Abstract
Objective
To describe the utilization of prenatal care in American Samoan women and to identify socio-demographic predictors of inadequate prenatal care utilization.
Methods
Using data from prenatal clinic records, women (n=692) were categorized according to the Adequacy of Prenatal Care Utilization Index as having received adequate plus, adequate, intermediate or inadequate prenatal care during their pregnancy. Categorical socio-demographic predictors of the timing of initiation of prenatal care (week of gestation) and the adequacy of received services were identified using one way Analysis of Variance (ANOVA) and independent samples t-tests.
Results
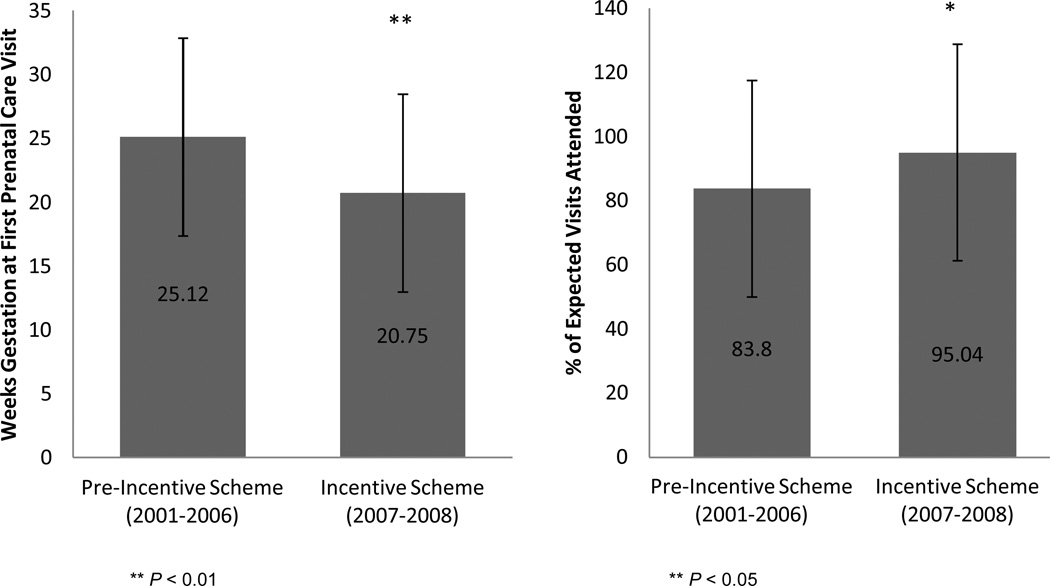
Between 2001 and 2008 85.4% of women received inadequate prenatal care. Parity (P=0.02), maternal unemployment (P=0.03), and both parents being unemployed (P=0.03) were negatively associated with the timing of prenatal care initation. Giving birth in 2007–2008, after a prenatal care incentive scheme had been introduced in the major hospital, was associated with earlier initiation of prenatal care (20.75 versus 25.12 weeks; P<0.01) and improved adequacy of received services (95.04% versus 83.8%; P=0.02).
Conclusion
The poor prenatal care utilization in American Samoa is a major concern. Improving healthcare accessibility will be key in encouraging women to attend prenatal care. The significant improvements in the adequacy of prenatal care seen in 2007–2008 suggest that the prenatal care incentive program implemented in 2006 may be a very positive step toward addressing issues of prenatal care utilization in this population.
Keywords: Pregnancy, Prenatal Care, Kotelchuck Index, American Samoa
Background
Ensuring that pregnant women have universal and timely access to quality prenatal care is a global public health priority as indicated by Millennium Development Goal #5 [1]. An optimal program of pre-delivery care usually consists of medical screening, physical and ultrasound exams, education and counseling and, if necessary, assistance with social services [2].
Despite a global focus on the universal provision of prenatal care there are well recognized disparities in prenatal care utilization and consequently in maternal and child health outcomes. Almost all maternal deaths (99%) occur in low and middle income countries (LMIC) [3]. While it is well documented that women in LMIC tend to access prenatal care late and attend an insufficient amount of appointments, the reasons for poor utilization vary widely and may be closely intertwined with local culture or local healthcare infrastructure. Socio-demographic risk factors for insufficient prenatal care that have been consistently identified in LMIC include young maternal age, low educational attainment, high birth order, being unmarried, and having insufficient income [4]. Accurate assessment of prenatal care utilization and the associated barriers to its access is the critical first step in the development of targeted public health programs to improve prenatal care access overall and in at risk groups [5].
American Samoa is an unincorporated island territory of the U.S. which lies ~2,400 miles Southwest of Hawaii and has a population of 54,947, predominantly made up of native Samoans who are recognized as US nationals [6]. Fifty-eight percent of families have incomes below the U.S. poverty level [7]. American Samoa faces very similar issues with provision of healthcare as other low-middle income island populations, particularly other Pacific island nations, who face unique issues of healthcare supply and demand, consistency of service provision and outward migration of healthcare professionals [8,9]. As such, American Samoa is considered both a medically underserved area and a healthcare professional shortage area [10].
Among pregnant Samoan women in New Zealand late initiation of prenatal care is common and is associated with high parity, low educational attainment, and pre-pregnancy unemployment [11]. The aim of this paper is to describe the utilization of prenatal care in American Samoa and to identify socio-demographic predictors of inadequate prenatal care utilization.
Methods
Quantitative Analysis Sample
Data for these analyses were extracted during a review of medical records in American Samoa in June 2008. The records of 1036 women who received prenatal care at the Tafuna Family Health Center (TFHC), Tafuna or the Lyndon B Johnson (LBJ) Tropical Medical Center, Pago Pago between 2001 and 2008 were available for review. The TFHC is a community health center which serves approximately 20,858 residents in Tualauata County [12]. The clinic provides prenatal services for low risk pregnancies until the last month of pregnancy. LBJ, the only full service hospital on the island, also provides prenatal care to low risk pregnancies, all high risk pregnancies, and all women in the last month of their pregnancy. Every women whose records were available for review delivered their infant at LBJ where approximately 97% of the ~1300 deliveries per year in American Samoa occur.
Of these women, 692 were Samoan (self-reported), had singleton births and complete data on their prenatal care, delivery, and infant outcomes. The postnatal growth of their infants is described elsewhere [13]. Clinic records were reviewed to determine the week of gestation at the woman’s first prenatal care visit, the total number of prenatal care visits they attended, and the length of their gestation in addition to various socio-demographic characteristics of the women and their partners. All data collection procedures were approved by the appropriate institutional review boards at Brown University and the American Samoa Department of Health.
Socio-demographic Characteristics
All of the socio-demographic characteristics of the mother and father available in the prenatal care records were utilized in this analysis. Women were classified as primiparous or having <4 or ≥4 children (based on the midpoint of the sample range (0–8)). Age, educational attainment and employment status of both the mother and the father were included in analysis. Employment status was divided into four categories: unemployed, managerial positions, manual labor and farming, reflecting standard categorizations of this population. Maternal marital status was dichotomized into single (single, separated, divorced or widowed) or married/cohabiting. A parental employment variable was created to describe whether one or both of the parents were employed.
Year of Delivery
Year of delivery was recorded and included in the analysis based on the fact that in 2006 a prenatal care incentive scheme was introduced at LBJ. Year of delivery was dichotomized as pre-introduction of the scheme (deliveries in 2006 or earlier) and post-introduction of the scheme (2007 onward).
Adequacy of Prenatal Care Utilization Index
The Adequacy of Prenatal Care Utilization (APNCU) Index [4] was used to describe prenatal care. The index reports on two dimensions: the timing of initiation (Adequacy of Initiation) and the number of visits a woman actually attends in relation to the amount she is expected to attend based on the American College of Obstetricans and Gynecologists (ACOG) guidelines [14] (Adequacy of Received Services). Within each dimension women were placed into one of four groups based on the adequacy of prenatal care received: adequate plus, adequate, intermediate and inadequate. An index summary variable was also calculated which combined the two dimensions into a single measure of prenatal care adequacy [4].
Statistical Analysis
Adequacy of received services was compared across initiation categories using a Chi-squared test. Because of a lack of variation in the timing of initiation of prenatal care in the study sample, timing of initiation was treated as a continuous variable (reported in weeks) to identify associated socio-demographic predictors. One way Analysis of Variance (ANOVA) (with Bonferroni correction for multiple comparisons) and independent samples t-tests were used to examine associations with categorical predictors. Predictors of the adequacy of received services, expressed as a percentage of expected visits actually attended, were examined in the same way.
Qualitative Data
In 2010, in a separate study, in depth personal interviews were undertaken with 14 pregnant women recruited in the prenatal clinics of the same two locations. Women answered open-ended questions designed to address barriers to prenatal care: accessibility of care, quality of health care provided, past experiences, and other barriers to prenatal care access. Interviews were conducted by one of the authors (CB) and a trained Samoan interviewer in either English or Samoan according to interviewee’s personal preference. Interviews conducted in Samoan were translated before transcription. The complete findings of this study are described elsewhere [15] but representative quotes from these interviews are included in the discussion section of this manuscript to anecdotally support the quantitative data from the prenatal clinic records.
Results
Sample Characteristics
Of the women included in the study sample, 135 were primiparous (19.5%) while 189 (27.3%) had delivered four or more infants (Table 1). The average week of gestation at which women attended their first prenatal visit was 24.74 (±7.80) weeks and the average number of prenatal care visits attended was 6.60 (±3.47).
Table 1.
Characteristics of the Study Sample
| n | Mean | SD | |
|---|---|---|---|
| Maternal Age (years) | 692 | 28.16 | 5.55 |
| Parity | 692 | 2.43 | 2.03 |
| Week of Gestation at First Prenatal Care visit | 692 | 24.74 | 7.80 |
| Trimester of First Prenatal Care visit (%) | 692 | ||
| First Trimester | 59 (8.5) | ||
| Second Trimester | 339 (49.0) | ||
| Third Trimester | 294 (42.5) | ||
| Total Number of Prenatal Care Visits | 692 | 6.60 | 3.47 |
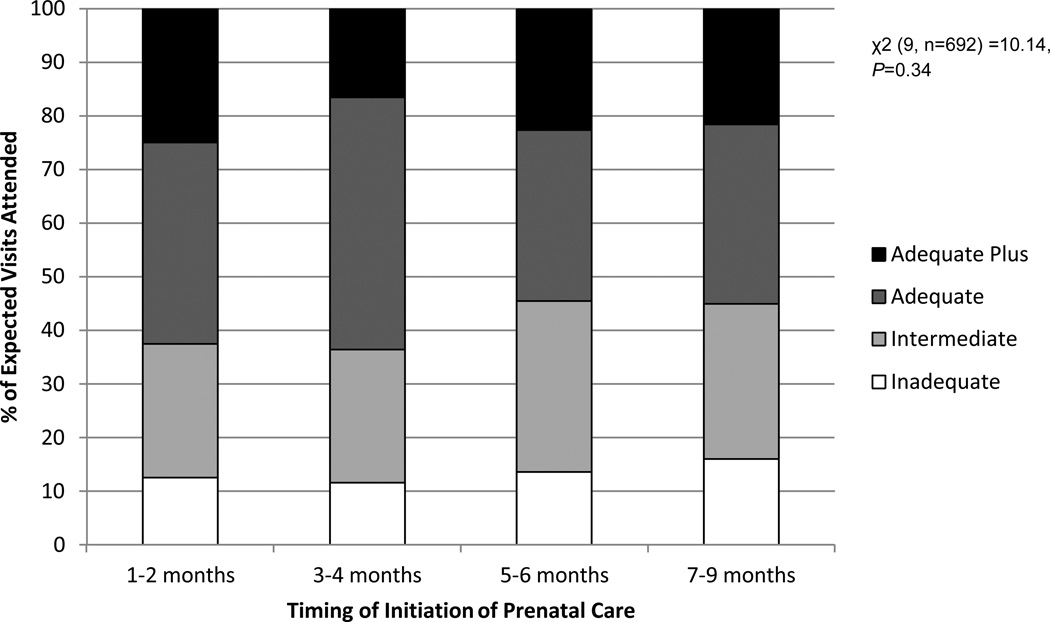
Adequacy of Prenatal Care Utilization
More than half of the sample (50.6%) received inadequate prenatal care based on initiation, only attending their first prenatal visit in the seventh month of pregnancy or later (Table 2). Adequacy of received services once prenatal care was initiated was substantially better with 56.5% of women receiving adequate or adequate plus care. The summary APNCU index shows that, based on both initiation and received services, 85.4% of the sample received inadequate prenatal care. Adequacy of received services was not associated with the timing of prenatal care initiation (Figure 1).
Table 2.
Frequency of adequate care based on the Adequacy of Prenatal Care Utilization Index
| n | % | |
|---|---|---|
| Adequacy of Initiation of Prenatal Carea | ||
| Adequate Plus | 8 | 1.2 |
| Adequate | 121 | 17.5 |
| Intermediate | 213 | 30.8 |
| Inadequate | 350 | 50.6 |
| Adequacy of Received Servicesb | ||
| Adequate Plus | 146 | 21.1 |
| Adequate | 245 | 35.4 |
| Intermediate | 201 | 29.0 |
| Inadequate | 100 | 14.5 |
| Summary Adequacy of Prenatal Care Utilization Indexc | ||
| Adequate Plus | 18 | 2.6 |
| Adequate | 54 | 7.8 |
| Intermediate | 29 | 4.2 |
| Inadequate | 591 | 85.4 |
Adequacy of Initiation of Prenatal Care: Month prenatal care began. Adequate Plus: 1st or 2nd month; Adequate: 3rd or 4th month; Intermediate: 5th or 6th month; Inadequate: 7th month or later or no prenatal care
Adequacy of Received Services: Proportion of the number of visits recommended by the American College of Obstetrics and Gynecologists received from the time prenatal care began until delivery. Adequate Plus: ≥110%; Adequate: 80–109%; Intermediate: 50–79%; Inadequate: <50%
Summary Adequacy of Prenatal Care Utilization Index: Adequate Plus: Prenatal care begun by the 4th month and 110% or more of recommended visits received; Adequate: Prenatal care begun by the 4th month and 80–109% of recommended visits received; Intermediate: Prenatal care begun by the 4th month and 50–79% of recommended visits received; Inadequate: Prenatal care begun after the 4th month OR less than 50% of recommended visits received
Figure 1.
Adequacy of received services according to the timing of initiation of prenatal care
Socio-demographic Predictors of the Timing of Prenatal Care Initiation and the Adequacy of Received Services
Significant predictors of the timing of prenatal care initiation were parity, maternal occupation and the combined employment status of both parents (Table 3). Parity was negatively associated with prenatal care initiation with women who had delivered four or more infants initiating prenatal care more than two weeks later than primiparous women (25.81 vs. 23.39 weeks, P=0.02). Unemployment was associated with later prenatal care initiation; women who were unemployed accessed prenatal care significantly later than their peers who were employed in management, professional or sales occupations (P=0.04). Having a partner who was also unemployed further delayed the initiation of prenatal care. Women in this situation accessed prenatal care more than four weeks later than women who were employed themselves and also had an employed partner (27.61 vs. 23.50 weeks; P=0.03).
Table 3.
Timing of the first prenatal care visit and the adequacy of received services according to maternal and paternal socio-demographic characteristics
| n (%) | Week of Gestation at First Prenatal Visit Mean (SD) |
Percentage of Expected Prenatal Visits Attended Mean (SD) |
|||
|---|---|---|---|---|---|
| Maternal Age | 692 | ||||
| < 20 years | 38 (5.5) | 24.31 (8.05) | F= 0.26 P= 0.86 |
84.12 (37.85) | F= 0.37 P= 0.78 |
| 20–29 years | 384 (55.5) | 24.83 (7.84) | 85.31 (45.53) | ||
| 30–39 years | 252 (36.4) | 24.78 (7.61) | 85.24 (34.89) | ||
| > 40 years | 18 (2.6) | 23.32 (9.30) | 95.43 (37.09) | ||
| Parity | 692 | ||||
| Primiparous | 135 (19.5) | 23.39 (7.79) | F= 3.85 P= 0.02* |
88.13 (38.44) | F= 1.03 P= 0.36 |
| < 4 | 368 (53.2) | 24.69 (7.79) | 86.32 (45.68) | ||
| ≥ 4 | 189 (27.3) | 25.81 (7.70) | 81.98 (33.44) | ||
| Family History of Multiple Births | 671 | ||||
| No | 332 (49.5) | 24.68 (8.07) | t= −0.20 P= 0.84 |
87.81 (46.84) | t= 1.51 P= 0.13 |
| Yes | 339 (50.5) | 24.80 (7.48) | 83.00 (34.83) | ||
| Maternal Marital Status | 665 | ||||
| Single | 126 (18.9) | 24.87 (7.96) | t= 0.30 P= 0.76 |
85.49 (56.47) | t= 0.12 P= 0.90 |
| Married/Cohabiting | 539 (81.1) | 24.64 (7.78) | 84.99 (36.79) | ||
| Maternal Occupation | 673 | ||||
| Unemployed | 394 (56.9) | 25.36 (7.63) | F= 3.49 P= 0.03* |
84.83 (37.33) | F= 0.38 P= 0.69 |
| Management/Professional/Sales | 199 (28.8) | 23.72 (7.77) | 89.24 (67.00) | ||
| Service/Construction/Elementary Occupations/Student | 80 (11.6) | 23.88 (8.40) | 85.89 (35.54) | ||
| Maternal Education | 311 | ||||
| Less than High School | 53 (17.0) | 25.74 (7.19) | F= 0.39 P= 0.68 |
82.93 (43.73) | F= 0.11 P= 0.90 |
| Completed High School | 202 (65.0) | 25.26 (7.66) | 84.36 (34.78) | ||
| College / Higher Education | 56 (18.0) | 24.47 (8.19) | 86.10 (30.91) | ||
| Paternal Age | 484 | ||||
| 20–29 years | 166 (34.3) | 24.75 (8.08) | F= 0.73 P= 0.48 |
86.61 (39.70) | F= 1.94 P= 0.14 |
| 30–39 years | 247 (51.0) | 24.16 (7.72) | 87.20 (35.87) | ||
| > 40 years | 71 (14.7) | 25.34 (7.66) | 77.74 (30.83) | ||
| Paternal Occupation | 510 | ||||
| Unemployed | 33 (6.5) | 27.28 (7.35) | F= 1.87 P= 0.13 |
93.45 (57.86) | F= 1.41 P= 0.24 |
| Management/Professional/Sales | 78 (15.3) | 24.67 (8.32) | 87.61 (33.40) | ||
| Service/Construction/Elementary Occupations/Student | 382 (74.9) | 24.48 (7.57) | 84.23 (34.88) | ||
| Farming | 17 (3.3) | 22.28 (9.04) | 72.60 (40.57) | ||
| Parental Employment | 503 | ||||
| Both Unemployed | 20 (4.0) | 27.61 (7.49) | F= 3.01 P=0.03* |
92.41 (48.68) | F= 0.63 P= 0.60 |
| Both Employed | 187 (37.2) | 23.50 (7.99) | 84.42 (31.60) | ||
| Mother Employed Only | 13 (2.6) | 26.78 (7.41) | 95.04 (71.92) | ||
| Father Employed Only | 283 (56.3) | 25.09 (7.52) | 84.43 (37.18) |
Main Effects Significant:
P < 0.05;
P < 0.01
Year of Delivery
The year in which a woman delivered her infant was associated with both the initiation of prenatal care and the adequacy of received services. Women who delivered in 2007 or 2008 after the introduction of the prenatal incentive scheme accessed prenatal care significantly earlier than women who delivered before the scheme began (P<0.01) and attended a significantly greater percentage of their expected appointments (95.04% vs. 83.80 %, P= 0.02).
Discussion
This study suggests that between 2001 and 2008 the utilization of prenatal care in American Samoa was poor, with 85.4% of the sample classified as receiving inadequate care based on a combination of the timing of initiation of prenatal care and the adequacy of received services after initiation. Data from the U.S. Pregnancy Risk Assessment and Monitoring System (PRAMS) suggests that approximately 80% of women initiate prenatal care in the first trimester [16]. With only 8.5% of women accessing first trimester care in American Samoa the urgent need for improvement is clear.
Despite their late initiation of prenatal care the qualitative interviews conducted with women in the prenatal clinics suggest that knowledge of the importance of prenatal care is ubiquitous among Samoan women. Women reflected that “Prenatal care is so important for a healthy baby and for us” and stressed that “….It’s very, very important. You know for the sake of the mom and the baby. For the safety of the unborn…..” Even so, prenatal care access was late and sporadic. Some of the socio-demographic predictors of prenatal care adequacy give an insight as to the barriers to adequate prenatal care utilization in this setting.
Potential Barriers to Adequate Prenatal Care Utilization
Parity
In a recent systematic review of factors affecting the utilization of prenatal care in LMIC, parity was negatively associated with adequacy of prenatal care [17]. In those studies, and in this sample, this association may reflect the fact that multiparous women who have had previous positive experiences of pregnancy may feel more confident having been through pregnancy several times before or may feel that they have already heard all of the advice that healthcare professionals have to offer. Alternatively, women who had a previous negative experience with pregnancy, delivery, or in their interactions with healthcare providers may not have wanted to go back in subsequent pregnancies [18]. Multiparous women may also be likely to face time pressures associated with already having multiple children or issues with childcare arrangements for while they attend appointments. Large families in particular may have very limited family resources meaning that the cost of prenatal care is not prioritized.
Unemployment
Unemployment was a significant barrier to adequate prenatal care utilization in this study and also in many other studies [17]. While unemployed mothers may not face the same pressure on their time as women who are employed they are more likely to have very limited resources. Indeed, when asked about barriers to accessing prenatal care resources and income were frequently mentioned by Samoan women: “I think it all depends on the resources that you have, in order to get here or to pay for it. I think that’s a major problem for some, but not for me right now.”
Other Potential Barriers to Prenatal Care
As the information presented here was based upon antenatal clinic records only the available socio-demographic variables could be explored and there may be many alternative explanations as to why these American Samoan women were not adequately utilizing prenatal care. Early recognition of pregnancy, which is associated with improved timing of prenatal care visits [16], may not be common or, as some women expressed in the in-depth surveys there may be hesitance to attend based on a lack of knowledge and anxiety about what prenatal care entails: [Being translated from Samoan]: “she says that she was so scared to come in to do her prenatal care that she waited a while to come in”. In other studies, wantedness of the pregnancy is also a significant predictor of prenatal care adequacy [19,20].
American Samoa, like many other developing populations, particularly island populations, experiences issues with its healthcare infrastructure: interruptions in service based on supply of medications or power [21], a lack of qualified healthcare professionals, which is a particular issue in the Pacific Islands [21,9], and problems with central location of their main healthcare facilities when large proportions of the population live in remote areas [22]. A common theme relating to this among the qualitative interviews was lack of car ownership and the need to rely on buses: “I couldn’t come because of the transportation, you know the buses. Most of the women, they don’t have their own ride or car so they have to catch the bus to come in to their checkups, their follow ups. So maybe that’s a hard thing….”. Similarly, having to wait a long time for appointments because of a lack of doctors was a recurring theme of the qualitative surveys: “I mean sometimes you have to wait really long. If you come earlier, we have to wait like 45 minutes” “Yeah, it [prenatal care] is accessible, the only problem is there are not enough doctors. So like waiting periods you know... People who come early you know, they are waiting so long”.
Data from the U.S. suggests that inadequate prenatal care utilization is not confined to Samoans in the island nations, but it is also a health risk behavior that remains among migrant Samoan communities. Data from the US Department of Health and Human Services states that nearly 52% of Samoan women do not begin prenatal care in the first trimester; a far greater proportion than in any other racial or ethnic group [23]. In Utah, where there is a particularly large Pacific Island community, 52.7% of Pacific Island women received inadequate care based on the APNCU index compared to 18.6% of all Utahns [24]. These adequacy reports may be a reflection of the socio-economic position of Pacific Islanders among their communities, however it suggests that perhaps unique cultural beliefs around prenatal care utilization should be given attention in future research.
Attempts to Improve Prenatal Care Utilization in American Samoa
The year of delivery was significantly associated with both the timing of initiation and the adequacy of received prenatal services after initiation, with both the timing of initiation and the adequacy of received services improved in 2007–2008 versus earlier years. This finding likely reflects several attempts by the American Samoan Medical Center Authority, which operates the LBJ Hospital, and the Department of Health to improve prenatal care utilization. Importantly, in 2006 LBJ introduced a prenatal care incentive scheme. In its design the program addresses both dimensions of prenatal care utilization. Women qualify for the program if they attend their first prenatal care visit before the end of the first trimester and agree to attend at least 80% of all prenatal care appointments thereafter. In return, women receive free medical services at LBJ’s OB/GYN clinic, two free ultrasound scans and two nights of free care in labor and delivery. With current prenatal care costs high, particularly for the uninsured, the prenatal program offers a significant monetary incentive for taking early advantage of prenatal care. Interviews with Samoan women in 2010 indicated that there was widespread knowledge of the program. When asked about who advised her about receiving prenatal care one woman responded “…. Mostly my sisters at home, they talk to me about the prenatal program. They said that I have to register within three months”, she goes on to say “….if I give birth there will be no bill, no fees, or in the labor room and the delivery room. There will be no fees for that. Even for my like, appointments… they give you a pass for seeing the doctor.” The improved utilization of prenatal care in 2007–2008 speaks to the early efficacy of this program but continued long-term monitoring and research quality evaluation are needed to confirm its success.
Since these data were collected in 2008 there have also been significant changes to the healthcare infrastructure in American Samoa, which should have further positive impacts on prenatal care utilization. The opening of two additional community health centers in the villages of Amouli and Leone in 2009 made prenatal care more accessible to residents of the Eastern and Western Districts which had previously been underserved communities. Prenatal care is now available at a clinic within a one hour bus ride from any point on the island [25]. At the Tafuna clinic an afterhours program was introduced and staffed by a nurse practitioner, allowing women to come in after 4pm for prenatal care. Additionally, federally supported Women, Infants, and Children (WIC) program offices were re-located into the Amouli and Leone community health centers in 2010 making it easier for women to register for prenatal care and WIC benefits simultaneously. Another WIC office will be moved into the Tafuna clinic in 2013. Again, future research to understand the impact of these programs on prenatal care utilization is necessary. Understanding what population groups benefited from these changes will allow further targeting and elaboration of such programs.
Importance of Prenatal Care in this Setting
Universal access to prenatal care is important to protect the health of both mother and infant [14]. A unique feature of the Samoan population, which is pertinent in the discussion of prenatal care provision, is the ubiquitous nature of overweight and obesity in women of childbearing age. In 2002, more than 76% of women of childbearing age (25–34 years) were obese (BMI >32 kg/m2) [26]. The prenatal care records reviewed here did not include pre-pregnancy BMI so we cannot comment on this sample specifically but the general levels of overweight and obesity characteristic of this population mean that there may be serious consequences of inadequate prenatal care. Pacific Island women are known to be at increased risk for acquiring GDM [27–29] and have higher rates of reoccurrence in subsequent pregnancies [30]. GDM screening should take place at 24–28 weeks gestation with an oral glucose tolerance test to allow for adequate monitoring and management of the condition [31]. Of the women in this sample, 232 (33.5%) attended their first prenatal care visit after this window and GDM status was not recorded. Overweight and obese women are also those most likely to exceed IOM guidelines for gestational weight gain [32] leading to increased risk of fetal macrosomia, labor abnormalities, postdatism, unscheduled cesarean sections [33] and future obesity risk for the offspring [34].
Limitations
Our description of prenatal care adequacy in American Samoa and the barriers to prenatal care access has several limitations. The first is that these records were not collected for the specific purpose of investigating prenatal care utilization, therefore the analysis was limited to those socio-demographic variables available. Secondly, because these records were obtained from the prenatal clinic records of women, they do not include any women who received no prenatal care before delivery. Recent reports suggest that approximately 7% of women in American Samoa receive no prenatal care [25]. These women may have different socio-demographic characteristics from the current study sample and therefore this study does not speak to why women do not access any prenatal care. Thirdly, the APNCU index has known limitations. Those women who received ‘adequate plus’ care based on the number of visits attended may have been those who were at high risk, based on previous pregnancies or preexisting conditions, and required more frequent monitoring. Fourthly, basing the adequacy of prenatal care received on the timing of initiation and the number of visits attended does not speak to the quality of the prenatal care provided. While women interviewed attested to the quality of prenatal care, interviews were conducted within a private room in the prenatal clinic itself, which may have prevented women expressing their true feelings about the quality of care for risk of their answers being shared with clinic staff and their subsequent care being affected.
Despite these limitations this study has significant strengths. The sample recruited represents a range of socio-demographic characteristics and includes approximately 10% of the deliveries we would expect to have occurred in American Samoa over the study period. Additionally, the qualitative interviews, despite the fact they were completed some time after the quantitative data collection and likely reflect the opinion of those with access to the prenatal program, appear to support the validity of our findings.
Conclusions
During the period between 2001 and 2008 prenatal care utilization in American Samoa was poor, which is a major concern. Prenatal care utilization was associated with several maternal socio-demographic characteristics which suggest that improving healthcare accessibility will be key in encouraging women to attend prenatal care. The significant improvements in the timing of initation of prenatal care and the utilization of received services seen in 2007–2008 suggest that the prenatal care incentive program implemented at LBJ in 2006 is a very positive step toward addressing issues of prenatal care utilization in this population.
Figure 2.
Adequacy of Prenatal Care Utilization based on Prenatal Incentive Scheme availability
Acknowledgements
Financial support was partially provided by US NIH grant R18-DK075371 and the Brown University Undergraduate Teaching and Research Assistantship program. We acknowledge the Tafuna Clinic, American Samoa Community Health Centers, Department of Health, and the American Samoa Community College Community and Natural Resources program for providing resources and assistance in the field. We thank the LBJ Tropical Medical Center prenatal clinic health care workers for their cooperation and the women who participated in the qualitative research for their cooperation and trust.
References
- 1.United Nations. [accessed Jan 29, 2013];Road map towards the implementation of the United Nations Millennium Declaration: report of the Secretary General. 2001 http://www.un.org/documents/ga/docs/56/a56326.pdf. [Google Scholar]
- 2.Stout A. Prenatal Care for Low-Income Women and the Health Belief Model: A New Beginning. J Community Health Nurs. 1997;14(3):169–180. doi: 10.1207/s15327655jchn1403_4. [DOI] [PubMed] [Google Scholar]
- 3.World Health Organization. Maternal Mortality. Fact Sheet No348; 2012. [accessed Jan 29 2013]. http://www.who.int/mediacentre/factsheets/fs348/en/index.html. [Google Scholar]
- 4.Say L, Raine R. A systematic review of inequalities in the use of maternal health care in developing countries: examining the scale of the problem and the importance of context. Bull World Health Organ. 2007;85(10):812–819. doi: 10.2471/BLT.06.035659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kotelchuck M. An evaluation of the Kessner adequacy of prenatal care index and a proposed adequacy of prenatal care utilization index. Am J Public Health. 1994;84(9):1414–1420. doi: 10.2105/ajph.84.9.1414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.US Central Intelligence Agency. [accessed Jan 30, 2013];The World Factbook. 2013 https://www.cia.gov/library/publications/the-world-factbook/geos/aq.html.
- 7.American Samoa Department of Commerce. [accessed Jan 30 2013];American Samoa at-a-glance. 2006 www.spc.int/prism/country/as/stats/At_A_Glance_2006.pdf. [Google Scholar]
- 8.Binns C, Hokama T, Low WY. Island health: hope and challenges for public health. Asia- Pac J Public Health. 2010;22(1):19–24. doi: 10.1177/1010539509357782. [DOI] [PubMed] [Google Scholar]
- 9.Yamamoto TS, Sunguya BF, Shiao LW, et al. Migration of health workers in the Pacific Islands: a bottleneck to health development. Asia-Pac J Public Health. 2012;24(4):697–709. doi: 10.1177/1010539512453259. [DOI] [PubMed] [Google Scholar]
- 10.Health Services and Resource Administration. [accessed Jan 29 2013];Designated health professional shortage areas. 2013 http://bhpr.hrsa.gov/shortage/ [Google Scholar]
- 11.Low P, Paterson J, Wouldes T, et al. Factors affecting antenatal care attendance by mothers of Pacific infants living in New Zealand. New Zeal Med J. 2005;118(1216):1489–1499. [PubMed] [Google Scholar]
- 12.U.S. Census Bureau. [accessed Jun 29 2012];Census Population Count Data Note 1 – American Samoa. 2010 http://www.2010.census.gov/news/doc/errata_note.doc.
- 13.Hawley NL, Johnson W, Nu’usolia O, et al. The contribution of feeding mode to obesogenic growth trajectories in American Samoan infants. Pediatr Obes. 2013 doi: 10.1111/j.2047-6310.2012.00137.x. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.American College of Obstetricians and Gynecologists. Manual of Standards in Obstetric- Gynecologic Practice. 2nd Ed. Chicago, IL: 1965. [Google Scholar]
- 15.Brown C. Barriers to Prenatal Care in American Samoa. Providence, RI, USA: Unpublished undergraduate thesis, Brown University; 2011. [Google Scholar]
- 16.Ayoola AB, Nettleman MD, Stommel M, et al. Time of pregnancy recognition and prenatal care use: a population-based study in the United States. Birth. 2010;37(1):37–43. doi: 10.1111/j.1523-536X.2009.00376.x. [DOI] [PubMed] [Google Scholar]
- 17.Simkhada B, van Teijlingen ER, Porter M, et al. Factors affecting the utilization of antenatal care in developing countries: systematic review of the literature. J Adv Nurs. 2007;61(3):244–260. doi: 10.1111/j.1365-2648.2007.04532.x. [DOI] [PubMed] [Google Scholar]
- 18.Goldenberg RL, Patterson ET, Freese MP. Maternal demographic, situational and psychosocial factors and their relationship to enrollment in prenatal care: a review of the literature. Women Health. 1992;19(2-3):133–151. doi: 10.1300/J013v19n02_08. [DOI] [PubMed] [Google Scholar]
- 19.Magadi MA, Madise NJ, Rodrigues RN. Frequency and timing of antenatal care in Kenya: explaining the variations between women of different communities. Soc Sci Med. 2000;51(4):551–561. doi: 10.1016/s0277-9536(99)00495-5. [DOI] [PubMed] [Google Scholar]
- 20.Paredes I, Hidalgo L, Chedraui P, et al. Factors associated with inadequate prenatal care in Ecuadorian women. Int J Gynaecol Obstet. 2005;88(2):168–172. doi: 10.1016/j.ijgo.2004.09.024. [DOI] [PubMed] [Google Scholar]
- 21.World Health Organization. Western Pacific Country Health Information Profiles. [accessed Jan 30 2013];2011 Revision. 2011 http://www.wpro.who.int/health_information_evidence/documents/CHIPS2011.pdf.
- 22.World Health Organization Representative Office in the South Pacific. Health Sector Development. [accessed Jan 30 2013];2008 http://www2.wpro.who.int/southpacific/sites/hsd/
- 23.Office of Women’s HealthU.SDepartment of Health and Human Services. Women of Color Health Data Book. [accessed Jan 13 2013];2000 http://www.4woman.gov/owh/pub/woc/toc.htm.
- 24.Utah Department of Health. Utah Health Disparities Summary 2009: Pacific Islanders. [accessed Jan 30 2013];2009 http://health.utah.gov/disparities/data/disparitiessummary/PacificIslanderFactSheet.pdf.
- 25.American Samoa MCH Program. [accessed Jan 30 2013];Assets and needs assessment - 2010. 2010 https://mchdata.hrsa.gov/tvisreports/Documents/NeedsAssessments/2011/AS-NeedsAssessment.pdf.
- 26.Keighley ED, McGarvey ST, Turituri P, et al. Farming and adiposity in Samoan adults. Am J Hum Bio. 2006;18(1):112–121. doi: 10.1002/ajhb.20469. [DOI] [PubMed] [Google Scholar]
- 27.Yapa M, Simmons D. Screening for gestational diabetes mellitus in a multiethnic population in New Zealand. Diabetes Res Clin Pract. 2000;48(3):217–223. doi: 10.1016/s0168-8227(99)00150-3. [DOI] [PubMed] [Google Scholar]
- 28.Hunsberger M, Rosenberg KD, Donatelle RJ. Racial/ethnic disparities in gestational diabetes mellitus: findings from a population-based survey. Womens Health Issues. 2010;20(5):323–328. doi: 10.1016/j.whi.2010.06.003. [DOI] [PubMed] [Google Scholar]
- 29.Chu SY, Abe K, Hall LR, et al. Gestational diabetes mellitus: all Asians are not alike. Prev Med. 2009;49(2-3):265–268. doi: 10.1016/j.ypmed.2009.07.001. [DOI] [PubMed] [Google Scholar]
- 30.Getahun D, Fassett MJ, Jacobsen SJ. Gestational diabetes: risk of recurrence in subsequent pregnancies. Am J Obstet Gynecol. 2010;203(5):467.e1–467.e6. doi: 10.1016/j.ajog.2010.05.032. [DOI] [PubMed] [Google Scholar]
- 31.American College of Obstetricians and Gynecologists. Screening and diagnosis of gestational diabetes mellitus. Committee Opinion No. 504. Obstet Gynecol. 118(3):751–753. doi: 10.1097/AOG.0b013e3182310cc3. [DOI] [PubMed] [Google Scholar]
- 32.Institute of Medicine. Weight gain during pregnancy: Reexamining the guidelines. Washington, DC: The National Academies Press; 2009. [PubMed] [Google Scholar]
- 33.Johnson JWC, Longmate JA, Frentzen B. Excessive maternal weight and pregnancy outcome. Am J Obstet Gynecol. 1992;167(2):353–372. doi: 10.1016/s0002-9378(11)91414-8. [DOI] [PubMed] [Google Scholar]
- 34.Nehring I, Lehmann S, von Kries R. Gestational weight gain in accordance to the IOM/NRC criteria and the risk for childhood overweight: a meta-analysis. Pediatr Obes. 2013 doi: 10.1111/j.2047-6310.2012.00110.x. 2012 Nov 21. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]