Abstract
Purpose
Localized articular cartilage degeneration in the patellofemoral joint is a common but yet understudied condition in younger patients. The purpose of this paper was to determine whether there are significant differences in radiographic alignment between those with and without isolated lateral patellofemoral degeneration.
Methods
Subjects with isolated symptomatic lateral patellofemoral degeneration and control subjects with no radiographic degeneration participated in the study. Variables of interest included the Caton-Deschamps index, sulcus angle, lateral patellofemoral angle, Dejour classification of trochlear dysplasia, patella linear displacement and the tibial tubercle-trochlear groove distance.
Results
We found significant differences between the patellofemoral degeneration group versus control group, respectively, for the Caton-Deschamps index (1.12 ± 0.1 vs. 1.00 ± 0.1), lateral patellofemoral angle (10.6 ± 4.3 vs. 16.6 ± 5.5) and tibial tubercle-trochlear groove distance (16.6 ± 4.0 vs. 9.0 ± 4.3). However, we found no difference in the sulcus angle (141.2 ± 8.2 vs. 137.0 ± 6.0), patella linear displacement (3.7 ± 1.9 vs. 4.0 ± 1.7) or in the Dejour Classification.
Conclusion
It appears that isolated lateral patellofemoral degeneration is associated with specific radiographic indices. Even though the radiographic measures in patients with degeneration may not be considered pathologic, they are “high normal” and may represent a risk factor for the development of focal chondral degeneration in the lateral trochlea and patella.
Keywords: Patellofemoral, Patellofemoral osteoarthritis, Radiographic alignment, Knee
4. Introduction
Knee osteoarthritis (OA) is a leading cause of disability and chronic pain [12]. The two most common forms of knee OA are combined tibiofemoral and patellofemoral OA, followed by isolated patellofemoral OA (PFOA) [9]. The early development of patellofemoral joint degeneration (PFJD) in younger individuals can be especially difficult to treat and may result in the future development of PFOA. Surgical planning and rehabilitation of these individuals should account for potential differences in the joint structure that may increase shear and abnormal loading on the joint. However, little is still known about the potential differences in the alignment of the patellofemoral joint between those with and without early PFJD.
Although there have been few reports on the possible differences in the radiographic alignment in those with PFJD, emerging evidence from other studies in those with well-established PFOA suggest that there are several key parameters to focus on. For example, patella height, sulcus angle (SA) and the lateral patellofemoral angle (LPFA) have all been found to be related to progressively severe lateral PFOA [17, 20]. Additionally, the Q-angle as measured as the tibial tubercle-trochlear groove distance (TT-TG) has been found to be greater in those with PFOA [2]. To date, there have been few reports comparing PFJD to radiographic indices of patellofemoral alignment [5, 11, 14]. One study did find that individuals with lateral-sided PFJD had greater lateral patella tilt and displacement and no difference in patella height [14]. However, differences were found when symptomatic and non-symptomatic patients were combined. Additionally, no comparisons were made to the TT-TG or the SA, which have been important variables in those with PFOA. Lastly, Grelsamer et al. [11] reported on a group of 367 patients with established PFOA and found that 78% of these patients had a positive crossing sign indicating trochlear dysplasia.
Surgery and rehabilitation could have their greatest impact in addressing early PFJD [13]. However, effective interventions are currently limited by the lack of knowledge on the potential radiographic alignment differences in this group. Observational studies on PFOA have reported that lateral-sided degeneration is more common and progresses more rapidly [4]. Focusing on lateral degeneration may yield insights into a potentially unique cohort that is at risk for developing PFOA. Therefore, the purpose of this paper was to determine the differences in radiographic parameters between those with and without lateral PFJD. We hypothesized that those with early PFJD would have a greater patella height, SA, LPFA, TT-TG greater lateral linear patella displacement and more overt trochlea dysplasia as measured on Dejour’s classification of trochlear dysplasia than an age-matched control group.
5. Materials and Methods
Informed consent was approved by the institutional review board at the University of Kentucky and was obtained from all patients prior to participation in the study. To be included in the PFJD group, a clinical evaluation to determine symptomatic patellofemoral pain and early stage PFJD (measured using routine radiography and MRI of the knee) was first done. All patients who fitted these criteria then underwent a staging arthroscopy of the knee in preparation for a possible future surgical procedure. During this procedure, the degeneration and its location were confirmed. Only grade 3 and 4 degeneration in the lateral patellofemoral joint as determined by the International Cartilage Research Society (ICRS) scale were included. The same orthopedic surgeon (CL) evaluated all of the patients for inclusion into the study.
An age-matched control cohort was chosen from a population of patients undergoing anterior cruciate ligament (ACL) reconstruction. The absence of any PFJD was confirmed with routine radiography and MRI. During the arthroscopic ACL reconstruction, the integrity of the patellofemoral joint was verified by direct inspection. Only patients with patellofemoral joints showing an ICRS rating of 0 in all three surfaces of the trochlea as well as all six surfaces of the patella on the ICRS scale were included in the cohort.
Patients with generalized OA and multiple defects in other compartments of the knee joint were excluded from this study. The determinations of any osteophytes or joint space narrowing was measured by standard MRI and plain radiography of the knee (weight bearing A/P in extension, weight bearing P/A at 45° flexion, Merchant view at 30° knee flexion and a weight bearing lateral). Additionally, subjects in either group could not report a history of previous patellar dislocation or instability.
Radiographic parameters
All patients underwent MRI scanning and plain radiography. Plain radiography included a full weight bearing A/P of the knee in full extension, a flexion weight bearing p/a view in 45° of flexion, a merchant view at 30° of knee flexion and a perfect lateral radiograph of the knee at 30° of flexion. Radiographic parameters measured were the Caton-Deschamps (CD) index, SA, the LPFA and the Dejour classification for trochlear dysplasia. The same orthopedic surgeon (SD) made all of the measurements of the radiographic indices.
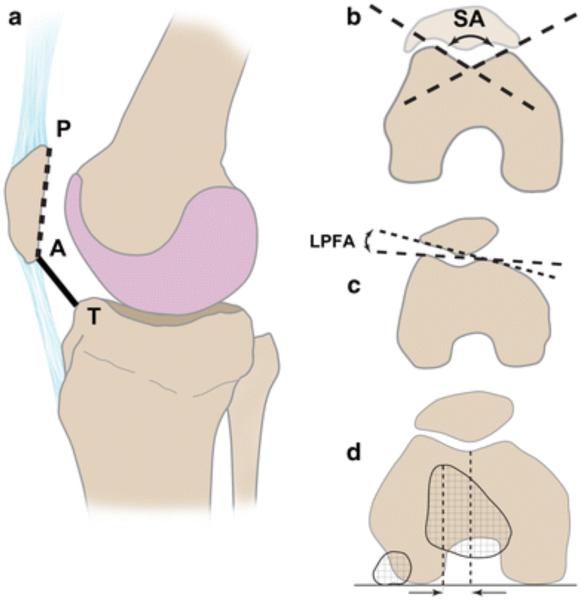
The CD index was calculated from the lateral radiograph. The CD index was determined by first drawing a line along the length of the articular surface of the patella (AP). Then, a second line is drawn between the most distal aspect of the patella to the most anterior tibial articulating surface (AT) (Fig. 1a). The CD was determined from the following equation CD = AT/AP [8].
Fig. 1.
Diagrams of the primary radiographic features measured. a The Caton-Deschamps index, b sulcus angle, clateral patellofemoral angle and d tibial tubercle-trochlear groove distance
To assess trochlea morphology, Dejour’s classification of trochlear dysplasia was used. This classification system has been previously described in detail elsewhere and is briefly reviewed here [7, 24, 25]. The classification consists of four grades (A–D) of increasing dysplasia, grade A equals a shallow trochlea, but its morphology is preserved, grade B equals a flat or convex trochlea possibly with a supratrochlear spur, grade C has asymmetric trochlear facets with a double contour and grade D has an oversized lateral spur of the convex medial trochlear facet [25]. Lastly, to better understand the relationship between the patella displacement and the trochlea, we also calculated the axial linear displacement of the patella (PLD) as described previously by Urch et al. [26].
The SA and LPFA were calculated based upon the Merchant view of the patellofemoral joint [2]. The SA was determined as the angle between two lines, one drawn along the lateral aspect of the trochlea and one along the medial aspect of the trochlea (Fig. 1b). The LPFA was determined by the angle formed from the intersection of two lines. The first is drawn from the medial to lateral femoral condyle. The second is drawn along the lateral boney margin of the patella (Fig. 1c).
The TT-TG measurement was taken off of axial MRI images. The MRI scan was performed in supine position with the knee near full extension. Routine sagittal, coronal and axial, T1 and T2 sequencing was performed. TT-TG measurements were performed on the axial MRI sections according to the technique described by Schoettle et al. [22].
Statistical analysis
Group means and standard deviations were calculated. A two-tailed independent t-test was used to determine group differences. To further understand the magnitude of the differences between groups, effects sizes were calculated. The Dejour classification for trochlear dysplasia was described descriptively between groups.
6. Results
A total of 28 individuals participated in the study (14 PFJD: 14 controls). Both the PFJD group and controls group were similar in age (PFJD 32 ± 8.8: controls 33 ± 10 years old) and gender (PFJD 6M, 8F: controls, 6M, 8F). The results are summarized in table one. Significant differences were found in the CD, LPFA and the TT-TG (Table 1). No significant differences were found in the SA, but it was associated with a moderate to large effect size (Table 1). There was also no significant difference in the PLD that was associated with a small effect size. All subjects in the control group had a grade A trochlear index, as did all, but one subject (grade B) in the PFJD group.
Table 1.
Comparison between the mean and (standard deviation) between the PFJD and control groups for the Caton-Deschamps index (CD), sulcus angle (SA), lateral patellofemoral angle (LPFA), tibial tubericle-trochlear groove distance (TT-TG) and patella linear displacement (PLD)
| PFJD | Control | P value | Effect size | |
|---|---|---|---|---|
| CD | 1.12 (0.1) | 1.00 (0.1) | 0.01 | 0.96 |
| SA | 141.2 (8.2) | 137.0 (6.0) | n.s. | 0.78 |
| LPFA | 10.6 (4.3) | 16.6 (5.5) | 0.02 | 0.80 |
| TT-TG | 16.6 (4.0) | 9.0 (4.3) | 0.00 | 1.8 |
| PLD | 3.7 (1.9) | 4.0 (1.7) | n.s. | 0.16 |
7. Discussion
The most important finding of the present study was the statistically significant differences in the CD, LPFA and TT-TG between the PFJD and control group. However, we found no difference in the SA or Dejour classification. Collectively, these differences provide important insights into how the alignment of the patellofemoral joint may place greater stress on the lateral aspect of the patellofemoral joint and could be important features in the future development of PFOA. The PFJD group had a significantly higher riding patella than the control group. This is in contrast to the findings of Harilainen et al. [14] who reported no difference in the patella height. However, we are unable to make a direct comparison between studies as the grade of the degeneration or how many of those with anterior knee pain also had a cartilage defect was not reported by Harilainen et al. [14]. A higher CD index suggests that the patella does not engage the trochlea until deeper degrees of knee flexion, resulting in greater shear across the patella at low flexion angles. Also, a longer patellar tendon decreases the mechanical advantage of the patella and may lead to greater compression in deeper knee flexion angles [16].
A larger SA may result in greater patellar mobility in early knee flexion as there is less osseous structure to guide the patella [17]. In the current study, we did not find a statistical difference between the groups, although the measure was associated with a large effect size. The findings in the current study are in contrast with Ali and colleagues, who reported that those with severe patellofemoral cartilage degeneration had a greater SA [1]. Likewise, a recent study reported that a larger SA was associated with increasingly severe symptomatic PFOA [17]. However, both of these studies focused on established PFOA, whereas the current study was focused on the early development of degeneration. It is plausible that as the condition worsens, joint morphology will also change.
The smaller value of LPFA in the PFJD group indicates that the patella was more laterally tilted. Greater lateral tilt of the patella may increase the compression and shear on the cartilage. Indeed, Kalichman et al. found that lower values of the LPFA were associated with lateral cartilage loss in patients with PFOA [16,17]. In contrast to these findings, Harilainen et al. [14] found no difference in the structure of the patellofemoral joint when comparing those who had patellofemoral pain to a group that had a meniscus rupture. However, they did find independent of patellofemoral pain, a relationship between the location of patellar degeneration and patellar translation and tilt [14]. These results suggest that the LPFA maybe an important variable to consider in assessing those with a PFJD.
To date, there is limited evidence on the role of the TT-TG in the development of PFJD. In the current study, we found a significantly larger TT-TG in the PFJD group. A greater TT-TG would increase the bias in the force vector from contraction of the quadriceps to the lateral aspect of the patellofemoral joint. The TT-TG of the PFJD group was also within the range that has been previously reported in those with symptomatic patellar instability [18, 22]. By contrast, it is also interesting that our control group showed a lower TT-TG (average: 9 mm), which was reported normal in the literature [22]. Perhaps, a marginally elevated TT-TG in fact may represent a subtle non-symptomatic instability that could increase the shear across the patellofemoral joint. However, this hypothesis is speculative at this point, and the future prospective studies are needed to consider its role and mechanism in the initial degeneration of the patellofemoral joint.
An important radiographic measure for the patellofemoral joint in patients with instability is the Dejour classification of trochlear dysplasia. Dejour et al. [8] could show that 96% of patients who had a documented patella dislocation had a measure of trochlear dysplasia, whereas the normal population only presented with this finding in 3%. In our study, however, there was only one subject in the defect group who had a slightly pathologically formed trochlea and scored a Dejour Type B showing an asymmetric crossing of the outline of the trochlear floor or so-called “recentring beak”. Two factors may play a role for this finding. First, patients in the current study did not have clinically symptomatic patella instability. Second, the study was only open to those who have established but discreet chondral defects in the lateral trochlea and patella. An interesting observation may be that young patients with severe trochlear dysplasia and recurrent dislocation rarely have trochlear cartilage lesions that is one reason why trochleoplasty as originally described by Masse, but modified and popularized by Henry Dejour or in the technique of Bereiter or Schoettle and Bereiter can be performed [3, 23]. These techniques cannot be performed if there is a significant cartilage loss or PFOA in the trochlea. We, therefore, may have had a different patient population in our study, which could explain the normal findings for trochlear dysplasia.
Unlike patella tilt, there was no difference in patella displacement between groups. Perhaps, subtle changes in patella displacement are not as evident in the early stages of PFJD. Indeed, a more laterally displaced patella has been associated with greater severity of PFOA [17]. Also, detecting early changes in displacement may be difficult due to the limitations in current techniques of measuring patella displacement. While these procedures are reliable and have the ability to detect large differences between groups, they are not well established in detecting more subtle changes in displacement [27]. The development of new techniques that are more sensitive to changes in displacement is needed and is the focus of future work.
Limitations of the study include a relatively small sample size. However, the variables were normally distributed and associated with a large effect size. Another limitation is the cross-sectional design of the study, which does not allow us to say that these variables caused the degeneration. Future prospective longitudinal studies are needed to determine whether these variables are related to the initial development of patellofemoral degeneration. Also, long leg alignment radiographs were not obtained on all of our patients to determine the influence of the axial alignment on the radiographic parameters. Nor were rotational MRI or CT scans obtained on all of these patients and were, therefore, not included in this analysis. However, the radiographic parameters measured are likely a composite result of the knee joint anatomy. Therefore, if any of the measured factors is affected by axial alignment, it will still be valid as a screening tool although it may not indicate the reason for the malalignment. We also performed no test-retest reliability for this study. A single experienced examiner, though, took all measurements, and any error in the measurements would have been randomly distributed. An assessment of the accuracy of these measurements to a gold standard was beyond the scope of the current paper, but they do represent measurements that clinicians can readily incorporate into their current practice. Continued research is needed to further refine the measurement accuracy of patellofemoral radiographic indices. Finally, we focused only on lateral patellofemoral degeneration. Different degeneration locations (medial, central) maybe associated with a unique set of radiographic parameters.
This study has several clinical implications. For instance, it maybe necessary to analyze patients with lateral-sided patellofemoral pain regarding a potential subtle-instability as indicated by high normal patellofemoral radiographic parameters. These findings also support the current practice to correct high normal or just abnormally high TT-TG values as suggested by other authors in patients undergoing cartilage repair procedures in the patellofemoral joint [10, 15, 21]. Correction of clinically subtle patellofemoral instability may need to be considered more carefully in patients with high normal TT-TG. These findings may also indicate that the normal values documented in the literature for TT-TG and Caton ratio may be too high. These data also add additional evidence to the importance of assessing the radiographic alignment of the patellofemoral joint and should be considered in the pre-surgical planning in a range of cases where there is degeneration of the lateral patellofemoral joint, including total knee replacements, and other surgeries such as partial lateral patellar facetectomy and autologous chondrocyte implantation [5, 19, 20]. Lastly, consideration should be given to the possible utility of taping and bracing to alter alignment and reduce pain in select patients with early lateral-sided patellofemoral degeneration and high patellar tilt [6]. This may provide an inexpensive means of pain relief as a more permanent long-term correction of the degeneration and alignment is sought.
8. Conclusion
In conclusion subjects with lateral PFJD had significant differences in the IS, LPFA and TT-TG as compared to an age-matched control group. There was no difference in the SA and PLD between groups. These results suggest that there maybe a unique radiographic presentation within a focused group of individuals with early lateral PFJD. Alterations in the alignment of the patellofemoral joint likely increase the compression and shear on the lateral aspect of the joint contributing to the formation of the cartilage degeneration.
Footnotes
2. Level of evidence
III.
9. References
- 1.Ali SA, Helmer R, Terk MR. Analysis of the patellofemoral region on MRI: association of abnormal trochlear morphology with severe cartilage defects. AJR Am J Roentgenol. 2010;194(3):721–727. doi: 10.2214/AJR.09.3008. [DOI] [PubMed] [Google Scholar]
- 2.Beaconsfield T, Pintore E, Maffulli N, Petri GJ. Radiological measurements in patellofemoral disorders. A review. Clin Orthop Relat Res. 1994;308:18–28. [PubMed] [Google Scholar]
- 3.Bereiter HGE. Die trochleaplastik als chirurgische Therapie der rezidivierenden Patellaluxation bei Trochleadysplasie des Femurs. Arthroskopie. 1994;7:281–286. [Google Scholar]
- 4.Cahue S, Dunlop D, Hayes K, Song J, Torres L, Sharma L. Varus-valgus alignment in the progression of patellofemoral osteoarthritis. Arthritis Rheum. 2004;50(7):2184–2190. doi: 10.1002/art.20348. [DOI] [PubMed] [Google Scholar]
- 5.Chia SL, Merican AM, Devadasan B, Strachan RK, Amis AA. Radiographic features predictive of patellar maltracking during total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2009;17(10):1217–1224. doi: 10.1007/s00167-009-0832-y. [DOI] [PubMed] [Google Scholar]
- 6.Crossley KM, Marino GP, Macilquham MD, Schache AG, Hinman RS. Can patellar tape reduce the patellar malalignment and pain associated with patellofemoral osteoarthritis? Arthritis Care Res. 2009;61(12):1719–1725. doi: 10.1002/art.24872. [DOI] [PubMed] [Google Scholar]
- 7.Dejour D, Le Coultre B. Osteotomies in patello-femoral instabilities. Sports Med Arthrosc. 2007;15(1):39–46. doi: 10.1097/JSA.0b013e31803035ae. [DOI] [PubMed] [Google Scholar]
- 8.Dejour H, Walch G, Nove-Josserand L, Guier C. Factors of patellar instability: an anatomic radiographic study. Knee Surg Sports Traumatol Arthrosc. 1994;2(1):19–26. doi: 10.1007/BF01552649. [DOI] [PubMed] [Google Scholar]
- 9.Duncan RC, Hay EM, Saklatvala J, Croft PR. Prevalence of radiographic osteoarthritis—it all depends on your point of view. Rheumatology. 2006;45(6):757–760. doi: 10.1093/rheumatology/kei270. [DOI] [PubMed] [Google Scholar]
- 10.Gomoll AH, Minas T, Farr J, Cole BJ. Treatment of chondral defects in the patellofemoral joint. J Knee Surg. 2006;19(4):285–295. doi: 10.1055/s-0030-1248121. [DOI] [PubMed] [Google Scholar]
- 11.Grelsamer RP, Dejour D, Gould J. The pathophysiology of patellofemoral arthritis. Orthop Clin North Am. 2008;39(3):269–274. doi: 10.1016/j.ocl.2008.03.001. [DOI] [PubMed] [Google Scholar]
- 12.Guccione AA, Felson DT, Anderson JJ, Anthony JM, Zhang Y, Wilson PW, Kelly-Hayes M, Wolf PA, Kreger BE, Kannel WB. The effects of specific medical conditions on the functional limitations of elders in the Framingham Study. Am J Public Health. 1994;84(3):351–358. doi: 10.2105/ajph.84.3.351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Guney A, Bilal O, Oner M, Halici M, Turk Y, Tuncel M. Short- and mid-term results of plica excision in patients with mediopatellar plica and associated cartilage degeneration. Knee Surg Sports Traumatol Arthrosc. 2010;18(11):1526–1531. doi: 10.1007/s00167-010-1125-1. [DOI] [PubMed] [Google Scholar]
- 14.Harilainen A, Lindroos M, Sandelin J, Tallroth K, Kujala UM. Patellofemoral relationships and cartilage breakdown. Knee Surg Sports Traumatol Arthrosc. 2005;13(2):142–144. doi: 10.1007/s00167-003-0467-3. [DOI] [PubMed] [Google Scholar]
- 15.Henderson IJ, Lavigne P. Periosteal autologous chondrocyte implantation for patellar chondral defect in patients with normal and abnormal patellar tracking. Knee. 2006;13(4):274–279. doi: 10.1016/j.knee.2006.04.006. [DOI] [PubMed] [Google Scholar]
- 16.Kalichman L, Zhang Y, Niu J, Goggins J, Gale D, Felson DT, Hunter D. The association between patellar alignment and patellofemoral joint osteoarthritis features—an MRI study. Rheumatology (Oxford) 2007;46(8):1303–1308. doi: 10.1093/rheumatology/kem095. [DOI] [PubMed] [Google Scholar]
- 17.Kalichman L, Zhang Y, Niu J, Goggins J, Gale D, Zhu Y, Felson D, Hunter D. The association between patellar alignment on magnetic resonance imaging and radiographic manifestations of knee osteoarthritis. Arthritis Res Ther. 2007;9(2):R26. doi: 10.1186/ar2138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Panni AS, Cerciello S, Maffulli N, Di Cesare M, Servien E, Neyret P. Patellar shape can be a predisposing factor in patellar instability. Knee Surg Sports Traumatol Arthrosc. 2011;19(4):663–670. doi: 10.1007/s00167-010-1329-4. [DOI] [PubMed] [Google Scholar]
- 19.Pascual-Garrido C, Slabaugh MA, L’Heureux DR, Friel NA, Cole BJ. Recommendations and treatment outcomes for patellofemoral articular cartilage defects with autologous chondrocyte implantation: prospective evaluation at average 4-year follow-up. Am J Sports Med. 2009;37(Suppl 1):33S–41S. doi: 10.1177/0363546509349605. [DOI] [PubMed] [Google Scholar]
- 20.Paulos LE, O’Connor DL, Karistinos A. Partial lateral patellar facetectomy for treatment of arthritis due to lateral patellar compression syndrome. Arthroscopy. 2008;24(5):547–553. doi: 10.1016/j.arthro.2007.12.004. [DOI] [PubMed] [Google Scholar]
- 21.Rue JP, Colton A, Zare SM, Shewman E, Farr J, Bach BR, Jr, Cole BJ. Trochlear contact pressures after straight anteriorization of the tibial tuberosity. Am J Sports Med. 2008;36(10):1953–1959. doi: 10.1177/0363546508317125. [DOI] [PubMed] [Google Scholar]
- 22.Schoettle PB, Zanetti M, Seifert B, Pfirrmann CW, Fucentese SF, Romero J. The tibial tuberosity-trochlear groove distance; a comparative study between CT and MRI scanning. Knee. 2006;13(1):26–31. doi: 10.1016/j.knee.2005.06.003. [DOI] [PubMed] [Google Scholar]
- 23.Schottle PB, Fucentese SF, Pfirrmann C, Bereiter H, Romero J. Trochleaplasty for patellar instability due to trochlear dysplasia: a minimum 2-year clinical and radiological follow-up of 19 knees. Acta Orthop. 2005;76(5):693–698. doi: 10.1080/17453670510041781. [DOI] [PubMed] [Google Scholar]
- 24.Tavernier T, Dejour D. Knee imaging: what is the best modality. J Radiol. 2001;82(3 Pt 2):387–405. 407–488. [PubMed] [Google Scholar]
- 25.Tecklenburg K, Dejour D, Hoser C, Fink C. Bony and cartilaginous anatomy of the patellofemoral joint. Knee Surg Sports Traumatol Arthrosc. 2006;14(3):235–240. doi: 10.1007/s00167-005-0683-0. [DOI] [PubMed] [Google Scholar]
- 26.Urch SE, Tritle BA, Shelbourne KD, Gray T. Axial linear patellar displacement: a new measurement of patellofemoral congruence. Am J Sports Med. 2009;37(5):970–973. doi: 10.1177/0363546508328596. [DOI] [PubMed] [Google Scholar]
- 27.Wilson T. The measurement of patellar alignment in patellofemoral pain syndrome: are we confusing assumptions with evidence? J Orthop Sports Phys Ther. 2007;37(6):330–341. doi: 10.2519/jospt.2007.2281. [DOI] [PubMed] [Google Scholar]