Abstract
Hematologic cancers comprise an aggregate of several different cancers, such as leukemia, lymphoma, and multiple myeloma. There are more than 100,000 new cases of these hematologic cancers in the United States annually, and more than 50,000 children and adults die from these cancers.1,2
Hematologic cancers affect the body’s blood, bone marrow, and lymphatic system, leaving these patients more susceptible to infections.1 A newly diagnosed patient with acute leukemia receives aggressive chemotherapy treatment and is closely monitored in the hospital for at least 3 to 4 weeks. Treatment-related signs and symptoms including fever, pain, nausea and vomiting, and respiratory distress may bring the patient to the emergency department before his or her next scheduled clinic appointment.3,4 In this article a case study of a patient with acute lymphoblastic leukemia who enters the emergency department will be used to illustrate a common clinical scenario and provide clinical implications for emergency nurses who care for patients with hematologic cancers.
Clinical Scenario
A 25-year-old Spanish-speaking Latino man presents in visible distress to the emergency department with fever, muscle aches, vomiting, coughing, shortness of breath, and a headache that resolved by the time he arrived in the emergency department. It has been 10 days since his discharge from induction (initial) chemotherapy for precursor B-cell acute lymphoblastic leukemia. His medical history includes type 2 diabetes and 2 finger amputations from a work-related injury. His current medications are Bactrim and insulin. His vital signs are as follows: temperature, 38.6°C (101.4°F); respirations, 22 breaths/min; heart rate, 104 beats/min; blood pressure, 98/64 mm Hg; and oxygen saturation, 93% on room air. Blood was drawn for laboratory testing from his implanted central venous access device. His white blood cell count was 1.1103/μL; absolute neutrophil count (ANC), 0.3 cells/μ; hemoglobin level, 7.1g/dL; hematocrit level, 23.1%; platelet count, 17,000×103/μL; and glucose level, 50mg/dL.
Management of Patient With Acute Leukemia
NEUTROPENIA
What is an ANC? An ANC provides the medical team an estimate of the person’s ability to fight off infections, particularly bacterial infections. A neutrophil is a type of white blood cell that kills bacteria. The Figure provides step-by-step instructions for calculating the ANC. An ANC at or below 500 indicates that a patient is at severe risk for infection. An ANC of 500 to 1000 denotes moderate infection risk, an ANC of 1000 to 1500 indicates minimal infection risk, and an ANC greater than 1500 is considered not clinically significant.5
FIGURE.
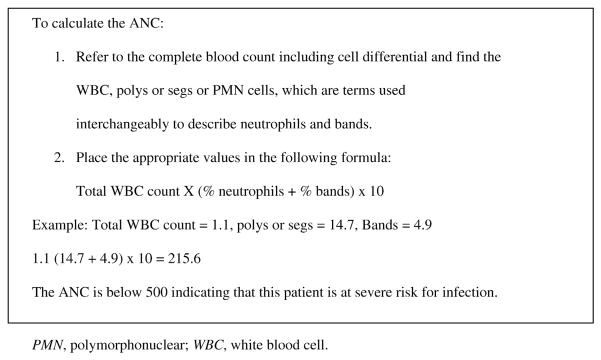
Step-by-step instructions for calculating ANC.
FEBRILE NEUTROPENIA
Febrile neutropenia (FN) is a relatively common but serious complication of treatment and post-treatment side effects for hematologic cancer patients.6 FN is defined as a single oral temperature of 38.3°C (101°F) or greater or a sustained temperature of 38.0°C (100.4°F) or greater over a 1-hour period in combination with neutropenia.7
BLOOD CULTURES
To optimize survival, the source of infection must be determined, and this is done by obtaining blood cultures. Blood cultures are obtained from the patient’s central venous access device (ie, Port-a-Cath [Smiths Medical MD, Inc, St. Paul, MN] or peripherally inserted central catheter) and a peripheral draw to determine the location of infection. In addition, urine, stool, mouth, skin, and sputum cultures may be obtained to rule out other sources of infection. A 2-view chest radiograph is typically ordered to rule out respiratory infections such as pneumonia.
INITIATION OF ANTIBIOTIC THERAPY
The American Society of Clinical Oncology (ASCO) revised its evidence-based practice guidelines for the management of FN in adults with cancer.8 ASCO still recommends that patients with neutropenia in whom a fever develops go immediately to the physician’s office, outpatient clinic, or hospital to receive initial antibacterial treatment.8,9 Evidence-based guidelines support that early, empirical broad-spectrum antibiotic therapy be initiated within 1 hour after a fever or blood cultures have been obtained to treat infection. Current practice guidelines recommend not delaying antibiotic therapy while waiting for blood culture results unless advised by the physician or health care provider. The patient’s drug allergies should be known before one selects and administers antibiotic therapy.
SUSPICION OF SEPSIS
The patient described earlier has 3 symptoms that make the clinician suspect sepsis, one of the gravest dangers to patients with hematologic cancers. In this case fever, mild hypotension, and tachycardia are observed as the 3 symptoms requiring medical attention. Early goal-directed therapy for patients with acute leukemia includes fluid resuscitation (to counter hypotension and tachycardia) and early administration of antimicrobial agents (to combat infection).10 These interventions have been proven to decrease the mortality rate and to be cost-effective in a wide variety of situations.11 Although a full complement of goal-directed therapy services may require more intensive care, these 2 crucial components can begin while the patient is in the emergency department.
Another important consideration for a patient receiving care for potential sepsis is blood glucose management. The patient in this case had a blood glucose level of 50 mg/dL, which was managed with 5% dextrose intravenously and oral intake of food and fluids. The follow-up blood glucose level was 142 mg/dL after these interventions. Current literature suggests that monitoring and management per current guidelines play important roles in sepsis care to optimize survival.12,13 Blood glucose levels in patients should be monitored per hospital-specific guidelines.
BLOOD TRANSFUSION SUPPORT
Patients with hematologic cancers will also likely need blood products throughout their treatment. Underproduction of blood and platelets in their marrow and chemotherapy toxicity are responsible for the inadequate recovery of their blood cells. Given this patient’s complete blood count values, he will need a transfusion of packed red blood cells. In this case the transfusion will also help with hypotension and tachycardia, as well as the patient’s shortness of breath. Although institutional policies vary, it is common to perform a transfusion in a patient whose hematocrit level is less than 25% or whose platelet count is less than 20,000.14 Again, institutional practice varies but premedication with 650 mg of acetaminophen and 25 mg of diphenhydramine orally is commonly used to prevent transfusion reactions. It is standard of care for a patient with a hematologic cancer to receive leukocyte-reduced and irradiated blood products to reduce transfusion reactions.
Educating Patient and Caregiver on Protective Precautions
The Oncology Nursing Society recommends the inclusion of the following protective precautions for neutropenic patients: hand hygiene; protective gowns for expected body fluid contamination; no visitors with symptoms of respiratory infection; private rooms with windows closed; negative-pressure rooms with anterooms for patients with airborne respiratory infections (eg, meningitis or pneumonia); high-efficiency particulate air filters; contact precautions with resistant organism colonization; and guidelines for the handling of ice, flowers, plants, and animals.15 Because the presented patient was accompanied by a close family member to the emergency department, it is important to communicate these precautions to both the patient and caregiver. Standardized patient education improves caregivers’ overall well-being and should become a routine part of patient care.16
Identification and Management of Cancer-Related Distress
The highest priority in care for patients with hematologic cancers in the emergency department is providing fluid resuscitation, antibiotics, and blood products as needed. However, once stabilization has begun, patients’ cancer-related distress (CRD) should be addressed to optimize their long-term outcomes. CRD is a complex psychological phenomena that has been found in as many as 35% to 50% of patients with hematologic cancers.17,18 Current theory suggests that demographics, intrinsic factors (personality), social support, disease progression, treatment, and communication with the health care team are all pre-existing factors that may contribute to CRD.19 Patients may be more vulnerable to CRD at various points in the treatment trajectory, which can include visits to the emergency department.
Although CRD is prevalent, it is often unrecognized in patients with cancer including hematologic cancer.20 High levels of CRD are associated with increased symptoms and lengths of hospitalization, as well as decreased health-related quality of life, and may necessitate modifications in chemotherapy treatment.21 FN, a severe side effect in patients receiving aggressive chemotherapy treatment, has been found to increase the symptom severity that patients experience and often delays chemotherapy treatment.22 Therefore patients in whom FN develops are at an additional risk of having CRD that may further complicate their care.
Recently, there has been a call for health care providers to recognize distress as the sixth vital sign, given the health and financial consequences associated with its presence.23 Thus nurses play a critical role in identifying and managing patients who are having CRD. The assessment of CRD may include using an instrument such as the National Comprehensive Cancer Network’s Distress Thermometer, which asks patients to rate their level of distress on a 0 to 10 numeric rating scale. Screening for distress should also include active listening and the assessment of both verbal and nonverbal cues.24
The management of CRD varies depending on the level of distress reported by the patient. Patients with moderate to high levels of CRD (defined as ≥4 of 10) should receive a referral to either a mental health, social work, pastoral care, or palliative care provider, depending on the source of distress.25 The Table provides further guidance on distress management and common symptoms based on varying levels of distress. Emergency nurses who assess CRD can help to manage this by using therapeutic communication skills that promote a trusting relationship23 and allow adequate time for the patient to ask questions and understand the plan of care.24 Nursing care is imperative in the identification and management of CRD and can lead to positive outcomes for patients and their families, which ultimately improves health-related quality of life and quality of care.
TABLE.
| Level of distress | Management | Common symptoms of distress that may be observed in emergency department |
|---|---|---|
| Low (0–3 of 10) |
|
General: anger, uncertainty, poor concentration Psychological: anxiety, depression, panic, worry |
| Moderate-high (4–10 of 10) |
|
Somatic: gastrointestinal upset, pain, dyspnea, palpitations, fatigue, weakness |
Conclusion
The described patient entered the emergency department because of physical and CRD changes and was admitted to the hospital. Per ASCO guidelines regarding management of FN, he was appropriately assessed, blood cultures were obtained, he received antibiotic treatment for FN and supportive care provided through fluid and blood transfusions, and cancer care education was provided to the patient and his caregiver. Emergency nurses will encounter such patients presenting with delayed and late side effects from treatment. The recognition of immunosuppression as a risk factor for sepsis is especially important. To optimize survival, these patients need to be admitted to the hospital for observation and antibiotic therapy while their blood cultures are pending, rather than being treated and discharged from the emergency department. By advocating for evidence-based care and identifying CRD, emergency nurses are critical in ensuring that patients with FN receive early medical intervention.
Acknowledgments
Supported by a National Cancer Institute Cancer Care Quality grant (R25CA116339) (A.L.B.), a Doctoral Scholarship in Cancer Nursing (renewal DSCNR-13-276-03) from the American Cancer Society (A.W.), and an Interdisciplinary Training of Nurse Scientists in Cancer Survivorship Research grant (T32NR011972) (T.A.A.).
Contributor Information
Ashley Leak Bryant, School of Nursing, The University of North Carolina at Chapel Hill, Chapel Hill, NC.
AnnMarie Walton, College of Nursing, University of Utah, Salt Lake City, UT; Social/Clinical Research Specialist, Lineberger Comprehensive Cancer Center and Adjunct Clinical Instructor, School of Nursing, The University of North Carolina at Chapel Hill, Chapel Hill, NC.
Tara A. Albrecht, Adult Health & Nursing Systems, School of Nursing, Virginia Commonwealth University, Richmond, VA.
References
- 1.Centers for Disease Control and Prevention. [Accessed February 17, 2013];Blood cancers: leukemia, lymphoma, and myeloma. http://www.cdc.gov/features/hematologiccancers/
- 2.Siegel R, Naishadham D, Jemal A. Cancer statistics, 2013. CA Cancer J Clin. 2013;62(1):11–3. doi: 10.3322/caac.21166. [DOI] [PubMed] [Google Scholar]
- 3.Mayer DK, Travers D, Wyss A, Leak A, Waller A. Why do cancer patients visit emergency departments? Results of a 2008 population study in North Carolina. J Clin Oncol. 2011;29(19):2683–8. doi: 10.1200/JCO.2010.34.2816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Leak A, Mayer D, Wyss A, Travers D, Waller A. Why do cancer patients die in the emergency department? An analysis of 283 deaths in NC EDs. Am J Hosp Palliat Care. 2013;30(2):178–82. doi: 10.1177/1049909112445306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Camp-Sorrell D. Myelosuppression. In: Itano J, Taoka K, editors. Core Curriculum for Oncology Nursing. 4. St. Louis, MO: Elsevier; 2005. p. 262. [Google Scholar]
- 6.Nirenberg A, Bush A, Davis A, Friese C, Gillespie T, Rice R. Neutropenia: state of the knowledge part 1. Oncol Nurs Forum. 2006;33(6):1193–201. doi: 10.1188/06.ONF.1193-1201. [DOI] [PubMed] [Google Scholar]
- 7.Freifeld A, Bow E, Sepkowitz K. Clinical practice guideline for the use of antimicrobial agents in neutropenic patients with cancer: 2010 update by the Infectious Diseases Society of America. Clin Infect Dis. 2011;52:e56–93. doi: 10.1093/cid/cir073. [DOI] [PubMed] [Google Scholar]
- 8.Eastman P. New guideline from ASCO on management of neutropenia and fever aims to reduce unnecessary hospitalizations. [Accessed May 30, 2013.];Oncology, Times. http://journals.lww.com/oncology-times/blog/onlinefirst/pages/post.aspx?PostID=650.
- 9.Flowers C, Seidenfeld J, Bow E. Antimicrobial prophylaxis and outpatient management of fever and neutropenia in adults treated for malignancy. American Society of Clinical Oncology clinical practice guideline. J Clin Oncol. 2013;31:794–810. doi: 10.1200/JCO.2012.45.8661. [DOI] [PubMed] [Google Scholar]
- 10.Shapiro NI, Wolfe RE, Moore RB, Smith E, Burdick E, Bates DW. Mortality in Emergency Department Sepsis (MEDS) score: a prospectively derived and validated clinical prediction rule. Crit Care Med. 2003;31(3):670–5. doi: 10.1097/01.CCM.0000054867.01688.D1. [DOI] [PubMed] [Google Scholar]
- 11.Huang DT, Angus DC, Dremsizov TT, Rivers EP, Clermont G. Cost-effectiveness of early goal-directed therapy in the treatment of severe sepsis and septic shock [abstract] Crit Care. 2003;7(Suppl 2):232. [Google Scholar]
- 12.Penack O, Buchheidt D, Christopeit M. Management of sepsis in neutropenic patients: guidelines from the Infectious Disease Working Party of the German Society of Hematology and Oncology. Ann Oncol. 2011;22:1019–29. doi: 10.1093/annonc/mdq442. [DOI] [PubMed] [Google Scholar]
- 13.Dellinger R, Levy M, Rhodes A. Surviving Sepsis Campaign: international guidelines for management of severe sepsis and septic shock: 2012. Crit Care Med. 2013;41:580–637. doi: 10.1097/CCM.0b013e31827e83af. [DOI] [PubMed] [Google Scholar]
- 14.Milligan DW, Grimwade D British Committee for Standards in Haematology. Guidelines on the management of acute myeloid leukaemia in adults. Br J Haematol. 2003;135:450–74. doi: 10.1111/j.1365-2141.2006.06314.x. [DOI] [PubMed] [Google Scholar]
- 15.Oncology Nursing Society. [Accessed February 20, 2013.];Quick view for prevention of infection. http://www.ons.org/ClinicalResources/media/ons/docs/research/outcomes/infection/quickview.pdf.
- 16.Creedle C, Leak A, Deal A. The impact of education on caregiver burden on two inpatient oncology units. J Cancer Educ. 2012;27(2):250–6. doi: 10.1007/s13187-011-0302-3. [DOI] [PubMed] [Google Scholar]
- 17.Albrecht T, Rosenzweig M. Management of cancer-related distress in patients with a hematologic malignancy. J Hosp Palliat Nurs. 2012;14(7):462–8. doi: 10.1097/NJH.0b013e318268d04e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Carlson LE, Angen M, Cullum J. High levels of untreated distress and fatigue in cancer patients. Br J Cancer. 2004;90(12):2297–304. doi: 10.1038/sj.bjc.6601887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Albrecht TA, Rosenzweig M. Distress in patients with acute leukemia: a concept analysis. Cancer Nurs. doi: 10.1097/NCC.0b013e31829193ad. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Albrecht T, Rosenzweig M. The symptom experience in patients hospitalized for the treatment of acute leukemia. Oncol Nurs Forum. 2012;39(6):E517. [Google Scholar]
- 21.Pirl WF, Muriel A, Hwang V. Screening for psychosocial distress: a national survey of oncologists. J Support Oncol. 2007;5(10):499–504. [PubMed] [Google Scholar]
- 22.Given CW, Jeon S, Sikorskii A. Effect of neutropenia on the impact of a cognitive-behavioral intervention for symptom management. Cancer. 2005;104(4):869–78. doi: 10.1002/cncr.21240. [DOI] [PubMed] [Google Scholar]
- 23.Bultz BD, Carlson LE. Emotional distress: the sixth vital sign—future directions in cancer care. Psychooncology. 2006;15(2):93–5. doi: 10.1002/pon.1022. [DOI] [PubMed] [Google Scholar]
- 24.Ryan H, Schofield P, Cockburn J. How to recognize and manage psychological distress in cancer patients. Eur J Cancer Care (Engl) 2005;14(1):7–15. doi: 10.1111/j.1365-2354.2005.00482.x. [DOI] [PubMed] [Google Scholar]
- 25.Holland J, Andersen B, Breitbart W. Vol. 3. National Comprehensive Cancer Network; [Accessed May 23, 2013.]. NCCN clinical practice guidelines in oncology: distress management. http://www.nccn.org/professionals/physician_gls/f_guidelines.asp#distress. [DOI] [PMC free article] [PubMed] [Google Scholar]


