J, Webb D. Bannayan-Riley-Ruvalcaba syndrome: a cause of extreme macrocephaly and neurodevelopmental delay. Arch Dis Child. 2009;94:553–554. doi: 10.1136/adc.2008.155663. [DOI] [PubMed] [Google Scholar]
- 10.Miles JH, Zonana J, Mcfarlane J, et al. Macrocephaly with hamartomas: Bannayan-Zonana Syndrome. Am J Med Genet. 1984;19:225–234. doi: 10.1002/ajmg.1320190204. [DOI] [PubMed] [Google Scholar]
- 11.Powell BR, Budden SS, Buist NRM. Dominantly inherited megalencephaly, muscle weakness, and myoliposis: A carnitine-deficient myopathy within the spectrum of the Ruvalcaba-Myhre-Smith syndrome. J Pediatr. 1993;123:70–75. doi: 10.1016/s0022-3476(05)81539-2. [DOI] [PubMed] [Google Scholar]
- 12.Starink TM, van der Veen JPW, Arwert F, et al. The cowden syndrome: a clinical and genetic study in 21 subjects. Clin Genet. 1986;29:222–233. doi: 10.1111/j.1399-0004.1986.tb00816.x. [DOI] [PubMed] [Google Scholar]
- 13.Pilarski R, Eng C. Will the real Cowden syndrome please stand up (again)? Expanding mutational and clinical spectra of the PTEN hamartoma tumour syndrome. J Med Genet. 2004;41:323–326. doi: 10.1136/jmg.2004.018036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gorlin RJ, Cohen MM, Jr, Condon LM, Burke BA. Bannayan-Riley-Ruvalcaba syndrome. Am J Med Genet. 1992;44:307–314. doi: 10.1002/ajmg.1320440309. [DOI] [PubMed] [Google Scholar]
- 15.Stuss DT, Alexander MP, Floden D, et al. Fractionation and localization of distinct frontal lobe processes: evidence from focal lesions in humans. In: Stuss DT, Knight RT, editors. Principles of frontal lobe function. New York, New York: Oxford University Press, Inc.; 2002. pp. 392–407. [Google Scholar]
- 16.Shimamura AP, Janowsky JS, Squire LR. What is the role of frontal lobe damage in memory disorders? In: Levin HS, Eisenberg HM, Benton AL, editors. Frontal lobe function and dysfunction. New York, New York: Oxford University Press, Inc.; 1991. pp. 173–195. [Google Scholar]
- 17.Tan W-H, Baris HN, Burrows PE, et al. The spectrum of vascular anomalies in subjects with PTEN mutations: implications for diagnosis and management. J Med Genet. 2007;44:594–602. doi: 10.1136/jmg.2007.048934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.O'Halloran CJ, Kinsella GJ, Storey E. The cerebellum and neuropsychological functioning: a critical review. J Clin Exp Neuropsychol. 2012;34:35–56. doi: 10.1080/13803395.2011.614599. [DOI] [PubMed] [Google Scholar]
- 19.Stoodley C. The cerebellum and cognition: evidence from functional imaging studies. Cerebellum. 2012;11:352–365. doi: 10.1007/s12311-011-0260-7. [DOI] [PubMed] [Google Scholar]
- 20.Bellebaum C, Daum I. Cerebellar involvement in executive control. Cerebellum. 2007;6:184–192. doi: 10.1080/14734220601169707. [DOI] [PubMed] [Google Scholar]
- 21.Robinson S, Cohen AR. Cowden disease and Lhermitte–Duclos disease: an update. Case report and review of the literature. Neurosurg Focus. 2006;20:1–6. doi: 10.3171/foc.2006.20.1.7. [DOI] [PubMed] [Google Scholar]
- 22.Vinchon M, Blond S, Lejeune JP, et al. Association of Lhermitte-Duclos and Cowden disease: report of a new case and review of the literature. J Neurol Neurosurg Psychiatry. 1994;57:699–704. doi: 10.1136/jnnp.57.6.699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Robinson S, Cohen A. Cowden disease and Lhermitte-Duclos disease: characterization of a new phakomatosis. Neurosurgery. 2000;46:371–383. doi: 10.1097/00006123-200002000-00021. [DOI] [PubMed] [Google Scholar]
- 24.Tan MH, Mester J, Peterson C, et al. A clinical scoring system for selection of subjects for PTEN mutation testing is proposed on the basis of a prospective study of 3042 probands. Am J Hum Genet. 2011;88:42–56. doi: 10.1016/j.ajhg.2010.11.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.