Caduceus
The early results of the CArdiosphere-Derived aUtologous stem CElls to reverse ventricUlar dySfunction study were recently published in the Lancet. 1 This study is a phase 1 prospective randomised study, performed at two centres. The study was designed to test the hypothesis that intracoronary infusion of autologous cardiac-derived cells following myocardial infarction can reduce the size of the infarct and increase the amount of viable myocardium. The eligible patients were randomised in a 2:1 ratio to receive CDCs or standard care. In all, 17 patients were randomised to cell therapy and 8 to standard care. The cell therapy consisted of an infusion of 25 million cells into the infarct related artery, 1.5–3 months after successful primary angioplasty in patients who developed LV dysfunction (EF less than 37 per cent). The cells were derived from RV endomyocardial biopsies performed within the previous 37 days. The number of cells was determined from previous experimental studies of the maximum number of cells which can be injected without inducing infarction. The study was not blinded because of ethical considerations regarding performing right ventricular biopsy on the controls. The exclusion criteria included patients who had evidence of right ventricular infarction, or could not have an MRI examination because of claustrophobia or prior insertion of devices. There was no death, myocardial infarction or serious arrhythmia reported in either group during the period of follow up, which was between 6–12 months. Serious adverse events were observed in 24 percent of the intervention group versus 12 per cent in the controls (p not significant).
Although the study was not powered to determine efficacy, the authors observed significant reduction in the size of the infarct ( − 7.7 per cent at 6 month and − 12.3 per cent at 12 months) and importantly an increase in the amount of viable myocardium. In addition there was a significant increase in the thickness and rate of thickening in the peri-infarction zone, however there was no change in ejection fraction of left ventricular volumes.
The authors concluded that injection of a specific number of CDCs into the infarct related artery is safe and should be tried further.
The strong points in this trial are the fact that it has shown for the first time that injection of CDCs in humans is feasible and safe, and that this might increase the amount of viable myocardium and therefore influence longer-term outcome. The study was started after extensive preclinical research by the authors, to justify moving into the clinic. In addition the choice of MRI to assess results enhances the ultimate value of the study.
What have we learned?
In spite of the fact that the results of the study are potentially very exciting, they are not sufficient to influence practice, because of the small number of patients, the short period of follow up, the putative nature of the results, and the limit imposed on the number of cells which can be safely injected into the coronary arteries because of the large size of the CDCs (20 microns in diameter) which is considerably larger than the myocardial capillaries (7 microns).
In addition, although the CDCs are cardiac derived and have been labelled progenitor cells, there is no evidence that they can differentiate into myocardial cells, and therefore the mechanisms involved in the beneficial actions observed remain unknown. Recent studies using carbon-14 or multi-isotope imaging mass spectrometry (MIMS), suggest that myocardial regeneration following injury results from division of mature myocardial cells. Future reports about the longer term results from the same group in phase 2 trials are awaited with great interest, while other strategies to enhance division of adult cardiomyocytes 2–6 should be actively explored.
Scipio
The early results of the phase 1 trial, cardiac Stem Cell In Patients with Ischemic cardiomyopathy (SCIPIO) were recently published in The Lancet. 7 This trial appears to have raised expectations to an unrealistic degree with the hope that “it will transform cardiac cell therapy that its namesake, Scipio Africanus achieved in Roman Military Campaigns”. 8 The trial is an open label randomised trial of patients with post infarction left ventricular dysfunction (EF less than 45 per cent) requiring surgical revascularisation. At the time of operation, performed at one of two centres in Kentucky, the atrial appendage was excised and sent to Dr Piero Anversa's lab in Boston. Following cell culture, cells expressing the cell surface marker c-kit, which are also lineage negative, were extracted using magnetic beads and thoroughly characterised and tested for lack of senility and ability to proliferate. The cells were then shipped to another lab in Kentucky to be prepared for clinical use. For the patients randomised to the cell therapy arm, intra-coronary injection of the specified number of cells were injected into the graft or vessel supplying the infarction area about 120 days after operation. For patients with large anterior infarcts, one million cells were injected, while for patients with smaller posterior infarcts one or more injections of 500,000 cells were used. The primary end point was short-term safety and the secondary end point was efficacy as determined by clinical, quality of life questionnaire and MRI at 1 and 4 months. Patient recruitment utilised a complex system with the first nine consecutive eligible patients assigned to cell therapy and the next four conseutivec patients acting as controls. After that patients were randomised in a 3:2 ratio to treatment and controls. In all, 16 patients received cells and 7 were controls.
The authors report no mortality or major adverse events following this form of therapy. In addition, although the study was not powered to address efficacy, in the patients who could be investigated by MRI, there was improvement in EF by 8 and 12 percent at one and four-year time points in the cell therapy group, as opposed to no improvement in the controls. There was also evidence of diminution in the size of the infarct in the cell therapy group. These results are superior to those described after infusion of bone marrow derived cells. However the numbers are small, and the potential confounding effect of myocardial revascularisation cannot be excluded.
What have we learned?
The results of this phase 1 trial are unlikely to influence practice because of the putative nature of the findings and the small number of patients. The results of the phase 2 trial will be eagerly awaited. Similarly, studies to define the mechanism of changes observed would be of great value. In the meantime, the major expectations have to wait (Figure 1).
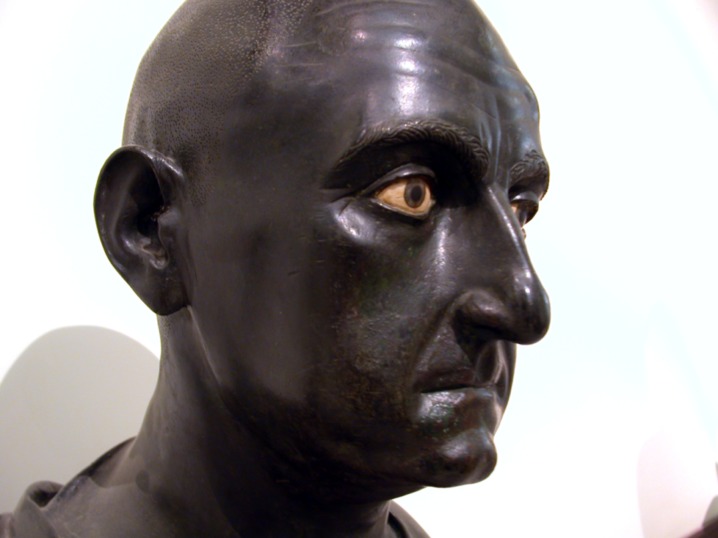
Figure 1. .
Scipio Africanus The Elder was a general in the Second Punic War and statesman of the Roman Republic. He was best known for defeating Hannibal at the final battle of the Second Punic War at Zama, a feat that earned him the agnomenAfricanus, the nickname “the Roman Hannibal”, as well as recognition as one of the finest commanders in military history. Picture credit: http://upload.wikimedia.org/wikipedia/commons/3/38/Scipio_Africanus_the_Elder.jpg
Alcadia
Results of the ALCADIA (AutoLogous Human CArdiac-Derived Stem Cell To Treat Ischemic cArdiomyopathy) trial were presented during the American Heart Association Scientific Sessions in November 2012. 9 The study evaluated a hybrid cell therapy application, namely the administration of autologous cardiac stem cells together with a controlled release formulation of basic Fibroblast Growth Factor (bFGF) in patients with ischemic cardiomyopathy and heart failure.
This is one of the first human trials, together with CADUCEUS and SCIPIO, where cardiac derived cells are used to treat heart failure. ALCADIA is the smallest and most preliminary of them and the final results have not been published yet.
ALCADIA was an open label, non-randomized, phase 1 safety/feasibility study of autologous cardiac derived stem cell combined with bFGF administration in advanced heart failure. 9 Six patients (55.5 ± 10.8 years old, 5 men and one woman) with ischemic cardiomyopathy (left ventricular ejection fraction between 15 and 45%), symptomatic heart failure (NYHA class III or IV), myocardial viability and indication for coronary artery bypass surgery, were enrolled.
Cardiac-derived stem cells were grown from endomyocardial biopsies and expanded for a period of approximately one month. They were delivered to the heart during the subsequent CABG surgery, by 20 intramyocardial injections (total number 0.5million/kg). Finally, a biodegradable gelatin hydrogel sheet containing 200μg of bFGF was implanted on the epicardium, covering the injection sites areas.
The primary safety end point was the occurrence of Major Cardiac Event (MACE) during the one year follow up period. Efficacy end points included changes in Left Ventricular Ejection Fraction (LVEF, assessed by echocardiography and MRI), infarct volume (assessed by MRI) and symptoms (NYHA class and exercise capacity) at 6 months.
One patient experienced acute occlusion of a graft 3 weeks after surgery and was excluded from further evaluation. From the remaining five patients, one experienced a worsening heart failure episode during the follow up. No other serious adverse events were observed. At 6 months, there was an increase in LVEF measured by both imaging modalities (9% and 12%, by echocardiography and MRI respectively). Infarct size decreased by 3.3% of the total LV volume and maximal aerobic exercise capacity (VO2peak) increased by 4.5 ml/kg/min.
What have we learned?
The ALCADIA trial is a small, preliminary Phase 1 study without a control group. No conclusions about the efficacy of this hybrid therapy can be derived. The favorable trends observed in LV function and symptom severity can also be attributed to the effects of revascularization. In the small number of patients (five) who were followed for 12 months, there was only one serious adverse event, related to worsening heart failure; therefore, no concerns about safety were raised.
The concept is interesting since poor cell survival is currently one of the major hurdles limiting the effectiveness of cell therapies, irrespective of the type of the cell used. Tissue engineering approaches may offer a solution to this problem. In this study, a sustained release bFGF gelatin hydrogel sheet was used, in order to augment the effect exerted by the cells. The investigators have previously shown the efficacy of this method in a preclinical animal model. 10 FGF has many attractive properties, since it promotes cell proliferation and angiogenesis. The cardiac derived cells used in ALCADIA were autologous and were grown from endomyocardial biopsies. The cells have surface markers characteristic of mesenchymal cells (CD105 and CD90), but also express transcription factors characteristic of progenitor cells. It should be noted however that there is no compelling evidence that these cells can differentiate into cardiomyocytes in vivo and most experimental studies suggest a paracrine mechanism of action, leading to augmentation of endogenous repair mechanisms (both cardiomyocyte proliferation and recruitment of resident cardiac stem cells). 11
In conclusion, the ALCADIA trial has demonstrated the safety of the combined administration of autologous cardiac derived stem cells together with a sustained bFGF gelatin hydrogel in patients with ischemic cardiomyopathy. Larger, prospective, randomized, placebo control clinical trials are required in order to investigate the effectiveness of this approach.
References
- [1].Makkar RR, Smith RR, Cheng K, Malliaras K, Thomson LE, Berman D, Czer LS, Marbán L, Mendizabal A, Johnston PV, Russell SD, Schuleri KH, Lardo AC, Gerstenblith G, Marbán E. Intracoronary cardiosphere-derived cells for heart regeneration after myocardial infarction (CADUCEUS): a prospective, randomised phase 1 trial. Lancet. 2012;379(9819):895–904. doi: 10.1016/S0140-6736(12)60195-0. Available at: http://dx.doi.org/10.1016/S0140-6736(12)60195-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Bergmann O, Bhardwaj RD, Bernard S, Zdunek S, Barnabe-Heider F, Walsh S, Zupicich J, Alkass K, Buchholz BA, Druid H, Jovinge S, Frisen J. Evidence for cardiomyocyte renewal in humans. Science. 2009;324(5923):98–102. doi: 10.1126/science.1164680. Available at: http://dx.doi.org/10.1126/science.1164680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3]. Senyo SE, Steinhauser ML, Pizzimenti CL, Yang VK, Cai L, Wang M, Wu T-D, Guerquin-Kern J-L, Lechene CP, Lee RT. Mammalian heart renewal by pre-existing cardiomyocytes Nature 2012. 493 7432 433 436 Available at: http://dx.doi.org/10.1038/nature11682 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Porrello ER, Mahmoud AI, Simpson E, Johnson BA, Grinsfelder D, Canseco D, Mammen PP, Rothermel BA, Olson EN, Sadek HA. Regulation of neonatal and adult mammalian heart regeneration by the miR-15 family. Proc Natl Acad Sci. 2013;110(1):187–192. doi: 10.1073/pnas.1208863110. Available at: http://dx.doi.org/10.1073/pnas.1208863110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Woo YJ, Panlilio CM, Cheng RK, Liao GP, Atluri P, Hsu VM, Cohen JE, Chaudhry HW. Therapeutic delivery of cyclin A2 induces myocardial regeneration and enhances cardiac function in ischemic heart failure. Circulation. 114:I-206–I-213. doi: 10.1161/CIRCULATIONAHA.105.000455. Available at: http://dx.doi.org/10.1161/CIRCULATIONAHA.105.000455. [DOI] [PubMed] [Google Scholar]
- [6].Eulalio A, Mano M, Ferro MD, Zentilin L, Sinagra G, Zacchigna S, Giacca M. Functional screening identifies miRNAs inducing cardiac regeneration. Nature. 2012;492(7429):376–381. doi: 10.1038/nature11739. Available at: http://dx.doi.org/10.1038/nature11739. [DOI] [PubMed] [Google Scholar]
- [7].Bolli R, Chugh AR, Damario D, Loughran JH, Stoddard MF, Ikram S, Beache GM, Wagner SG, Leri A, Hosoda T, Sanada F, Elmore JB, Goichberg P, Cappetta D, Solankhi NK, Fahsah I, Rokosh DG, Slaughter MS, Kajstura J, Anversa P. Cardiac stem cells in patients with ischaemic cardiomyopathy (SCIPIO): initial results of a randomised phase 1 trial. Lancet. 2011;378(9806):1847–1857. doi: 10.1016/S0140-6736(11)61590-0. Available at: http://dx.doi.org/10.1016/s0140-6736(11)61590-0. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- [8].Heusch G. SCIPIO brings new momentum to cardiac cell therapy. Lancet. 2011;378(9806):1827–1828. doi: 10.1016/S0140-6736(11)61648-6. Available at: http://dx.doi.org/10.1016/S0140-6736(11)61648-6. [DOI] [PubMed] [Google Scholar]
- [9].Takehara N, Nagata M, Ogata T, Nakamura T, Matoba S, Gojo S, Sawada T, Yaku H, Matsubara H. The ALCADIA (Autologous Human Cardiac-derived Stem Cell To Treat Ischemic Cardiomyopathy) trial. AHA 2012; LBCT-20032.
- [10]. Takehara N, Tsutsumi Y, Tateishi K, Ogata T, Tanaka H, Ueyama T, Takahashi T, Takamatsu T, Fukushima M, Komeda M, Yamagishi M, Yaku H, Tabata Y, Matsubara H, Oh H. Controlled delivery of basic fibroblast growth factor promotes human cardiosphere-derived cell engraftment to enhance cardiac repair for chronic myocardial infarction J Am Coll Cardiol 2008. 52 23 1858 1865 Available at: http://dx.doi.org/10.1016/j.jacc.2008.06.052 [DOI] [PubMed] [Google Scholar]
- [11].Malliaras K, Zhang Y, Seinfeld J, Galang G, Tseliou E, Cheng K, Sun B, Aminzadeh M, Marbán E. Cardiomyocyte proliferation and progenitor cell recruitment underlie therapeutic regeneration after myocardial infarction in the adult mouse heart. EMBO Mol Med. 2013;5(2):191–209. doi: 10.1002/emmm.201201737. Available at: http://dx.doi.org/10.1002/emmm.201201737. [DOI] [PMC free article] [PubMed] [Google Scholar]