Abstract
The cost of managing end stage renal disease (ESRD) is prohibitive in Nigeria and the burden is solely borne by patients and their relatives. Despite increasing number of dialysis centers in urban areas, actual utilization of such facilities is very low. It is unclear if the outcomes of these patients have improved in recent times. We evaluated pattern of hemodialysis (HD) performance and outcome among ESRD patients. A 5-year prospective cross-sectional study of all ESRD patients on HD was undertaken. The final outcomes included duration on maintenance dialysis, death from inability to sustain dialysis, absconded, confirmed deaths within or outside health facility or referral for kidney transplant. A total of 540 (54%) of 976 cases of ESRD commenced HD, out of which 7 (1.3%) eventually had live-related kidney transplant in India. The male to female ratio was 2:1 with male and female mean ages of 43 ± 17 and 36 ± 16 years respectively. There was a progressive annual increase in the number of ESRD patients. The commonest underlying renal disorder was chronic glomerulonephritis. The mean HD session duration was 8.11 ± 5.4 hours, while the mean duration of stay on HD was 8.72 ± 1.0 weeks. In conclusion, ESRD is common and is being increasingly recognized. Financial constraint and late presentation are major contributory factors to poor outcomes despite the widespread availability of HD facilities. Therefore, effort should be geared towards aggressive strategies for early detection and treatment. Government commitment in terms of funding and/or subsidy for patient with ESRD is advocated.
Keywords: End stage renal disease, hemodialysis, Nigeria, outcome, performance
Introduction
Hemodialysis (HD) is the most common form of renal replacement therapy (RRT) for end stage renal disease (ESRD) world-wide. Unlike in the developed world, where HD facilities are readily available and accessible to patients because of efficient social security system and/or health insurance schemes, such assistance is virtually non-existent in tropical developing countries.[1,2,3] ESRD contributes significantly to manpower shortage and economic waste in Nigeria as the peak prevalence is in the 3rd to 4th decade of life.[3,4] Despite the increasing number of dialysis centers in urban areas of Nigeria, actual utilization of such facilities remain very low because of the prohibitive cost.[4] More importantly, there is no social security system or health insurance scheme in place to assist these very poor patients, resulting in the burden being borne solely by patients and their relatives.[4] Therefore, ESRD frequently results in unnecessary suffering and premature death of our patient who can neither afford nor sustain the high cost of therapy. Majority of these patients with ESRD die within 3 months of commencing HD because of inability to sustain regular therapy. It is unclear if the outcomes of these patients have improved in recent times. We therefore evaluated pattern of ESRD and HD performance outcome in Usmanu Danfodiyo University Teaching Hospital (UDUTH), Sokoto, Nigeria.
Materials and Methods
UDUTH, Sokoto serves as the referral center for patients with renal failure from Sokoto, Kebbi, and Zamfara states. A 5-year-cross-sectional study of all ESRD patients enrolled into HD program from July 2007 to December 2012 was done. Information obtained included socio-demographics, clinical presentation, bio-data characteristics and etiology of ESRD, vascular access, biochemical data and duration on dialysis and outcome at the end of the study period. Outcome measures include maximum duration of HD, death, absconded and referral for transplant. ESRD was diagnosed by calculating estimated glomerular filtration rate (eGFR) from serum creatinine utilizing modification of diet in renal disease (MDRD) equation.[2] All patients with eGFR ≤15 ml/min for ≥3months had ESRD with reference to kidney disease improving global outcome (KDIGO) staging system. Patient seen either in the clinic or admitted with chronic kidney disease were recruited but only those with ESRD as defined by KDIGO were analyzed.[1] Patients who had signs and symptoms of renal disease ≥3months, eGFR ≤15 ml/min, renal length by ultrasound <9cm and/or complete loss of corticomedullary differentiation or dependence on HD were included.
The diagnosis of causative factors was derived from documented clinical features and the results of relevant investigative procedures which included: Urinlysis, blood biochemistry, urinary system imaging and renal tissue histology. Chronic glomerulonephritis (CGN) was diagnosed in the presence of more than 3 months history of renal disease, biochemical evidence of nephrotic syndrome, past medical history of profuse proteinuria noted biochemically or recognized by the patient as frothy urine and/or histological evidence of glomerular disease defined by examination of either biopsy or autopsy specimen. Hypertensive nephrosclerosis was diagnosed in a setting that include a history of hypertension for more than 1 year, diastolic blood pressure usually above 110 mmHg, presence of grade 3 hypertensive retinopathy, features of left ventricular hypertrophy and aortic unfolding, presence of microscopic hematuria and moderate proteinuria or renal tissue histologic changes.
Our diagnosis of diabetic nephropathy was based on the history of diabetes mellitus for more than 10 years duration, proteinuria of over 0.5 g/24 h, presence of systemic hypertension and retinal changes consistent with diabetic retinopathy. The other causes of end stage kidney disease like polycystic kidney disease, obstructive uropathy (benign prostate hypertrophy, carcinoma of prostate and carcinoma of the cervix) and connective tissue disease were based on history, physical findings and appropriate investigation where applicable. Patients in whom definite etiological factor could not be implicated from the records were classified as unknown. The final outcome include the following: maximum duration on maintenance dialysis, dead from inability to sustain dialysis, absconded, confirmed dead within or outside health facility or referred for kidney transplant.
Statistical analysis
Data analysis was performed using the statistical package for social science software (SPSS) version 17. Continuous and categorical variables were displayed as means ± standard deviation and percentages respectively. Categorical variables were compared using non-parametric tests of Chi-squares and P values were set at 0.05.
Results
A total of 540 (54%) of 976 cases of ESRD commenced HD, out of which 7 (1.3%) eventually had live-related kidney transplant after a variable period on dialysis. There were 360 males with a male to female ratio of 2:1. Overall mean age was 40.5 ± 18.6 years while male and female mean ages were 43 ± 17 years and 36 ± 16 years respectively. The difference was statistically significant (P < 0.01). The commonest underlying renal disorder was CGN followed by hypertensive nephrosclerosis, obstructive uropathy (carcinoma of prostate, benign prostatic hypertrophy, carcinoma of bladder and carcinoma of the cervix) and diabetes mellitus (DM) [Table 1]. There was a progressive annual increase in the number of ESRD patients enrolled into HD program [Figure 1].
Table 1.
Etiology of ESRD
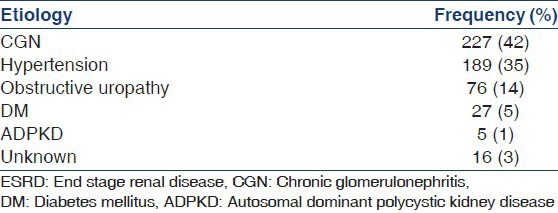
Figure 1.
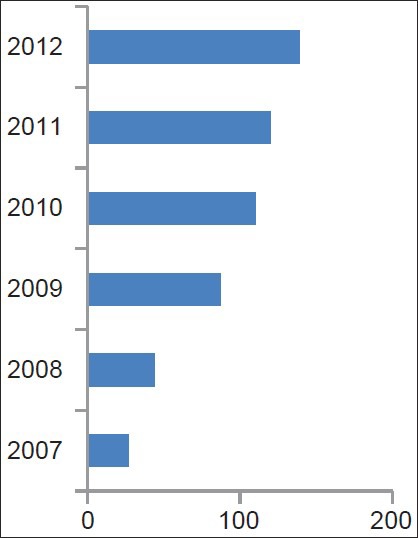
Yearly distribution of cases
Majority of patients had less than five sessions HD before defaulting with a range of 1-312 and mean 8.11 ± 5.4 sessiton while the duration of stay on HD was 1-208 weeks with a mean 8.72 ± 1.0 weeks [Tables 2 and 3]. It was only 10% that had more than 15 sessions of dialysis and only about 12.5% could sustain it for more than 3 months. Our center has not yet commenced peritoneal dialysis and kidney transplantation. The seven cases that had transplantation were done in various hospitals in India [Figure 2].
Table 2.
No. of sessions
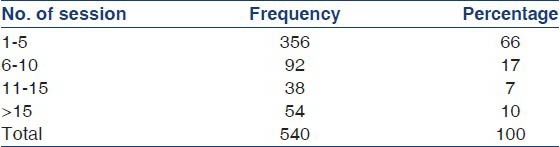
Table 3.
Duration of dialysis
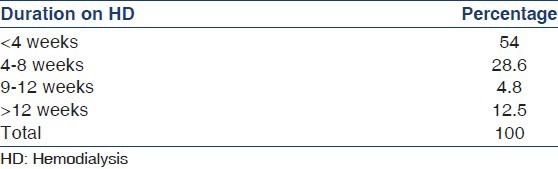
Figure 2.
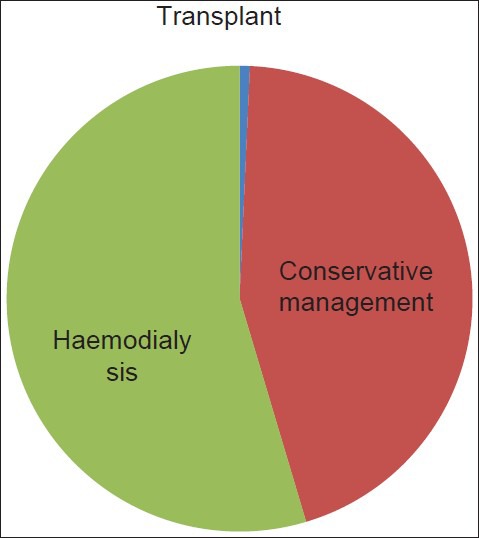
Mode of treatment modalities
Discussion
Our study has revealed that ESRD is common with progressive annual increase and a similar trend is prevalent in developed and developing countries.[5,6,7,8] CGN and hypertension were leading causes of ESRD in this study which is in accord with recent trends in other parts of Nigeria.[9,10,11,12] This contrasts with what obtains in developed countries where DM is most prevalent thus reflecting high prevalence of infectious disease in developing countries. The mean age of 40.5 ± 18.6 years observed in this study show that ESRD predominantly affects young adults and early middle age in contrast with the peak age of 70 years occurrence in Europe and America.[6,13] It is however, similar to reports from other centers from Nigeria.[8,14] There is male preponderance, which is in accord with findings from other studies.[9,10,15,16] The socio-economic implication of this finding is grave as males are main bread winners in most homes. It underscores the need for effective preventive measures as well as active cost-effective RRT.
Most of our patients could not afford the cost of RRT resulting in high default rate from treatment. Majority had less than five sessions of HD before discontinuing the program either by death or departure against medical advice. Most of the deaths occur within 3-6 months of therapy, which is similar to observations in other parts of Nigeria.[7,8,17] Main factors contributing to very poor HD performance and abysmal outcome after starting maintenance HD among our patients are late presentation, low index of clinical suspicion, inadequate diagnostic facilities and lack of financial ability to sustain long-term dialysis. Many of our patients presented at a stage requiring dialysis because of delay resulting from ignorance and superstitious beliefs, which often culminate in time wasting with spiritualists, herbalists and faith healers. Late presentation and delay in commencement of HD has been found to adversely affect outcome of these patients.[18,19] It is however, pertinent to note that HD has sustained life of more than a million ESRD patients worldwide and has remained the commonest form of RRT in Nigeria. Unfortunately, our study shows that more than 50% of our patients commenced HD, but only about 12% could afford to sustain at least two sessions per week for more than 12 weeks. Majority of the patients had less than five sessions of HD before defaulting because of financial constraint. The cost of managing ESRD is prohibitive the world over and in Nigeria, the burden of health care is solely borne by patients and relations. This is in accordance with what obtains in other developing nations.[4,8,20] Financial constraint has been and still remains the crucial factor culminating in treatment withdrawal among ESRD patients in sub-Saharan Africa.[3,11]
Renal transplantation represents 0.7% of the total ESRD managed in our study and accounted for 1.3% of those that commenced HD. All the cases had transplantation done at various hospitals in India. Although, our center has not commenced renal transplantation, there are very few centers in Nigeria where such services are offered in both private and government owned hospitals. Ulasi and Ijoma[4] reported that 0.3% of ESRD patients managed in their center had renal transplant.
ESRD is common and is increasingly being recognized. Financial constraint, late presentation and inadequate diagnostic facilities are major contributory factors to poor outcome in patients with the disease despite widespread availability of HD facilities. Therefore, effort should be geared toward aggressive strategies for early detection and treatment of the causes. Pressure group advocate should be put in place in order to get government commitment in terms of funding and/or subsidy for patient with ESRD.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Levey AS, Coresh J, Balk E, Kausz AT, Levin A, Steffes MW, et al. K/DOQI clinical practice guidelines for CKD: Evaluation, classification and stratification. Am J Kidney Dis. 2002;2:1–246. [Google Scholar]
- 2.Johnson CA, Levey AS, Coresh J, Levin A, Lau J, Eknoyan G. Clinical practice guidelines for chronic kidney disease in adults: Part I. Definition, disease stages, evaluation, treatment, and risk factors. Am Fam Physician. 2004;70:869–76. [PubMed] [Google Scholar]
- 3.Ijoma CK, Ulasi II, Kalu AO. Cost implication of treatment of end stage renal disease in Nigeria. J Coll Med. 1998;3:95–6. [Google Scholar]
- 4.Ulasi II, Ijoma CK. The enormity of chronic kidney disease in Nigeria: The situation in a teaching hospital in South-East Nigeria. J Trop Med 2010. 2010 doi: 10.1155/2010/501957. 501957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Levey AS, Atkins R, Coresh J, Cohen EP, Collins AJ, Eckardt KU, et al. Chronic kidney disease as a global public health problem: Approaches and initiatives – A position statement from kidney disease improving global outcomes. Kidney Int. 2007;72:247–59. doi: 10.1038/sj.ki.5002343. [DOI] [PubMed] [Google Scholar]
- 6.Bethesda, MD: National Institute of Diabetes, digestive and kidney diseases, National Institute of Health; 1991. US Renal Data System (USRD, 1991). Anunal Data Report. [Google Scholar]
- 7.Arije A, Kadiri S, Akinkugbe OO. The viability of hemodialysis as a treatment option for renal failure in a developing economy. Afr J Med MedSci. 2000;29:311–4. [PubMed] [Google Scholar]
- 8.Wokoma FS, Okafor HU. Haemodialysis experience with chronic kidney failure patients at the University of Port Harcourt Teaching Hospital: An analysis of data of the first year of operation. Trop J Nephrol. 2010;2:97–104. [Google Scholar]
- 9.Akinsola W, Odesanmi WO, Ogunniyi JO, Ladipo GO. Diseases causing chronic renal failure in Nigerians – A prospective study of 100 cases. Afr J Med MedSci. 1989;18:131–7. [PubMed] [Google Scholar]
- 10.Alebiosu CO, Ayodele OO, Abbas A, Olutoyin AI. Chronic renal failure at the Olabisi Onabanjo University Teaching Hospital, Sagamu, Nigeria. Afr Health Sci. 2006;6:132–8. doi: 10.5555/afhs.2006.6.3.132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Naicker S. End-stage renal disease in sub-Saharan and South Africa. Kidney Int Suppl. 2003;83:S119–22. doi: 10.1046/j.1523-1755.63.s83.25.x. [DOI] [PubMed] [Google Scholar]
- 12.Barson RS. Renal disease in indigenous populations. North Afr Nephrol. 1998;4:29–32. [Google Scholar]
- 13.Vol. 14. Basel: Switzerland: 1985. European Dialysis and Transplant Association. Combined report on regular dialysis and transplantation in Europe. [Google Scholar]
- 14.Chijioke A, Adeniyi AB. End stage renal disease: Racial differences. Orient J Med. 2003;15:24–31. [Google Scholar]
- 15.Dash SC, Agarwal SK. Incidence of chronic kidney disease in India. Nephrol Dial Transplant. 2006;21:232–3. doi: 10.1093/ndt/gfi094. [DOI] [PubMed] [Google Scholar]
- 16.Afshar R, Sanavi S, Salimi J. Epidemiology of chronic renal failure in Iran: A four year single-center experience. Saudi J Kidney Dis Transpl. 2007;18:191–4. [PubMed] [Google Scholar]
- 17.Odutola TA, Ositelu SB, D’Almeida EA, Mabadeje AF. Five years experience of haemodialysis at the Lagos University Teaching Hospital – November 1981 to November 1986. Afr J Med MedSci. 1989;18:193–201. [PubMed] [Google Scholar]
- 18.Alebiosu CO. Detrimental effects of late referral for dialysis. Afr J Health Sci. 2001;8:89–92. [PubMed] [Google Scholar]
- 19.Obrador GT, Pereira BJ. Early referral to the nephrologist and timely initiation of renal replacement therapy: A paradigm shift in the management of patients with chronic renal failure. Am J Kidney Dis. 1998;31:398–417. doi: 10.1053/ajkd.1998.v31.pm9506677. [DOI] [PubMed] [Google Scholar]
- 20.Wairaga SG. End stage renal disease in Africa: Conservative management. New Afr J Med. 1998;2:34–7. [Google Scholar]


