Abstract
Purpose
Our aim was to test the validity of using the bare spot method to quantify glenoid bone loss arthroscopically in patients with shoulder instability.
Methods
Twenty-seven patients with no evidence of instability (18 males, nine females; mean age 59.1 years) were evaluated arthroscopically to assess whether the bare spot is consistently located at the center of the inferior glenoid. Another 40 patients with glenohumeral anterior instability who underwent shoulder arthroscopy (30 males, ten females; mean age 25.9 years) were evaluated for glenoid bone loss with preoperative three-dimensional computed tomography (3D-CT) and arthroscopic examination. In patients without instability, the distances from the bare spot of the inferior glenoid to the anterior (Da) and posterior (Dp) glenoid rim were measured arthroscopically. In patients with instability, we compared the percentage glenoid bone loss calculated using CT versus arthroscopic measurements.
Results
Among patients without instability, the bare spot could not be identified in three of 27 patients. Da (9.5±1.2 mm) was smaller than Dp (10.1±1.5 mm), but it was not significantly different. However, only 55% of glenoids showed less than 1 mm of difference between Da and Dp, and 18% showed more than 2 mm difference in length. The bare spot could not be identified in five of 40 patients with instability. Pearson’s correlation coefficient showed significant (P<0.001) and strong (R2=0.63) correlation in percentage glenoid bone loss between the 3D-CT and arthroscopy method measurements. However, in ten shoulders (29%), the difference in percentage glenoid bone loss between 3D-CT and arthroscopic measurements was greater than 5%.
Conclusion
The bare spot was not consistently located at the center of the inferior glenoid, and the arthroscopic measurement of glenoid bone loss using the bare spot as a landmark was inaccurate in some patients with anterior glenohumeral instability.
Level of evidence
Level II, prospective comparative study.
Keywords: shoulder instability, glenoid defect, arthroscopy, Bankart repair, 3D-CT, bone graft, shoulder dislocation
Introduction
The degree of glenoid bone loss has a significant impact on the outcome of arthroscopic Bankart repair.1–9 Several cadaveric studies have shown that an osseous defect with a width approximately 20% of the glenoid length or 25% of the glenoid width remains unstable even after Bankart repair, and bone grafting is recommended in such cases.10,11 Burkhart and De Beer12 reported that patients with significant glenoid bone loss (more than 25%) had a high recurrence rate (67%) after arthroscopic Bankart repair, whereas patients without significant bone loss had a low recurrence rate (4%). Thus, evaluation of glenoid bone loss is crucial for surgical decision making in patients with anterior glenohumeral instability. Several preoperative imaging studies2,5,13–23 and intraoperative arthroscopic methods12,24–26 with many different measuring techniques have been proposed to assess glenoid bone loss. For intraoperative evaluation, Burkhart12,26 was the first to propose using the glenoid bare spot (GBS) as a reference point during arthroscopic examination. He defined the GBS as always located at the center of the inferior glenoid, and measured the distance from the GBS to the anterior rim (Da) and posterior rim (Dp) using a graduated probe with 3 mm calibrated marks inserted through the posterior portal. Using Burkhart’s method, the width of the preinjury glenoid is two times Dp, and the length of the bone loss is Dp – Da. Therefore, the percentage bone loss equals Dp – Da/Dp ×2. However, several authors27–30 have questioned this method, claiming that the GBS is not consistently located at the center of the inferior glenoid and/or that the GBS is not always found arthroscopically. Kralinger et al28 found that the GBS was located approximately 1.4 mm anterior to the true center of the glenoid. Saintmard et al29 reported finding the GBS in only half of 58 consecutive patients during arthroscopic examination. Recently, Barcia et al30 reported that the GBS was observed in only 48% of patients undergoing arthroscopic surgery and, when observed, was at the center only 37% of the time.
To investigate the validity of the arthroscopic GBS method, we sought to determine whether the GBS is consistently located at the center of the normal glenoid in patients without instability, and to compare the percentage bone loss as determined by preoperative three-dimensional computed tomography (3D-CT) evaluation and by the arthroscopic GBS method in patients with anterior glenohumeral instability. Our hypotheses were that the GBS is not consistently located at the center of the normal glenoid and that therefore the percentage bone loss calculated by the arthroscopic GBS method will sometimes differ from that obtained by preoperative 3D-CT evaluation.
Materials and methods
Subjects
From December 2008 to December 2011, 40 consecutive patients with anterior instability (30 males, ten females; mean age 25.9 years; range 15–72 years) who underwent shoulder arthroscopy were prospectively evaluated for the amount of glenoid bone loss with preoperative 3D-CT and arthroscopic examination. Of these, 37 patients underwent arthroscopic Bankart repair, and three underwent open Latarjet reconstruction. To investigate the location of the GBS in the normal glenoid, 27 patients without instability (18 males, nine females; mean age 59.1 years; range 38–74 years) were recruited. Of these 27 patients, 25 underwent arthroscopic rotator cuff repair. One patient underwent arthroscopic subacromial decompression and another underwent arthroscopic capsular release. None of the patients had any history of pain or injury in their nonoperative shoulders.
CT evaluation
All patients underwent CT scanning of both shoulders preoperatively. The images were taken using a SOMATOM Sensation Cardiac 64 (Siemens AG, Munich, Germany), and conventional volume-rendering 3D-CT images were obtained. A single orthopedic surgeon performed all CT measurements.
CT examinations were performed on the patients without glenoid bone loss, to exclude patients with obviously abnormally shaped glenoids. According to Chuang et al,23 the glenoid height (H1) is defined as the maximum longitudinal length of the en face view of the uninjured glenoid. The glenoid width (W1) is defined as the maximum length of the inferior glenoid perpendicular to H1 (Figure 1). In the operative shoulder, the maximum longitudinal (H2) and transverse (W2) lengths were compared with measurements from the contralateral uninjured shoulder. If the value of W1/H1 was less than 95% or more than 105% of the value of W2/H2, the shape of the glenoid was considered abnormal and the patient was excluded from the study. Patients with obvious deformity such as osteoarthritic change in the uninjured shoulder were also excluded.
Figure 1.
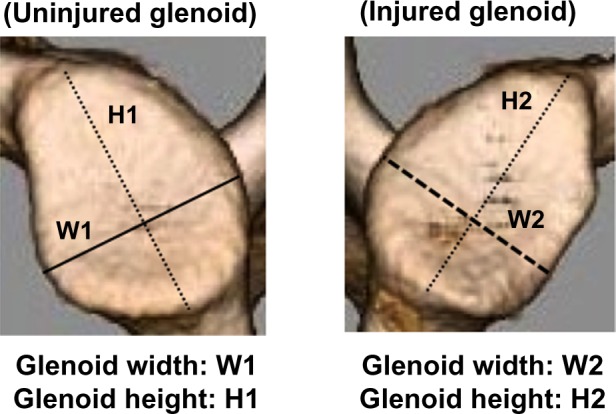
Uninjured glenoid: H1 represents the long axis of the glenoid, and W1 is the widest portion of the inferior glenoid perpendicular to H1. Injured glenoid: H2 and W2 correspond with H1 and W1 in the uninjured glenoid. The predicted preinjury width of the injured glenoid (W2′) can be calculated with the following formula: W2′ = (W1/H1) × H2. Percentage glenoid bone loss was calculated using the following formula: percentage glenoid bone loss = (1 − W2/W2′) × 100 (%).
To measure the percentage glenoid bone loss in patients with instability, the maximum longitudinal (H2) and transverse (W2) lengths of the injured glenoid were measured in a similar manner (Figure 1). The predicted preinjury width (W2′) of the injured glenoid was calculated with the following formula: W2′ = (W1/H1) × H2. The percentage glenoid bone loss was calculated with the following formula: percentage glenoid bone loss = (1 − W2/W2′) × 100 (%) (Figure 1).
Arthroscopic evaluation
Arthroscopic examination was performed in the beach chair position (patients without instability) or lateral decubitus position (patients with instability). According to Burkhart et al’s26 method, the anterosuperior portal was used as the viewing portal. A graduated probe with 2 mm calibrated marks was passed through the posterior portal and placed across the glenoid so that its tip rested on the bare spot. The distance from the center of the GBS to the posterior glenoid rim (Dp) was measured. The probe was then used to measure the distance from the anterior glenoid rim to the center of the GBS (Da) (Figures 2 and 3). The distance was measured by a 1 mm unit. We compared Dp and Da in patients without instability to determine whether the bare spot is located in the center of the inferior glenoid when no bone defect is present. In patients with instability, percentage glenoid bone loss was calculated using the following formula: percentage glenoid bone loss = (1 − [Da + Dp]/[Dp × 2]) × 100 (%).
Figure 2.
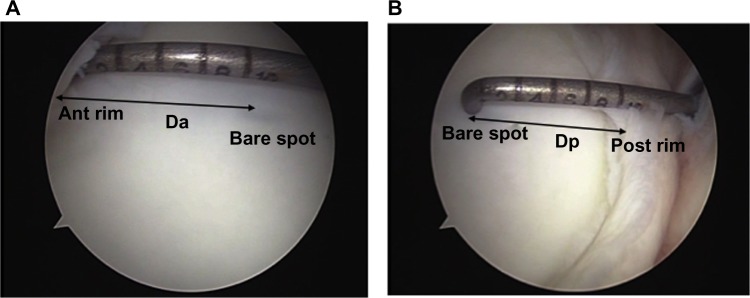
(A) Right shoulder with normal glenoid as viewed through the anterosuperior portal. The tip of the calibrated probe is placed at the anterior rim of the glenoid. Anterior (Da) is the distance between the anterior glenoid rim and the center of the bare spot. (B) The tip of the probe is placed at the center of the bare spot.
Abbreviations: Ant, anterior; Post, posterior.
Figure 3.
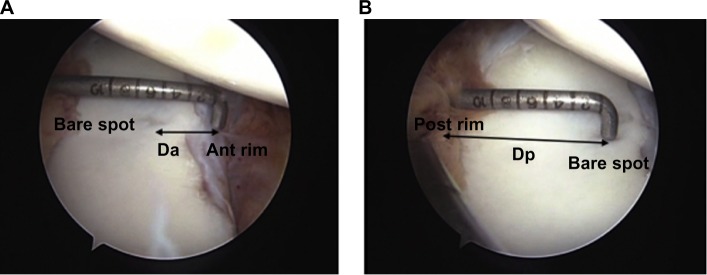
Left shoulder with glenoid bone loss as viewed through the anterosuperior portal. Distances from the center of the bare spot to the anterior (Da) and posterior (Dp) rim of the glenoid are measured in the same way as in the normal glenoid. Percentage glenoid bone loss is calculated using the following formula: percentage glenoid bone loss = (1 − [Da + Dp]/[Dp × 2]) × 100 (%).
Abbreviations: Ant, anterior; Post, posterior.
Arthroscopic measurements were determined by the consensus of two orthopedic surgeons who have more than 15 years of experience in shoulder arthroscopy.
Statistical analyses
Paired t-test was used to compare Da and Dp in glenoids without bone loss. Pearson’s correlation coefficient was used to determine the correlation between the percentage glenoid bone loss as calculated by CT and by arthroscopic measurements. The level of significance was set at P<0.05.
Results
Among the 27 patients with no evidence of instability, the mean percentage of W1/H1 to W2/H2 measured on 3D-CT images was 102%±6.1% (range 93.1%–121.7%). Five patients were excluded from this study because percentage was less than 95% or more than 105% (two patients) or because we could not identify the GBS arthroscopically (three patients). Among 22 patients, the mean Da was 9.5±1.2 mm (range 8~12 mm) and the mean Dp was 10.1±1.5 mm (range 8~14 mm). There was no significant difference between Da and Dp (P=0.065). Da and Dp were identical in eight glenoids, Da was greater than Dp in three glenoids, and Dp was greater than Da in eleven glenoids. Four glenoids showed more than 2 mm difference between Da and Dp.
Among the 40 patients with anterior glenohumeral instability, five were excluded because the GBS could not be identified arthroscopically. Of the remaining 35 patients, the mean percentage glenoid bone loss calculated by 3D-CT measurement was 13.6%±9.3% (range 0%–35.4%) and the mean percentage loss calculated by arthroscopic measurement was 15.1%±10.0% (range −5.0% to 31.8%). Pearson’s correlation coefficient showed significant (P<0.001) and strong (R2=0.63) correlation between the percentage bone loss of these measurement methods. However, ten shoulders (29%) had greater than 5% difference in percentage glenoid bone loss, as determined by 3D-CT versus arthroscopic measurement, and the difference was greater than 10% in five shoulders (14.5%) (Figure 4).
Figure 4.
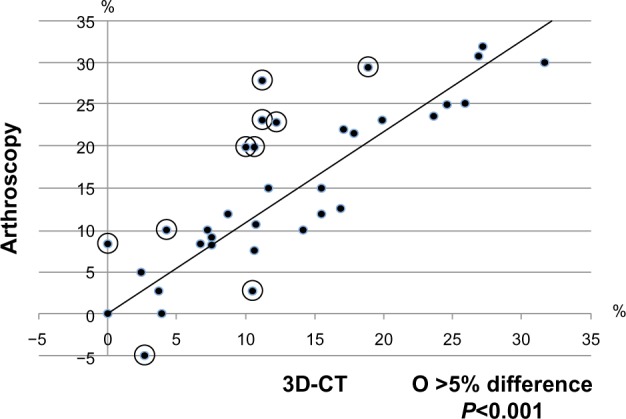
Correlation of percentage glenoid bone loss as calculated by preoperative three-dimensional computed tomography (3D-CT) versus arthroscopic measurements. A circle indicates a glenoid with more than 5% difference between the 3D-CT and arthroscopic measurements.
Discussion
Our results supported our hypotheses that the GBS is not consistently located at the center of the inferior glenoid without bone loss and that the percentage glenoid bone loss as measured by 3D-CT and by arthroscopic GBS methods was different in some cases with anterior glenohumeral instability.
Burkhart et al26 arthroscopically measured the distance from the center of the GBS to the anterior and posterior glenoid rim in 56 patients with no evidence of instability, and reported that Da and Dp were almost identical. They also measured Da and Dp in ten cadaver glenoids, and again found identical distances. However, Kralinger et al28 questioned the validity of using the GBS as a central reference point. They measured Da and Dp in 20 embalmed glenoids and reported that the mean Da (10.9 mm) was significantly shorter than the mean Dp (13.7 mm). In the present study, we arthroscopically measured Da and Dp in normally shaped glenoids. The results demonstrated that Da and Dp were significantly different. Among 22 glenoids, only twelve (55%) showed less than 1 mm of difference between Da and Dp, and four (18%) showed more than 2 mm difference.
To illustrate to what extent the Da–Dp difference influences the calculation of percentage glenoid bone loss, suppose the original glenoid width is 26 mm and glenoid bone loss is 5 mm. In this case, the glenoid bone loss is 19%. When the GBS center is located 1 mm anterior to the true center (Da – Dp = 2mm), the calculated loss is 25%. Although there is no consensus on the percentage glenoid bone loss that is significant for surgical decision making, several basic10,11 and clinical studies2,4,8,9,12 have suggested 25% glenoid bone loss as the cut-off for bone grafting. If the variability of the GBS location in the present study is found in the general population, and if the surgical procedure is chosen based on the arthroscopic GBS method alone, then bone grafting procedures would be performed on a substantial percentage of patients who should be candidates for arthroscopic Bankart repair.
Chuang et al23 investigated the validity of 3D-CT measurement on the choice of surgical procedure for patients who underwent arthroscopic Bankart repair versus open Latarjet reconstruction, based on this arthroscopic method. They reported that 3D-CT scans accurately predicted arthroscopic decisions in 24 (96%) of 25 cases. However, they did not describe the exact values of percentage glenoid bone loss with the arthroscopic GBS measurement. Therefore, the difference between the percentage glenoid bone loss as determined by arthroscopic versus 3D-CT measurements is unknown. In the present study, the results of the percentage glenoid bone loss measured by 3D-CT and arthroscopic GBS methods were strongly correlated. However, a difference of more than 5% between the methods was found in ten glenoids (29%), and the difference was greater than 10% in five glenoids. In most cases, the arthroscopic GBS method overestimated the percentage glenoid bone loss. Detterline et al24 created 12.5% and 25% bone loss in seven embalmed cadaveric shoulders and measured the percentage glenoid bone loss by the arthroscopic GBS method. They reported that the arthroscopic GBS measurement showed greater percentage glenoid bone loss compared with actual bone loss (22.2% and 30.4%, respectively). The GBS method’s overestimation of bone loss shown in Detterline et al’s24 study and in the present study is partly explained by the fact that the GBS is located anterior to the true center of the inferior glenoid in many cases.
Several studies29–31 have indicated that it is not always possible to identify the GBS. Huysmans et al31 reported that the GBS could not be identified in five of 40 cadaveric scapulae (12.5%). Saintmard et al29 prospectively investigated the presence of the GBS in 58 consecutive patients and could find the GBS in only 28 patients (48%). They concluded that the GBS is an unreliable landmark to determine the center of the inferior glenoid because it was present in only half of the shoulders studied. Barcia et al30 reported that the GBS was observed in only 48% of the patients undergoing arthroscopic surgery of the shoulder without a diagnosis of instability. They also concluded that the GBS should not be used as the sole reference point to measure glenoid bone loss. In the present study, the GBS could not be identified in five of 40 glenoids with anterior glenohumeral instability (12.5%). Two of these five patients underwent open Latarjet reconstruction because the preoperative 3D-CT showed more than 25% glenoid bone loss. Both patients had a long history with multiple dislocations. Precise evaluation of glenoid bone loss should be performed, especially in patients with similar histories. However, if surgeons rely on the arthroscopic GBS method and perform arthroscopy without preoperative 3D-CT evaluation, they are likely to choose the wrong surgical procedure in some cases.
In our experience, the arthroscopic probe did not always intersect the GBS when the tip of the probe was located at the center of the anterior–inferior bony defect through the posterior portal. Although Burkhart et al26 recommended a more inferior placement for the posterior portal than standard placement, Detterline et al24 reported that the arthroscopic probe did not always intersect the GBS, regardless of whether the posterior portal was placed at the 10 o’clock or 9 o’clock position. Moreover, the GBS was sometimes identified not as circular but rather as broad and irregularly shaped. In these cases, it was difficult to determine the true center of the bare spot.
Limitations
The present study had some limitations. First, the mean age of patients without shoulder instability was substantially higher than that of patients with anterior glenohumeral shoulder instability. However, Burkhart et al26 reported that the bare spot was located in the center of the inferior glenoid in cadaver shoulders with a mean age of 76 years, as well as in younger living subjects.
Second, we did not investigate our measurement reliability of the arthroscopic GBS method. Intrarater reliability is difficult to determine in patients, and arthroscopic measurements were performed by the consensus of two orthopedic surgeons who had substantial experience in shoulder arthroscopy.
Third, the two orthopedic surgeons who performed the arthroscopic GBS method were not blind to the results of CT evaluation prior to surgery.
Finally, we did not evaluate the role of magnetic resonance imaging (MRI) in the measurement of glenoid bone loss. To avoid radiation exposure, MRI is preferable if the ability of MRI for assessing the glenoid bone loss is comparable with that of 3D-CT. However, whether MRI can be an alternative for this purpose is still the matter of debate.32–35 In our experience, we believe that 3D-CT is superior to MRI for evaluating glenoid bone loss.
Conclusion
The bare spot is not consistently located at the center of the inferior glenoid, and the arthroscopic measurement of glenoid bone loss using the GBS as a landmark may not be accurate for some patients. To evaluate glenoid bone loss precisely, it is preferable to combine the bare spot method with preoperative 3D-CT evaluation.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Gerber C, Nyffeler RW. Classification of glenohumeral joint instability. Clin Orthop Relat Res. 2002;(400):65–76. doi: 10.1097/00003086-200207000-00009. [DOI] [PubMed] [Google Scholar]
- 2.Bigliani LU, Newton PM, Steinmann SP, Connor PM, McLlveen SJ. Glenoid rim lesions associated with recurrent anterior dislocation of the shoulder. Am J Sports Med. 1998;26(1):41–45. doi: 10.1177/03635465980260012301. [DOI] [PubMed] [Google Scholar]
- 3.Boileau P, Villalba M, Hery JY, Balg F, Ahrens P, Neyton L. Risk factors for recurrence of shoulder instability after arthroscopic Bankart repair. J Bone Joint Surg Am. 2006;88(8):1755–1763. doi: 10.2106/JBJS.E.00817. [DOI] [PubMed] [Google Scholar]
- 4.Lo IK, Parten PM, Burkhart SS. The inverted pear glenoid: an indicator of significant glenoid bone loss. Arthroscopy. 2004;20(2):169–174. doi: 10.1016/j.arthro.2003.11.036. [DOI] [PubMed] [Google Scholar]
- 5.Sugaya H, Moriishi J, Dohi M, Kon Y, Tsuchiya A. Glenoid rim morphology in recurrent anterior glenohumeral instability. J Bone Joint Surg Am. 2003;85-A(5):878–884. doi: 10.2106/00004623-200305000-00016. [DOI] [PubMed] [Google Scholar]
- 6.Warner JJ, Gill TJ, O’Hollerhan JD, Pathare N, Millett PJ. Anatomical glenoid reconstruction for recurrent anterior glenohumeral instability with glenoid deficiency using an autogenous tricortical iliac crest bone graft. Am J Sports Med. 2006;34(2):205–212. doi: 10.1177/0363546505281798. [DOI] [PubMed] [Google Scholar]
- 7.Mologne TS, Provencher MT, Menzel KA, Vachon TA, Dewing CB. Arthroscopic stabilization in patients with an inverted pear glenoid: results in patients with bone loss of the anterior glenoid. Am J Sports Med. 2007;35(8):1276–1283. doi: 10.1177/0363546507300262. [DOI] [PubMed] [Google Scholar]
- 8.Scheibel M, Magosch P, Lichtenberg S, Habermeyer P. Open reconstruction of anterior glenoid rim fractures. Knee Surg Sports Traumatol Arthrosc. 2004;12(6):568–573. doi: 10.1007/s00167-004-0495-7. [DOI] [PubMed] [Google Scholar]
- 9.Longo UG, Loppini M, Rizzello G, Romeo G, Huijsmans PE, Denaro V. Glenoid and humeral head bone loss in traumatic anterior glenohumeral instability: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2014;22(2):392–414. doi: 10.1007/s00167-013-2403-5. [DOI] [PubMed] [Google Scholar]
- 10.Itoi E, Lee SB, Berglund LJ, Berge LL, An KN. The effect of a glenoid defect on anteroinferior stability of the shoulder after Bankart repair: a cadaveric study. J Bone Joint Surg Am. 2000;82(1):35–46. doi: 10.2106/00004623-200001000-00005. [DOI] [PubMed] [Google Scholar]
- 11.Yamamoto N, Muraki T, Sperling JW, et al. Stabilizing mechanism in bone-grafting of a large glenoid defect. J Bone Joint Surg Am. 2010;92(11):2059–2066. doi: 10.2106/JBJS.I.00261. [DOI] [PubMed] [Google Scholar]
- 12.Burkhart SS, De Beer JF. Traumatic glenohumeral bone defects and their relationship to failure of arthroscopic Bankart repairs: significance of the inverted-pear glenoid and the humeral engaging Hill-Sachs lesion. Arthroscopy. 2000;16(7):677–694. doi: 10.1053/jars.2000.17715. [DOI] [PubMed] [Google Scholar]
- 13.Barchilon VS, Kotz E, Barchilon Ben-Av M, Glazer E, Nyska M. A simple method for quantitative evaluation of the missing area of the anterior glenoid in anterior instability of the glenohumeral joint. Skeletal Radiol. 2008;37(8):731–736. doi: 10.1007/s00256-008-0506-8. [DOI] [PubMed] [Google Scholar]
- 14.Murachovsky J, Bueno RS, Nascimento LG, et al. Calculating anterior glenoid bone loss using the Bernageau profile view. Skeletal Radiol. 2012;41(10):1231–1237. doi: 10.1007/s00256-012-1439-9. [DOI] [PubMed] [Google Scholar]
- 15.Itoi E, Lee SB, Amrami KK, Wenger DE, An KN. Quantitative assessment of classic anteroinferior bony Bankart lesions by radiography and computed tomography. Am J Sports Med. 2003;31(1):112–118. doi: 10.1177/03635465030310010301. [DOI] [PubMed] [Google Scholar]
- 16.de Filippo M, Castagna A, Steinbach LS, et al. Reproducible noninvasive method for evaluation of glenoid bone loss by multiplanar reconstruction curved computed tomographic imaging using a cadaveric model. Arthroscopy. 2013;29(3):471–477. doi: 10.1016/j.arthro.2012.10.017. [DOI] [PubMed] [Google Scholar]
- 17.Bois AJ, Fening SD, Polster J, Jones MH, Miniaci A. Quantifying glenoid bone loss in anterior shoulder instability: reliability and accuracy of 2-dimensional and 3-dimensional computed tomography measurement techniques. Am J Sports Med. 2012;40(11):2569–2577. doi: 10.1177/0363546512458247. [DOI] [PubMed] [Google Scholar]
- 18.Dumont GD, Russell RD, Browne MG, Robertson WJ. Area-based determination of bone loss using the glenoid arc angle. Arthroscopy. 2012;28(7):1030–1035. doi: 10.1016/j.arthro.2012.04.147. [DOI] [PubMed] [Google Scholar]
- 19.Nofsinger C, Browning B, Burkhart SS, Pedowitz RA. Objective preoperative measurement of anterior glenoid bone loss: a pilot study of a computer-based method using unilateral 3-dimensional computed tomography. Arthroscopy. 2011;27(3):322–329. doi: 10.1016/j.arthro.2010.09.007. [DOI] [PubMed] [Google Scholar]
- 20.Hantes ME, Venouziou A, Bargiotas KA, Metafratzi Z, Karantanas A, Malizos KN. Repair of an anteroinferior glenoid defect by the latarjet procedure: quantitative assessment of the repair by computed tomography. Arthroscopy. 2010;26(8):1021–1026. doi: 10.1016/j.arthro.2010.05.016. [DOI] [PubMed] [Google Scholar]
- 21.Diederichs G, Seim H, Meyer H, et al. CT-based patient-specific modeling of glenoid rim defects: a feasibility study. AJR Am J Roentgenol. 2008;191(5):1406–1411. doi: 10.2214/AJR.08.1091. [DOI] [PubMed] [Google Scholar]
- 22.Griffith JF, Yung PS, Antonio GE, Tsang PH, Ahuja AT, Chan KM. CT compared with arthroscopy in quantifying glenoid bone loss. AJR Am J Roentgenol. 2007;189(6):1490–1493. doi: 10.2214/AJR.07.2473. [DOI] [PubMed] [Google Scholar]
- 23.Chuang TY, Adams CR, Burkhart SS. Use of preoperative three-dimensional computed tomography to quantify glenoid bone loss in shoulder instability. Arthroscopy. 2008;24(4):376–382. doi: 10.1016/j.arthro.2007.10.008. [DOI] [PubMed] [Google Scholar]
- 24.Detterline AJ, Provencher MT, Ghodadra N, Bach BR, Jr, Romeo AA, Verma NN. A new arthroscopic technique to determine anterior-inferior glenoid bone loss: validation of the secant chord theory in a cadaveric model. Arthroscopy. 2009;25(11):1249–1256. doi: 10.1016/j.arthro.2009.05.019. [DOI] [PubMed] [Google Scholar]
- 25.Provencher MT, Detterline AJ, Ghodadra N, et al. Measurement of glenoid bone loss: a comparison of measurement error between 45 degrees and 0 degrees bone loss models and with different posterior arthroscopy portal locations. Am J Sports Med. 2008;36(6):1132–1138. doi: 10.1177/0363546508316041. [DOI] [PubMed] [Google Scholar]
- 26.Burkhart SS, Debeer JF, Tehrany AM, Parten PM. Quantifying glenoid bone loss arthroscopically in shoulder instability. Arthroscopy. 2002;18(5):488–491. doi: 10.1053/jars.2002.32212. [DOI] [PubMed] [Google Scholar]
- 27.Aigner F, Longato S, Fritsch H, Kralinger F. Anatomical considerations regarding the “bare spot” of the glenoid cavity. Surg Radiol Anat. 2004;26(4):308–311. doi: 10.1007/s00276-003-0217-8. [DOI] [PubMed] [Google Scholar]
- 28.Kralinger F, Aigner F, Longato S, Rieger M, Wambacher M. Is the bare spot a consistent landmark for shoulder arthroscopy? A study of 20 embalmed glenoids with 3-dimensional computed tomographic reconstruction. Arthroscopy. 2006;22(4):428–432. doi: 10.1016/j.arthro.2005.12.006. [DOI] [PubMed] [Google Scholar]
- 29.Saintmard B, Lecouvet F, Rubini A, Dubuc JE. Is the bare spot a valid landmark for glenoid evaluation in arthroscopic Bankart surgery? Acta Orthop Belg. 2009;75(6):736–742. [PubMed] [Google Scholar]
- 30.Barcia AM, Rowles DJ, Bottoni CR, Dekker TJ, Tokish JM. Glenoid bare area: arthroscopic characterization and its implications on measurement of bone loss. Arthroscopy. 2013;29(10):1671–1675. doi: 10.1016/j.arthro.2013.06.019. [DOI] [PubMed] [Google Scholar]
- 31.Huysmans PE, Haen PS, Kidd M, Dhert WJ, Willems JW. The shape of the inferior part of the glenoid: a cadaveric study. J Shoulder Elbow Surg. 2006;15(6):759–763. doi: 10.1016/j.jse.2005.09.001. [DOI] [PubMed] [Google Scholar]
- 32.Gyftopoulos S, Beltran LS, Yemin A, et al. Use of 3D MR reconstructions in the evaluation of glenoid bone loss: a clinical study. Skeletal Radiol. 2014;43(2):213–218. doi: 10.1007/s00256-013-1774-5. [DOI] [PubMed] [Google Scholar]
- 33.Stecco A, Guenzi E, Cascone T, et al. MRI can assess glenoid bone loss after shoulder luxation: inter- and intra-individual comparison with CT. Radiol Med. 2013;118(8):1335–1343. doi: 10.1007/s11547-013-0927-x. [DOI] [PubMed] [Google Scholar]
- 34.Rerko MA, Pan X, Donaldson C, Jones GL, Bishop JY. Comparison of various imaging techniques to quantify glenoid bone loss in shoulder instability. J Shoulder Elbow Surg. 2013;22(4):528–534. doi: 10.1016/j.jse.2012.05.034. [DOI] [PubMed] [Google Scholar]
- 35.Bishop JY, Jones GL, Rerko MA, Donaldson C. 3-D CT is the most reliable imaging modality when quantifying glenoid bone loss. Clin Orhtop Relat Res. 2013;471(4):1251–1256. doi: 10.1007/s11999-012-2607-x. [DOI] [PMC free article] [PubMed] [Google Scholar]


