Abstract
We present the introduction of the surgical robot for pelvic lymphadenectomy for skin cancer through a cross-specialty collaboration. In this prospective series, we include the first report of cases undergoing robot-assisted pelvic lymph node dissection for Merkel cell carcinoma and melanoma in the recognised scientific literature.
Keywords: Melanoma, Squamous cell carcinoma, Merkel cell carcinoma, Robotics, Minimally invasive surgical procedures, Lymph node excision
Pelvic lymphadenectomy is advocated, sometimes prophylactically, in international guidelines for both melanoma and squamous cell carcinoma (SCC). 1–3 Laparoscopic techniques have been applied to minimise the significant morbidity associated with open pelvic dissection. 4–6 Laparoscopic lymph node dissection in skin cancer has been limited by concerns including the ability to perform meticulous node clearance around major vessels, port site implantation and working in previously irradiated tissue planes. The enhanced dexterity and, particularly, the magnified three-dimensional vision afforded by the da Vinci® robotic system (Intuitive Surgical, Sunnyvale, CA, US) addresses several of these issues. We report our first four cases of robot-assisted pelvic lymph node dissection (RAPLND) for skin malignancy, including the first for Merkel cell carcinoma (MCC) reported worldwide, managed in a multidisciplinary setting from a tertiary referral centre using a four-arm da Vinci® Si (Fig 1).
Figure 1.
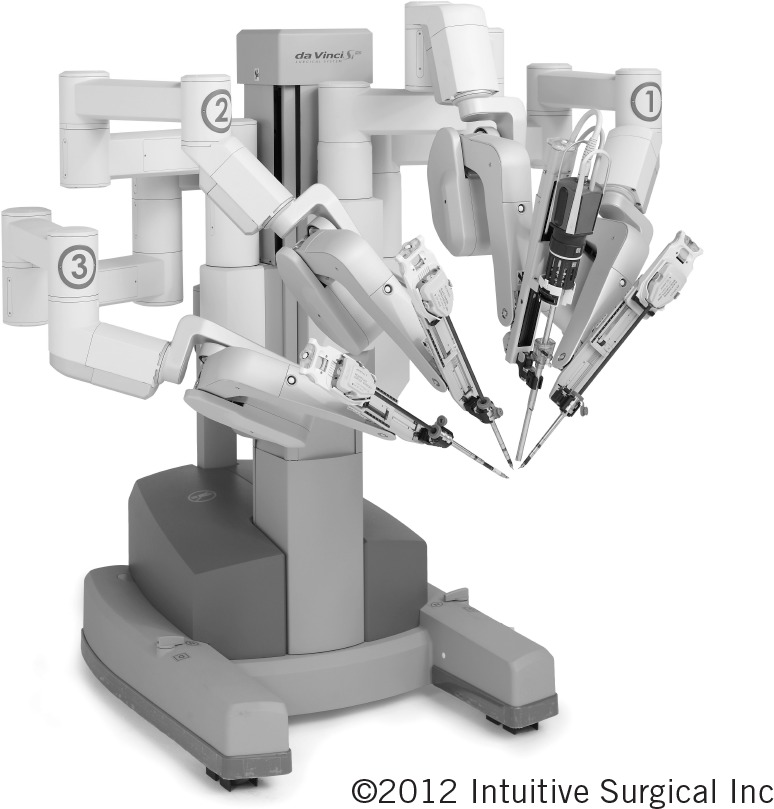
The four-arm da Vinci® Si
Methods
Data were collected prospectively for patients undergoing RAPLND for skin cancer at the Guy’s and St Thomas’ NHS Foundation Trust. These included age, indication, disease pathology, site of primary tumour, previous treatment, comorbidities, operative time, complications, length of hospital stay, the histopathologically reported number of lymph nodes and nodal disease involvement.
Results
All operations were performed at Guy’s Hospital and all patients were female. The cases are summarised in Table 1. The first patient was offered a prophylactic pelvic clearance after her inguinal lymphadenectomy (for a stage IIIB melanoma arising from her thigh) had shown two of eight nodes with extracapsular spread. This was complicated by seroma formation, pain, cellulitis and lymphoedema. She was offered RAPLND after refusing an open approach due to the morbidity associated with the latter procedure. Ipsilateral RAPLND was carried out without complications. The patient was fit for discharge 24 hours postoperatively. The genitofemoral and obturator nerves formed the cranial and inferior borders of the dissection. All tissue medial and lateral to the external iliac vessels was cleared. All nodes retrieved were clear of metastases. She remains disease free after 15 months of follow-up.
Table 1.
Summary of the first four reported cases to undergo robot-assisted pelvic lymph node dissection for skin cancer
| Patient 1 | Patient 2 | Patient 3 | Patient 4 | |
|---|---|---|---|---|
| Age | 69 years | 86 years | 43 years | 74 years |
| Pathology | Melanoma | Melanoma | SCC | MCC |
| Primary site | Right thigh | Right ankle | Unknown | Right leg |
| Time since inguinal lymph node clearance | 7 months | Not required | 5 months | 5 months |
| Co-morbidities | Inguinal dissection complicated by pain, infection, seroma and dehiscence | Folate deficiency and raised APTT, hypertension, frail | Renal transplant, myaesthenia gravis, non-melanoma skin cancers, cervical carcinoma | Diabetes mellitus, non-melanoma skin cancers |
| Indication | Prophylactic (2 of 8 inguinal lymph nodes with extracapsular spread) | Enlarged pelvic lymph node confirmed on PET-CT | Extensive pelvic nodal metastases on PET-CT | Enlarged pelvic lymph node confirmed on PET-CT |
| Operative time | 90 min | 90 min | 150 min | 90 min |
| Complications | Pre and postoperative lymphoedema | Ileus, constipation | Pre and postoperative lymphoedema, died 4 months later | None |
| Pelvic histopathology | 0 of 6 nodes | 1 of 5 nodes (extracapsular spread) | Mass of metastatic SCC | 1 of 8 nodes (extracapsular spread) |
| Length of hospital stay | 4 days* | 17 days | 8 days | 2 days |
SCC = squamous cell carcinoma; MCC = Merkel cell carcinoma; APTT = activated partial thromboplastin time; PET-CT = positron emission tomography - computed tomography
Medically fit to be discharged at 24 hours but patient declined as she was the first patient to undergo robotic surgery for skin cancer
The second patient was an 86-year-old woman, the oldest we know of to have a robotic procedure, presenting with a stage IIIC melanoma (three in-transit metastases and a pelvic node detected on positron emission tomography - computed tomography [PET-CT]). Minimally invasive surgery was indicated due to multiple co-morbidities including a clotting deficiency. RAPLND and concurrent right ankle metastasis excision were carried out without immediate complications. Technical modification included a ‘no touch’ technique of the golf ball sized melanoma deposit. The postoperative course was complicated by constipation and ileus but no wound complications. The patient remains disease free, independent and self-caring at home after 12 months of follow-up.
The third patient was a 43-year-old woman with a history of myaesthenia gravis, a renal transplant, multiple cutaneous SCCs and a vulval carcinoma treated previously with radiotherapy, presenting with groin swelling. A prior inguinal lymphadenectomy had been performed for a metastatic SCC with extracapsular spread. Follow-up PET-CT detected an 8cm mass adherent to the external iliac vessels in close proximity to the extraperitoneal renal transplant. RAPLND was carried out without complications. Technical modification included proximal control of the external iliac artery and vein with vessel loops enabling dissection of the lymph node mass with clear surgical margins. Sharp dissection was used in the previously irradiated field. A single venotomy was closed with a 5/0 Prolene® suture (Ethicon, Somerville, NJ, US). The patient’s total intraoperative blood loss was 50ml. She succumbed to her disease four months postoperatively.
The fourth patient was a 74-year-old diabetic woman who underwent a right inguinal lymphadenectomy for a metastatic SCC. PET-CT detected a positive pelvic lymph node. Ipsilateral RAPLND was performed without complications. One of eight nodes retrieved showed MCC, a rare cancer that shows a high preponderance to lymphatic spread. Metastases should be excised where possible and radiotherapy considered. 7 The patient remains well 11 months postoperatively.
All cases were completed robotically. Associated morbidity was low, with no complications of wound healing. In the case of Patient 3, open surgery would have been hazardous in a previously irradiated field containing a transplanted kidney.
Discussion
The morbidity of open pelvic lymph node dissection has made this treatment modality unpopular. However, several groups have reported a 5-year survival rate of up to 47% and a 10-year survival rate of 20% in patients in patients undergoing combined inguinal and pelvic dissection. 4,8 Lymphatic studies demonstrate trunk and thigh sentinel node drainage to lie in the pelvis in a significant proportion of patients. 9 RAPLND offers the potential to minimise morbidity for both prophylactic and therapeutic indications for a pelvic lymphadenectomy. We know from our prostate patients that robotic surgery offers rapid patient recovery, mobilisation and return to normal activities of daily living. Surgery can be conducted safely in the previously operated/irradiated pelvis. Modern tissue retrieval systems using disposable endoscopic bags eradicate the possibility of port site seeding.
Three out of four patients in our series deferred surgery due to concerns with pain and prolonged recovery following open surgery. Once a suitable alternative technique was made available to them, they were able to be treated as per guidelines by both a skin surgeon and an experienced urological robotic team.
The particular technical demands of the robot control reward operator experience. The collaboration between skin cancer and experienced robot urology surgeons enables us to offer RAPLND to patients for whom the potential morbidity of an open operation outweighs the likely benefit of a pelvic lymphadenectomy. The cost and multidisciplinary skills required to make this technique available will, of course, restrict its use to mainly tertiary subspecialty referral units.
Conclusions
This prospective series of patients with skin malignancy undergoing RAPLND demonstrates the potential of the technique in minimising the morbidity of a pelvic lymphadenectomy and the importance of cross-specialty collaboration in bringing technological advances to patients. We are not advocating that this becomes a standard approach in all units. This combined approach came about due to restrictions on which surgeons can operate on skin cancer patients. Guidance from the National Institute for Health and Clinical Excellence 10 had been adhered to in these cases and the patients benefited from the extra choice. High patient satisfaction with the rapidity of recuperation following RAPLND has encouraged our unit to develop and offer this modality to patients deemed appropriate from our specialty skin cancer multidisciplinary meetings.
Acknowledgement
The material in this paper was presented at the winter meeting of the British Association of Plastic, Reconstructive and Aesthetic Surgeons held in London, 2011.
References
- 1.Marsden JR, Newton-Bishop JA, Burrows Let al Revised UK guidelines for the management of cutaneous melanoma 2010. J Plast Reconstr Aesthet Surg 2010; 63: 1,401–1,419 [DOI] [PubMed] [Google Scholar]
- 2.Australian Cancer Network Melanoma Guidelines Revision Working Party. Clinical Practice Guidelines for the Management of Melanoma in Australia and New Zealand. Sydney: Cancer Council Australia and Australian Cancer Network; Wellington: New Zealand Guidelines Group; 2008 [Google Scholar]
- 3.Motley RJ, Preston PW, Lawrence CM. Multi-professional Guidelines for the Management of the Patient with Primary Cutaneous Squamous Cell Carcinoma. London: British Association of Dermatologists; 2009 [Google Scholar]
- 4.Hughes TM, Thomas JM. Combined inguinal and pelvic lymph node dissection for stage III melanoma. Br J Surg 1999; 86; 1,493–1,498 [DOI] [PubMed] [Google Scholar]
- 5.Ali-Khan AS, Crundwell M, Stone C. Inguinal lymphadenectomy combined with staging endoscopic pelvic node sampling for stage III melanoma. J Plast Reconstr Aesthet Surg 2009; 62: 1,063–1,067 [DOI] [PubMed] [Google Scholar]
- 6.Picciotto F, Volpi E, Zaccagna A, Siatis D. Transperitoneal laparoscopical iliac lymphadenectomy for treatment of malignant melanoma. Surg Endosc 2003; 17: 1,536–1,540 [DOI] [PubMed] [Google Scholar]
- 7.Ruan JH, Reeves M. A Merkel cell carcinoma treatment algorithm. Arch Surg 2009; 144: 582–585 [DOI] [PubMed] [Google Scholar]
- 8.Strobbe LJ, Jonk A, Hart AAet al Positive iliac and obturator nodes in melanoma: survival and prognostic factors. Ann Surg Oncol 1999; 6: 255–262 [DOI] [PubMed] [Google Scholar]
- 9.Kaoutzanis C, Barabás A, Allan Ret al When should pelvic sentinel lymph nodes be harvested in patients with malignant melanoma? J Plast Reconstr Aesthet Surg 2012; 65; 85–90 [DOI] [PubMed] [Google Scholar]
- 10.National Institute for Health and Clinical Excellence. Improving Outcomes for People with Skin Tumours including Melanoma. London: NICE; 2006 [PubMed] [Google Scholar]


