Summary
Objective
Relevant patient information is frequently difficult to obtain in emergency department (ED) visits. Improved provider access to previously inaccessible patient information may improve the quality of care and reduce hospital admissions. Health information exchange (HIE) systems enable access to longitudinal, community-wide patient information at the point of care. However, the ability of HIE to avert admissions is not well demonstrated. We sought to determine if HIE system usage is correlated with a reduction in admissions via the ED.
Methods
We identified 15,645 adults from New York State with an ED visit during a 6-month period, all of whom consented to have their information accessible in the HIE system, and were continuously enrolled in two area health plans. Using claims we determined if the ED encounter resulted in an admission. We used the HIE’s system log files to determine usage during the encounter. We determined the association between HIE system use and the likelihood of admission to the hospital from the ED and potential cost savings.
Results
The HIE system was accessed during 2.4% of encounters. The odds of an admission were 30% lower when the system was accessed after controlling for confounding (odds ratio = 0.70; 95%C I= 0.52, 0.95). The annual savings in the sample was $357,000.
Conclusion
These findings suggest that the use of an HIE system may reduce hospitalizations from the ED with resultant cost savings. This is an important outcome given the substantial financial investment in interventions designed to improve provider access to patient information in the US.
Key words: Health information exchange, computerized patient records, information systems, emergency department, admission
Introduction
Emergency department (ED) physicians must routinely make complex decisions in the absence of complete historical patient information. Estimates suggest that relevant patient information, including medication information, test results, and medical histories, may be difficult to obtain or unavailable in approximately 30% of visits to emergency settings [1, 2]. It is hypothesized that improving ED physicians’ access to more patient information could result in higher quality of care, including the prevention of potentially avoidable hospitalizations. It would be highly desirable to reduce the frequency of avoidable hospitalizations, because they are common and costly [3, 4].
Enabling physician access to more complete patient information is particularly relevant to the ED setting where longitudinal patient information from multiple providers is frequently not easily accessible due to a variety of patient and healthcare system factors. Patients present to the ED with urgent and unplanned health problems [5, 6] and often with fragmented care patterns [7, 8]. Health information exchange (HIE) systems facilitate the electronic sharing of patient level information among different providers in a community. Therefore, access to an HIE system could potentially avert unnecessary admissions from the ED by providing relevant clinical data, such as the presence of renal insufficiency or an electrocardiogram abnormality at baseline. This information could also potentially avert unnecessary admissions by providing access to lists of medications and problems as well as access to the medical opinions of previous physicians.
Evidence about the effectiveness of HIE systems to avert admissions is beginning to grow [9]. Recently, the MidSouth eHealth Alliance demonstrated HIE was effective in reducing admissions from the ED. Similar work in Israel also found HIE was associated with avoided admissions [10]. These recent findings stand in contrast to earlier studies that were not able to document any effects of HIE on admissions from the ED or on ED utilization [11–13].
This paper examines the hypothesis that usage of an HIE system reduces the odds that a patient in the ED will be hospitalized. This research seeks to add to our current understanding of the effectiveness of electronic exchange of health information, responds to the current call for more outcomes-based research [9], and considers a typical community-based setting using a commercially available product.
Methods
Setting
We conducted a retrospective cohort study in the Rochester, New York, area using encounters during 2009-2010. The Rochester Regional Health Information Organization (RHIO) is supported in part by the State Department of Health under New York’s Health Care Efficiency and Affordability Law for New Yorkers (HEAL NY) capital grants program. Founded in 2006 by a collaboration of payers, providers, public health agencies, and civic leaders, the Rochester RHIO is a non-profit organization that facilitates information exchange among more than 70 organizations in 13 county region of western New York [14]. This organization enables authorized physician and staff to access a web-based HIE system, which includes patients’ laboratory results, radiology reports and images, medication history, discharge summaries, and payer information [15]. Hospital systems, providers, reference laboratories, radiology groups, insurance companies, and county elder care offices contribute clinical data to the HIE. A previous investigation described usage patterns of the HIE’s commercially available web portal system [16].
At the time of the study (2009–2010), the HIE system’s 1,318 users accessed patient records in 156 different outpatient, emergency, inpatient, long-term care and specialty care settings via a web portal. Seven EDs were included. RHIO staff authorized users at practice sites to have access to the system. All user accounts were managed centrally by RHIO staff; the RHIO also maintained the community-wide master patient index. At the time of study, the web portal was not integrated into any organization’s EHR. The HIE system operates under an “opt-in” model where patients consent to have their information accessible. The system was fully operational by March 2009.1
This study was part of an evaluation of the HEAL NY program by the Health Information Technology Collaborative (HITEC), a consortium of four academic institutions charged with evaluating the effects of interoperable health information technology [17].
Data
This study is based on claims files from patients ≥18 years old who consented to allow at least one of the RHIO’s member organizations to view their data during 2009–2010 and who also were continuously enrolled in one of two participating health plans. These two plans cover over 60% of the area population. The RHIO provided a roster of consented patients to a private healthcare data aggregation and analytics company for matching against the claims files. We limited claims to patients who had had at least one encounter with a provider participating in the HIE system in the six months following the patient’s consent date.
Furthermore, we utilized two datasets associated with the HIE system. The RHIO provided us with the system log files documenting the use of the HIE system via the web portal. The RHIO also supplied a registry describing portal users’ job types and practice settings.
To collect data for a sensitivity analysis described below, we noted the physician associated with each ED claim, which was present for 92% of the ED encounters. When ED physician was missing, we used the inpatient physician, which occurred when hospitals submitted single claims for the combined ED encounter and inpatient stay. We chose to use the physician identified on the claim, rather than the physician who used the HIE system for two reasons: the physician was missing (by definition) when the HIE system was not accessed and, when the HIE system was accessed, the actual user could be a nurse or other staff member accessing the system on the physician’s behalf (without defined linkages to the physician of record in the ED). Using log data for some physician identification and claims data for other physician identification would have introduced information bias; thus, we consistently used the physician on the claim.
Measures
The outcome of interest was a hospital admission via the ED. The data aggregation and analytics company identified admissions via the ED through the claims files.
The primary independent variable was HIE system use at the time of the ED visit, measured in a yes/no fashion. To qualify as system use during the ED visit, records from the claims data and the user logs had to match on: patient identifiers, service dates, and user location [18, 19]. Additionally, since emergency visits might cross midnight, we also allowed system use on the following calendar day to match. Matching occurrences constituted usage; all other ED encounters were no usage.
We derived additional independent variables from the claims data. Patient demographics included gender, age and insurance status (commercial, Medicare managed care, or Medicaid managed care]. A small percentage of encounters (~5%) were covered by a state-subsidized product for low income individuals. We combined this product with Medicaid managed care. We measured patient disease severity as the count of Major Aggregated Diagnostic Groups (ADGs) in the 12 months prior to consent using the Johns Hopkins ACG Case-Mix System® [20, 21]. Since major ADGs are based are non-mutually exclusive groupings of diagnoses, we did not include diagnoses separately in our modeling. We also counted the number of hospitalizations during the six months prior to the patient’s consent.
Selection of cohort
► Figure 1 illustrates the selection of the cohort. We had claims files for 65% of patients >18 years old who had consented to have their data viewed by providers (n = 207,506). Of those, we included only individuals who had valid consent dates (n = 198,067). From this set, we retained patients who had ≥1 encounter with a provider registered to use the HIE system in the six months following their consent date. This ensured that each cohort member had a patient record. From this group, we identified all ED encounters and restricted the sample to only include each patient’s first ED visit (n = 15,645). Therefore, patients only appear in the analysis once. This restriction avoids the potential for differing effects on individual providers’ use of the system for repeat patients.
Fig. 1.
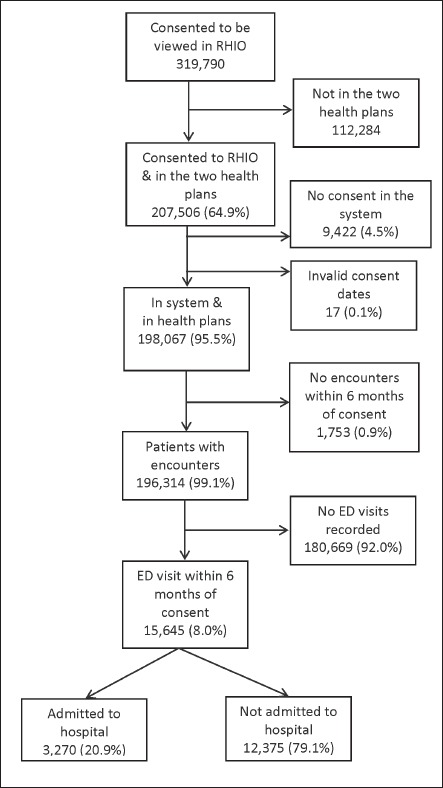
Patient selection and inclusion criteria.
Analysis
We compared the characteristics of patients for whom the HIE system was accessed to those for whom it was not accessed using the likelihood ratio χ2. We measured the association between system access and hospital admissions with logistic regression models. We set significance testing at ρ = 0.05. The full model adjusts for all independent variables with patient age, the count of major ADGs, and the number of prior hospitalizations treated as continuous variables.
To arrive at an estimate of potential cost savings, we estimated the number of potentially avoided admissions due to system usage. To calculate the number of expected admissions in the system usage group, we applied to that group the rate of admissions observed in the no usage group. The difference between the number of expected and actual admissions in the system usage group represented the number of admissions in our sample that were potentially avoided over the 6-month period. To assign a dollar value, we used the mean total costs among all 2010 New York state hospitalizations [22] and annualized the figures.
We performed four sensitivity analyses to explore the robustness of our findings. First, we created a more restrictive definition of system usage to explore whether our findings were a product of our usage definition. For this analysis, to qualify as system use during the ED visit, we required records from the claims data and the system usage logs to match all of the following: patient identifiers, user location, and same calendar date of service.
For our second sensitivity analysis, we included all ED encounters in our models. For the main analysis, each patient only had one encounter. For this analysis, we included both patients’ first as well as any subsequent encounters to make sure our selection of only the first ED visit did not bias our results. We applied the clustered sandwich estimator to the standard errors to account for the potential non-independence of observations [23].
Third, we performed several analyses to explore whether or not the findings were attributable to a single subgroup, such as the sickest or oldest patients. We also excluded patients with injury or pregnancy complication diagnoses since the HIE information may not be informative in these instances [19].
Finally, we conducted a sensitivity analysis to confirm that our findings were not due to physician effects. That is, we sought to confirm that a given physician might access the HIE for some patients, but not for others, a pattern which would be clinically appropriate. If confirmed, this would decrease the likelihood that the results were due to physician-level confounding, because the same physicians would be contributing patients to both the intervention and the control groups.
We performed all analyses using Stata 12.1 (StataCorp, College Station, TX).
Results
Of the 319,790 consented adult patients in the Rochester RHIO, 196,314 (61.3%) met our inclusion criteria regarding health plan participation, continuous enrollment and data within the HIE system. From these patients, we identified a cohort of 15,645 patients with an ED visit within 6 months of their consent date (►Figure 1). The HIE system was accessed for 2.4% of the ED visits (n = 374) in the cohort with the remaining 15,217 without HIE system access. This usage rate is consistent with comparable systems in other communities [12, 19, 24–26].
▶ Table 1 displays the sample characteristics stratified by system access. The majority of patients were female (66.8%), one-third were greater than 65 years old and nearly half had private insurance (46.9%). Nearly, 40% of patients had no major ADGs and the majority (87.5%) had not been hospitalized in the previous year. Those with and those without system access differed significantly in several areas. Those for whom the system was accessed were more likely to have private insurance (54.5% vs. 46.9%, p<0.01), had a higher percentage of encounters without any major ADGs (42.3% vs. 40.0%, p<0.01), and had fewer previous inpatient admissions (92.0% vs. 87.5%, p<0.05).
Table 1.
Characteristics of patients who consented to participate in a health information exchange system and who presented for an emergency department visit stratified by whether providers accessed their clinical data in the system or nota
| Encounter characteristics |
Totals | System accessed | No system access | p-valueb |
|---|---|---|---|---|
| n = 15,645 (%) | n = 374 (%) | n = 15,271 (%) | ||
| Admitted to hospital | 3270 (20.90) | 58 (15.51) | 3212 (21.03) | 0.009 |
| Gender | ||||
| Male | 5188 (33.16) | 128 (34.22) | 5060 (33.13) | 0.66 |
| Female | 10457 (66.84) | 246 (65.78) | 10211 (66.87) | |
| Age | ||||
| 18–34 | 3604 (23.04) | 90 (24.06) | 3514 (23.01) | 0.96 |
| 35–44 | 1969 (12.59) | 45 (12.03) | 1924 (12.60) | |
| 45–64 | 4344 (27.77) | 103 (27.54) | 4241 (27.77) | |
| ≥65 | 5728 (36.61) | 136 (36.36) | 5592 (36.62) | |
| Insurance | ||||
| Private | 7344 (46.94) | 204 (54.55) | 7140 (46.76) | 0.005 |
| Medicaid | 3804 (24.31) | 69 (18.45) | 3735 (24.46) | |
| Medicare | 4497 (28.74) | 101 (27.01) | 4396 (28.79) | |
| Major ADG count | ||||
| 0 | 6251 (39.96) | 158 (42.25) | 6093 (39.90) | 0.005 |
| 1 | 3913 (25.01) | 114 (30.48) | 3799 (24.88) | |
| 2 | 2662 (17.02) | 56 (14.97) | 2606 (17.07) | |
| ≥3 | 2819 (18.02) | 46 (12.30) | 2773 (18.16) | |
| No. inpatient hospitalizations | ||||
| 0 | 13683 (87.46) | 344 (91.98) | 13339 (87.35) | 0.02 |
| 1–2 | 1781 (11.38) | 26 (6.95) | 1755 (11.49) | |
| ≥3 | 181 (1.16) | 4 (1.07) | 177 (1.16) | |
aRochester RHIO during 2009–2010
bcomparing patients with system access and encounters without access
The dataset included ED encounters with 229 different physicians. Of the 229 physicians, 16 (7%) used the HIE system. Of those 16 users, 15 used the HIE system for some but not all of their patients in the study. Thus, the physicians who were users contributed data to both the intervention group and the control group.
In the study, 20.9% (n = 3,270) were admitted to the hospital and 79.1% (n = 15,645) were not admitted. For patients with system access during their ED encounter, 15.5% were subsequently admitted to the hospital (n = 58). In contrast, a higher percentage (21.0%, p<0.01) of patients for whom the system was not accessed were admitted.
As illustrated in ▶ Table 2, the unadjusted odds of being admitted to the hospital were 31% lower when the HIE system was accessed compared to when it was not accessed. After controlling for patient characteristics, the odds a patient was admitted to the hospital when the HIE system was accessed were still significantly lower (aOR = 0.70; 95%CI = 0.52, 0.95). Additionally in the multivariate model, male patients, older patients, patients with increasing disease severity, and those that had been hospitalized previously all had higher odds of admission. In terms of insurance, the odds of admission were lower for those covered by Medicaid managed care and the odds were higher for those covered by Medicare managed care.
Table 2.
Unadjusted and adjusted associations between usage of health information exchange system at the time of the emergency department visit and admission to the hospital.
| Unadjusted odds ratio (95%CI)a |
Adjusted odds ratio (95%CI) |
|
|---|---|---|
| System access | 0.69 (0.52, 0.91)** | 0.70 (0.52, 0.95)* |
| Male | 1.76 (1.63, 1.91)*** | 1.47 (1.35, 1.60)*** |
| Age | 1.05 (1.04, 1.05)*** | 1.03 (1.03, 1.03)*** |
| Insurance | ||
| • Private | Reference | Reference |
| • Medicaid / safety-net | 0.37 (0.32, 0.43)*** | 0.61 (0.52, 0.72)*** |
| • Medicare | 4.13 (3.78, 4.51)*** | 2.02 (1.82, 2.25)*** |
| Major ADG count | 1.40 (1.37, 1.44)*** | 1.04 (1.01, 1.08)** |
| No of prior hospitalizationsb | 1.78 (1.67, 1.90)*** | 1.46 (1.37, 1.57)*** |
a95% confidence interval;
bUtilization in the six months prior
*p<0.05;
**p<0.01;
***p<0.001
The potential annual savings in avoided admission costs associated with usage of the HIE system in this sample was $357,552 (95%CI = $139,048, 556,192).
Sensitivity analyses
The results of the sensitivity analyses (▶ Table 3) were generally consistent with the main analysis. First, when limiting the definition of system usage to the same calendar day, the odds of an admission were lower (OR = 0.83; 95%CI = 0.55, 1.25), but not statistically significant. The direction and magnitude of the effect were similar to the full sample results. The lack of significance is partly attributable to the decrease in the number of cases and decrease in statistical power. With this definition 1.2% of encounters were accessed, but this same calendar day criterion is probably too restrictive as it excludes possible access during late night visits. Our second sensitivity analysis allowed for patients to have multiple visits. Adjusted for confounding, system access was still negatively and significantly associated with admissions (aOR = 0.69; 95%CI = 0.53, 0.90). Third, the stratified analyses were also consistent with the main findings, although not always statistically significant. Finally, when we restricted the analysis to only those physicians who used the HIE system for some but not all of their patients, thereby minimizing physician variability, HIE usage was still negatively associated with the odds of admission (aOR = 0.46; 95%CI = 0.34, 0.62).
Table 3.
Unadjusted and adjusted associations between usage of health information exchange system at the time of the emergency department visit and admission to the hospital.
| Sample size | System access % |
OR & 95%CI1 | |
|---|---|---|---|
| Matching criterion changes | |||
| Usage limited to same calendar day as ED encounter | 15645 | 1.2 | 0.83 (0.55, 1.25) |
| Sample definition | |||
| Multiple encounters per patient included in analysis | 24543 | 2.2 | 0.69 (0.53, 0.90) |
| Stratified analyses | |||
| ≥ 65 | 5728 | 2.4 | 0.72 (0.49, 1.06) |
| <65 | 9917 | 2.4 | 0.62 (0.37, 1.02) |
| ≥ 3 major ADGs | 2819 | 1.6 | 0.83 (0.42, 1.63) |
| < 3 major ADGs | 12826 | 2.6 | 0.67 (0.48, 0.94) |
| ≥ 1 prior hospitalizations | 1962 | 1.5 | 1.02 (0.47, 2.26) |
| No prior hospitalizations | 13683 | 2.5 | 0.66 (0.47, 0.92) |
| Excluded encounters with injury or pregnancy complication diagnoses | 12409 | 2.5 | 0.70 (0.51, 0.95) |
| Limited to only providers that used HIE | 8670 | 4.5 | 0.46 (0.34, 0.62) |
Discussion
Among patients who presented to the ED, the rate of hospitalization was lower for those patients who had their information accessed from an HIE system compared to those who did not. Controlling for patient characteristics, the odds of patient’s admission were 30% lower when the system was accessed. Use in the ED of an HIE system was associated with a conservatively estimated annual savings of nearly $357,000.
Conceptually, there are many potential mechanisms by which access to an HIE system at the point of care could have helped avoid hospitalization including: accessing additional patient history or prior laboratory result, revealing a contraindication to a medication, or identifying prior care providers to contact for further information [27]. That type of information has previously been unavailable or difficult to obtain in settings dealing with unplanned and urgent care delivery. Our analysis suggests that access to such information is correlated with a reduction of the odds of admission; however, elucidating the specific decision pathway requires future investigation with alternative study designs. From the existing literature, we know that different providers have varying information needs [5], users access HIE systems in different ways [28], and HIE usage varies between organizations [29]. We suspect the mechanisms underlying any one admission decision are likely to be patient-, context- and provider-specific.
This study also contributes to the broader literature that explores which interventions are effective for decreasing potentially avoidable hospitalizations. Previous work has explored the effectiveness of strategies like disease management [30], medication review [31], and telehealth [32]. All of these strategies are targeted at the ambulatory setting, and by the time patients arrive in an ED, these strategies are no longer applicable. This study describes a community-based HIE system that can be used in the ED and provides clinical information that could affect the decision to admit a patient or discharge them home from the ED.
To date, the existing literature on the effectiveness of HIE systems for changing utilization has been mixed [9]. Earlier studies that found no effect between HIE and utilization tended to face limitations in terms of the number of participating providers, number of information sources, or included populationsn [11–13] Our findings are consistent with the recent results from the MidSouth eHealth Alliance, but the effect size in our study was slightly smaller. Like Rochester RHIO, the Mid-South eHealth Alliance contains a broad array of providers and end users access data through a stand-alone, web-based portal [33]. In addition to both exchanges receiving state funding, both the Memphis area and Rochester have a long history of attempting innovative healthcare system reforms [24].
A strength of our analytic approach is the reliance on objective measures of HIE usage. Our focus on actual usage at the point of care, in this case an ED encounter, removes the limitations posed by self-reported usage or use of organizational adoption as a proxy for actual usage. It is worth noting that several HIE studies which measure actual system usage have found positive effects [33–35], whereas those that look at organizational level adoption only, have not [36–39].
Additionally, these findings illustrate a challenge facing policy makers, practitioners and organizational leaders with using health information technology (HIT) to transform healthcare. This study suggests that technology interventions may be able to live up to their touted ability to change care, but overall the system was not used very often. Integrating useful tools into clinical work is challenging as providers encounter numerous attention and workflow barriers to using additional HIT [40]. If HIT proves useful to clinical decision making, it is the responsibility of the healthcare organizations to ensure system use is a well-integrated part of care. With more widespread usage, we would expect potentially greater financial savings.
This study has several limitations. First, we describe associations between HIE use and admissions, but cannot determine causality. Primarily, we cannot prove that the data in the HIE system factored into the admission decision, because we do not have detailed data on medical decision making. However, interviews with ED physicians in the RHIO indicate physicians will access historical information to help establish baselines and confirm their decisions around patient admission. Relatedly, there is a potential for error in measuring temporal sequence. Again, however, discussion with ED physicians and other users suggest that the HIE system is not consulted once the patient has been admitted. Second, we were unable to determine the clinical appropriateness of any given decision to admit or to discharge. Determinations of appropriateness are beyond the scope of this present study and our secondary datasets. However, a future line of inquiry could assess the outcomes for both patients admitted as well as those that were not admitted. Third, the decision to use HIE systems is not completely random, but influenced by patient, user, and workplace factors [19, 25, 29] Therefore, factors not captured in our claims datasets at the provider and patient level may be confounding the relationship between HIE access and admission status. It is possible that the users of HIE are very different than non-users. That is why we undertook the sensitivity analysis of restricting the sample to only the users of HIE. Again the results persisted, suggesting that among this potential more uniform of group of HIE adopters the system may be beneficial. Fourth, this study examined a single HIE system in a single community, which may limit the generalizability to different areas or technologies; however, the community-based setting also maximizes generalizability, as it expands the evidence about HIE beyond academic medical centers and integrated delivery systems [41]. Finally, our estimated of cost savings are based solely on the average cost of the potentially avoided admissions and does not consider any other potential patients costs nor the costs associated with establishing and operating the RHIO.
Despite these limitations, this study has important policy implications given the substantial financial investment in interventions designed to improve provider access to patient information. The most notable investment is the federal government’s Meaningful Use program established under the Health Information Technology for Economic and Clinical Health (HITECH) Act. This $27 billion program offers incentives for the adoption and use of electronic health record systems (EHRs) with the capability to exchange information with other entities [42]. The recently released Stage 2 criteria are focused on robust use of electronic exchange [43]. Additionally, the federal government is also funding state-based exchange efforts to improve information availability. States also have contributed to the further adoption of interoperable HIT [44]. Furthermore, the emerging popularity of organizational restructuring of healthcare through Patient Centered Medical Homes and Accountable Care Organizations is predicated on broad access to clinical information. The findings of this study support the current policy goals of improving provider access to patient information via HIT.
Usage of a community-wide HIE system was associated with a 30% lower odds of hospital admission among patients who come to the ED. This study provides important new evidence on the potential of community-wide longitudinal patient information systems to decrease the utilization of expensive healthcare services. This finding is particularly notable due to its’ community-based setting, which may increase the generalizability.
Acknowledgments
The project was funded by the New York State Department of Health Evaluation of the Healthcare Efficiency and Affordability Law for New Yorkers Program (HEAL NY) – Phase 5 (Contract #C023699) and by the Commonwealth Fund. The authors wish to thank the Rochester Regional Health Information Organization for requesting this evaluation and providing access to data. We also thank Ted Kremer, MPH, Jill Eisenstein, MS, Gloria Hitchcock, MS, Sarah Abrams, MPH, Vaishali Patel, PhD, and Alison Edwards, MS for their assistance with this project. The authors had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Footnotes
Clinical Relevance
Relevant and timely patient information can be difficult to obtain in emergency department settings. Health information exchange (HIE) can make patient information more accessible to providers at the point of care. This study suggests HIE may be able to change healthcare utilization and help save money.
Conflict Of Interest
The authors have no conflict of interest to declare.
Human Subjects Protections
The Institutional Review Boards of Weill Cornell Medical College and the University of Rochester approved the study protocol.
1 More information about system functionality and capability is available at www.grrhio.org.
References
- 1.Stiell A, Forster AJ, Stiell IG, van Walraven C.Prevalence of information gaps in the emergency department and the effect on patient outcomes. Canadian Medical Association Journal 2003; 169(10): 1023–1028 [PMC free article] [PubMed] [Google Scholar]
- 2.Remen VM, Grimsmo A.Closing information gaps with shared electronic patient summaries–How much will it matter? International Journal of Medical Informatics 2011; 80(11): 775–781 [DOI] [PubMed] [Google Scholar]
- 3.Levit K, Stranges E, Ryan K, Elixhauser A.HCUP Facts and Figures, 2006: Statistics on Hospital-based Care in the United States. Agency for Healthcare Research & Quality; 2008; Available from:http://www.hcup-us.ahrq.gov/reports/factsandfigures/facts_figures_2006.jsp [PubMed] [Google Scholar]
- 4.Owens P, Elixhauser A.Hospital Admissions That Began in the Emergency Department, 2003. Agency for Healthcare Research and Quality, 2006 [PubMed] [Google Scholar]
- 5.Shapiro JS, Kannry J, Kushniruk AW, Kuperman G.The New York Clinical Information Exchange Clinical Advisory S. Emergency Physicians’ Perceptions of Health Information Exchange. J Am Med Inform Assoc 2007; 14(6): 700–705 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Shapiro JS, Kannry J, Lipton M, Goldberg E, Conocenti P, Stuard S, Wyatt BM, Kuperman G.Approaches to patient health information exchange and their impact on emergency medicine. Annals of Emergency Medicine 2006; 48(4): 426–432 PubMed PMID: ISI:000240886200013 [DOI] [PubMed] [Google Scholar]
- 7.Finnell JT, Overhage JM, Dexter PR, Perkins SM, Lane KA, McDonald CJ.Community clinical data exchange for emergency medicine patients. AMIA Annu Symp Proc 2003: 235–238 PubMed PMID: 14728169 [PMC free article] [PubMed] [Google Scholar]
- 8.Frisse ME, Holmes RL.Estimated financial savings associated with health information exchange and ambulatory care referral. Journal of Biomedical Informatics 2007; 40(6 S1): S27–S32 [DOI] [PubMed] [Google Scholar]
- 9.Hincapie A, Warholak T.The Impact of Health Information Exchange on Health Outcomes. Applied Clinical Informatics 2011; 2(4): 499–507 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ben-Assuli O, Shabtai I, Leshno M.The impact of EHR and HIE on reducing avoidable admissions: controlling main differential diagnoses. BMC Med Inform Decis Mak 2013; 13(1): 49 PubMed PMID: doi:10.1186/1472–6947–13–49 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lang E, Afilalo M, Vandal AC, Boivin JF, Xue X, Colacone A, Leger R, Shrier I, Rosenthal S.Impact of an electronic link between the emergency department and family physicians: a randomized controlled trial. Cmaj 2006; 174(3): 313–318 PubMed PMID: 16399880 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Overhage J, Deter P, Perkins S, Cordell W, McGoff J, McGrath R.A randomized, controlled trial of clinical information shared from another institution. Ann Emerg Med 2002; 39(1): 14–23 [DOI] [PubMed] [Google Scholar]
- 13.Vest JR.Health information exchange and healthcare utilization. Journal of Medical Systems 2009; 33(3): 223–231 [DOI] [PubMed] [Google Scholar]
- 14.Greater Rochester Regional Health Information Organization About Rochester RHIO. 2009; Available from:http://www.grrhio.org/about/default.aspx [Google Scholar]
- 15.Greater Rochester Regional Health Information Organization The Virtual Health Record links you to clinical reports, medication histories, radiology images and more from across the region. Rochester, NY2010; Available from:http://www.grrhio.org/providers/~/media/VHR%20Insert.ashx [Google Scholar]
- 16.Campion TR, Jr, Edwards AM, Johnson SB, Kaushal R.Health information exchange system usage patterns in three communities: Practice sites, users, patients, and data. International Journal of Medical Informatics 2013; 82(9): 810–820 [DOI] [PubMed] [Google Scholar]
- 17.Kern LM, Kaushal R.Health information technology and health information exchange in New York State: New initiatives in implementation and evaluation. Journal of Biomedical Informatics 2007; 40(6, Supplement): S17–S20 [DOI] [PubMed] [Google Scholar]
- 18.Vest JR, Jasperson J, Zhao H, Gamm L, Ohsfeldt R.Use of a health information exchange system in the emergency care of children. BMC Med Inform Decis Mak 2011; 11(1): 78 PubMed PMID: doi:10.1186/1472-6947–11-78 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Vest JR, Zhao H, Jasperson J, Gamm LD, Ohsfeldt RL.Factors motivating and affecting health information exchange usage. Journal of the American Medical Informatics Association 2011; 18(2): 143–149 Pubmed Central PMCID: 21262919 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.The Health Services Research & Development Center at The Johns Hopkins University, Bloomberg School of Public Health The Johns Hopkins ACG® System: Technical Reference Guide Version 10.0. Baltimore, MD: 2011 [Google Scholar]
- 21.Baldwin LM, Klabunde CN, Green P, Barlow W, Wright G.In search of the perfect comorbidity measure for use with administrative claims data: does it exist? Med Care 2006; 44(8): 745–753 PubMed PMID: 16862036. Pubmed Central PMCID: 3124350. Epub 2006/07/25. eng [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Agency for Healthcare Research Quality. HCUPnet: Information on stays in hospitals for participating States from the HCUP State Inpatient Databases (SID) Rockville, MD: US Department of Health & Human Services; 2012[15 Aug 2012]; Available from:http://hcupnet.ahrq.gov/ [Google Scholar]
- 23.Long JS, Freese J.Regession Models for Categorical Dependent Varaibles Using Stata. 2nd ed College Station, TX: Stata Press; 2006 [Google Scholar]
- 24.Johnson KB, Gadd C, Aronsky D, Yang K, Tang L, Estrin V, King JK, Frisse ME.The MidSouth eHealth Alliance: Use and Impact In the First Year. AMIA Annu Symp Proc 2008: 333–337 PubMed PMID: 18999184. Epub 2008/11/13. eng [PMC free article] [PubMed] [Google Scholar]
- 25.Johnson KB, Unertl KM, Chen Q, Lorenzi NM, Nian H, Bailey J, Frisse ME.Health information exchange usage in emergency departments and clinics: the who, what, and why. Journal of the American Medical Informatics Association 2011; 18(5): 690–697 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hripcsak G, Sengupta S, Wilcox A, Green RA.Emergency department access to a longitudinal medical record. J Am Med Inform Assoc 2007; 14(2): 235–238 PubMed PMID: 17213496. Epub 2007/01/11. eng [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hripcsak G, Kaushal R, Johnson KB, Ash JS, Bates DW, Block R, Frisse ME, Kern LM, Marchibroda J, Overhage J, Wilcox AB.The United Hospital Fund meeting on evaluating health information exchange. Journal of Biomedical Informatics 2007; 40(6 S1): S3-S10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Vest JR, Jasperson J.How are health professionals using health information exchange systems? Measuring usage for evaluation and system improvement. Journal of Medical Systems 2012; 36(5): 3195–3204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Vest JR, Gamm L, Ohsfeldt R, Zhao H, Jasperson J.Factors Associated with Health Information Exchange System Usage in a Safety-Net Ambulatory Care Clinic Setting. Journal of Medical Systems 2011: 1–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Peytremann-Bridevaux I, Staeger P, Bridevaux P-O, Ghali WA, Burnand B.Effectiveness of Chronic Obstructive Pulmonary Disease-Management Programs: Systematic Review and Meta-Analysis. The American Journal of Medicine 2008; 121(5): 433–443e4 [DOI] [PubMed] [Google Scholar]
- 31.Royal S, Smeaton L, Avery AJ, Hurwitz B, Sheikh A.Interventions in primary care to reduce medication related adverse events and hospital admissions: systematic review and meta-analysis. Quality and Safety in Health Care 2006; 15(1): 23–31 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Inglis SC, Clark RA, McAlister FA, Ball J, Lewinter C, Cullington D, Stewart S, Cleland JG.Structured telephone support or telemonitoring programmes for patients with chronic heart failure. The Cochrane database of systematic reviews 2010. (8): CD007228 PubMed PMID: 20687083. Epub 2010/08/06. eng [DOI] [PubMed] [Google Scholar]
- 33.Frisse ME, Johnson KB, Nian H, Davison CL, Gadd CS, Unertl KM, Turri PA, Chen Q.The financial impact of health information exchange on emergency department care. J Am Med Inform Assoc 2012; 19(3): 328–333 PubMed PMID: 22058169. Epub 2011/11/08. Eng [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bailey JE, Pope RA, Elliott EC, Wan JY, Waters TM, Frisse ME.Health Information Exchange Reduces Repeated Diagnostic Imaging for Back Pain. Ann Emerg Med 2013. PubMed PMID: 23465552. Epub 2013/03/08 [DOI] [PubMed] [Google Scholar]
- 35.Bailey JE, Wan JY, Mabry LM, Landy SH, Pope RA, Waters TM, Frisse ME. Does Health Information Exchange Reduce Unnecessary Neuroimaging and Improve Quality of Headache Care in the Emergency Department? J Gen Intern Med. 2012 doi: 10.1007/s11606-012-2092-7. Epub 2012/06/01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Selck F, Decker S.Health Information Technology in the Emergency Department. AcademyHealth Annual Research Meeting; June 23–25; Baltimore, MD2013 [Google Scholar]
- 37.McCormick D, Bor DH, Woolhandler S, Himmelstein DU.Giving Office-Based Physicians Electronic Access To Patients’ Prior Imaging And Lab Results Did Not Deter Ordering Of Tests. Health Affairs 2012; 31(3): 488–496 [DOI] [PubMed] [Google Scholar]
- 38.Ross SE, Radcliff TA, LeBlanc WG, Dickinson LM, Libby AM, Nease DE.Effects of health information exchange adoption on ambulatory testing rates. Journal of the American Medical Informatics Association 2013 May 22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Jones SS, Friedberg MW, Schneider EC.Health information exchange, Health Information Technology use, and hospital readmission rates. AMIA Annu Symp Proc 2011; 2011: 644–653 PubMed PMID: 22195120. Pubmed Central PMCID: 3243133. Epub 2011/12/24. eng [PMC free article] [PubMed] [Google Scholar]
- 40.Lluch M.Healthcare professionals’ organisational barriers to health information technologies—A literature review. International Journal of Medical Informatics 2011; 80(12): 849–862 [DOI] [PubMed] [Google Scholar]
- 41.eHealth Initiative The State of Health Information Exchange in 2010: Connecting the Nation to Achieve Meaningful Use. Washington, DC: 2010 [Google Scholar]
- 42.Department of Health & Human Services 42 CFR Parts 412, 413, 422 et al. Medicare and Medicaid Programs; Electronic Health Record Incentive Program; Final Rule. Federal Register 2010; 75(144): 44314–44588 [PubMed] [Google Scholar]
- 43.Department of Health & Human Services, Center for Medicare & Medicaid Services Medicare and Medicaid Programs; Electronic Health Record Incentive Program – Stage 2. 2012[6 Sept 2012]; Available from:http://www.ofr.gov/%28X%281%29S%28uzclbwrx5fwqm2w2mipkysrh%29%29/OFRUpload/OFRData/2012-21050_PI.pdf [Google Scholar]
- 44.Kern LM, Barron Y, Abramson EL, Patel V, Kaushal R.HEAL NY: Promoting interoperable health information technology in New York State. Health Affairs 2009; 28(2): 493–504 PubMed PMID: 19276009. Epub 2009/03/12. eng [DOI] [PubMed] [Google Scholar]


