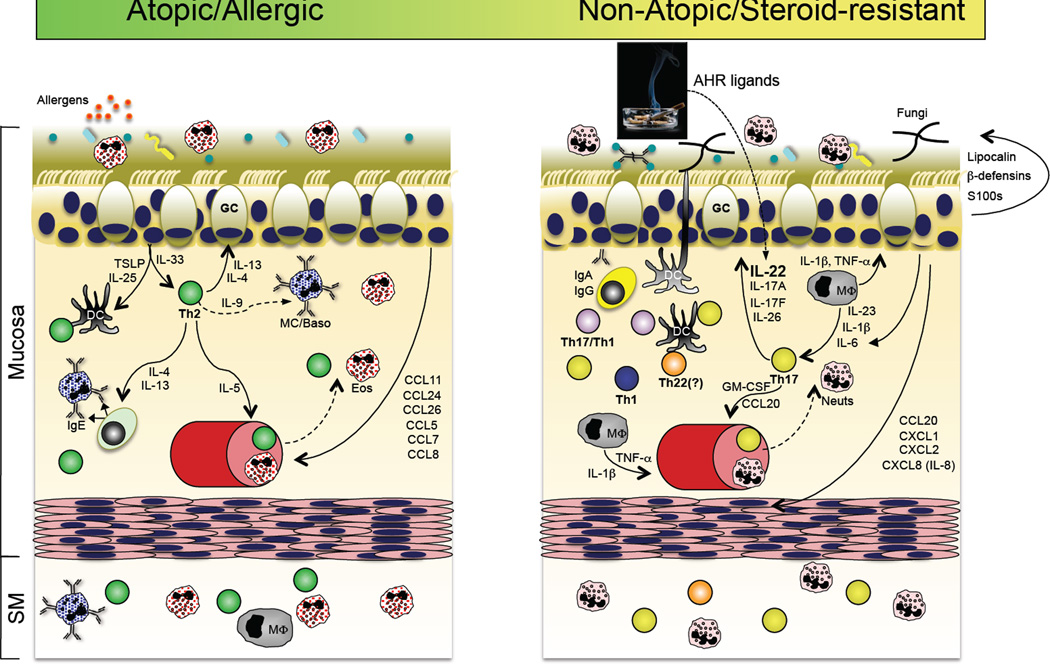
Figure 6.
Mechanisms by which Th17 and Th22 pathways contribute to psoriasis and atopic dermatitis. Psoriasis (left panel) and atopic dermatitis (right panel) are chronic inflammatory diseases of skin with distinct immunopathogeneses. In psoriasis, hyperproliferation and impaired differentiation of keratinocytes in the epidermis is caused by an inflammatory cascade primarily mediated by the signaling of cytokines produced by cells of the Th17 pathway within the dermis. IL-17A signaling into keratinocytes, in synergy with IL-22 and TNFα and potentially IFNγ, induces the production of a variety of pro-inflammatory proteins (AMPS, chemokines and cytokines), which results in a heightened immune state and the further recruitment and activation of immune cells that maintain chronic inflammation. IL-17A and IL-22 also induce the production of IL-20 and IL-24 by keratinocytes, which, with IL-22, induce keratinocyte hyperproliferation and hyperplasia, or acanthosis, that is a hallmark of the psoriatic pathology. Atopic dermatitis (AD) is distinguished by both defects in the terminal differentiation of the epidermis and the pattern of sustained inflammation (right panel). In AD, the barrier function of the cornified layer of the epidermis can be defective, resulting in increased sensitization to environmental antigens that primes a dysregulated Th2 response. Th2 cytokines promote the generation of antigen-specific IgE and the recruitment/expansion of mast cells, basophils and eosinophils. Similar to, yet distinct from, psoriasis, a variety of antimicrobial peptides (AMPs), cytokines and chemokines are up-regulated in AD, which contribute to maintenance of the underlying inflammation. It has been recently demonstrated that Th22 (and Tc22 cells; not shown) are prevalent in AD lesions, which contribute IL-22 that induces the epidermal hyperplasia that is characteristic of AD lesions. The relative contributions of Th2 and Th22 cells to pathogenesis has yet to be well explored, and there might well be a spectrum of disease in individual patients.