Figure 1.
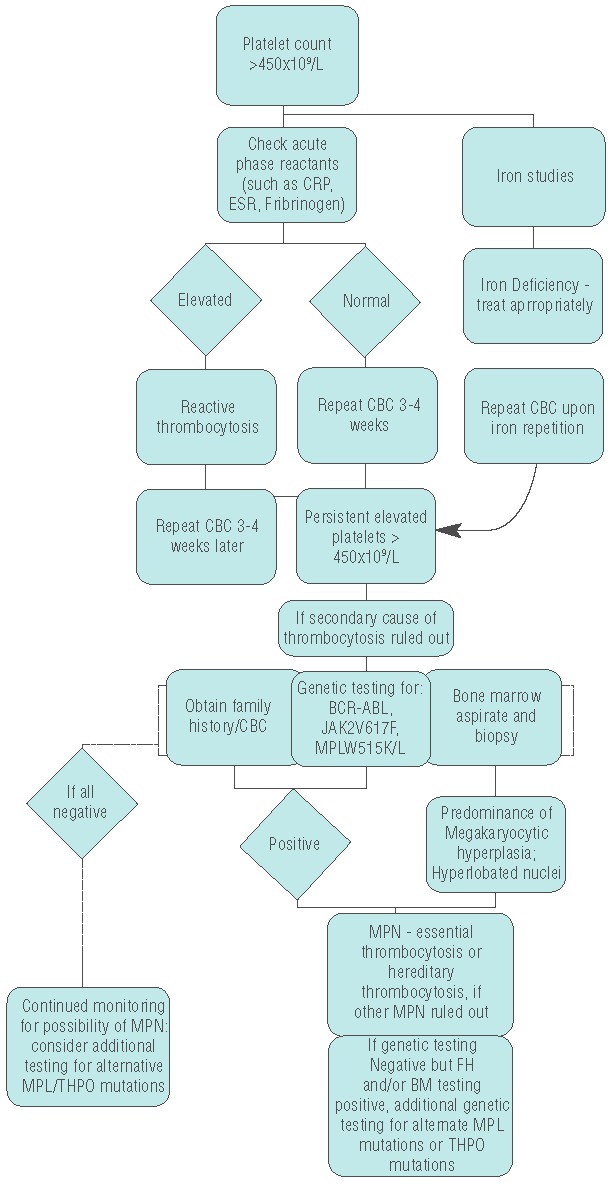
Diagnostic algorithm for persistent elevated platelets. Figure 1 shows our groups’ proposed diagnostic algorithm for approaching patients with elevated platelets. Evaluation for secondary causes, such as iron deficiency or inflammatory or infectious disorders is conducted. Iron deficiency and other underlying causes are treated. If no secondary cause is found, or treatment of the underlying disorder does not remedy the platelet count, further evaluation is done to look for signs of essential thrombocytosis. Bone marrow evaluation is recommended at this point. Also, genetic studies are recommended, and if there is clinical suspicion then BCR-ABL testing should be done. If it is not tested for, or if it is negative, testing for JAK2V617F or MPLW5151K/L is done. Positive JAK or MPL testing, and/or diagnostic bone marrow findings, contribute to the diagnosis of an MPN. Specific criteria for ET (or if needed, PV or PMF) are evaluated to identify the correct MPN. Concurrently, a detailed family history should be obtained to evaluate the possibility of hereditary thrombocytosis. Testing for alternative THPO or MPL mutations is recommended in the setting of presumed hereditary thrombocytosis. Absence of the more common genetic mutation does not rule out diagnosis of an MPN, and if no other cause is identified genetic testing for additional MPL or THPO mutations should be considered and patients should be monitored for the continued possibility of MPN.
