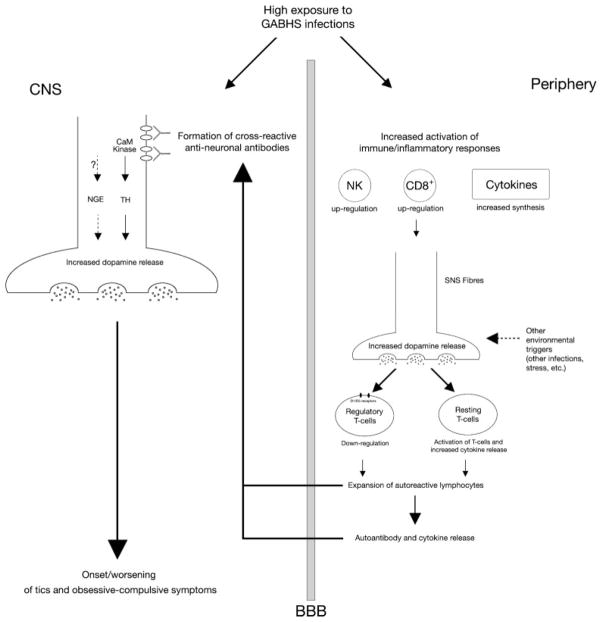
FIG. 1.
Proposed hypothetical model of immune-mediated basal ganglia dysfunction in tics and obsessive-compulsive symptoms. Group A β-hemolytic streptococcal (GABHS) infections induce the formation of cross-reactive autoantibodies which bind cell surface neuronal antigens. This binding might lead to increased calcium-calmodulin-dependent (CaM) kinase II activity, subsequent increase of tyrosine hydroxylase activity and enhanced dopamine release at the level of central synapses; alternatively autoantibodies might modulate the activity of membrane-bound neuronal glycolytic enzymes, thus leading to alterations in membrane excitability and to abnormal neurotransmitter release. In the periphery, GABHS infections may activate inflammatory responses, leading to Natural Killer and cytotoxic T cell functional up-regulation, and to increased synthesis of pro-inflammatory cytokines. This inflammatory background may enhance dopamine synthesis and release from sympathetic nervous system fibres, with the possible contribution of other environmental triggers, e.g. psychosocial stressors. Higher peripheral levels of dopamine may down-regulate the function of regulatory T cells and amplify the release of pro-inflammatory cytokines such as tumor necrosis factor (TNF)-α. These changes may ultimately lead to an enhanced autoimmune response and even greater dopamine release in the basal ganglia, which in turn contribute to onset or worsening of tics and obsessive-compulsive symptoms.