Abstract
Pancreato-biliary malignancies often present with locally advanced or metastatic disease. Surgery is the mainstay of treatment although less than 20% of tumours are suitable for resection at presentation. Common sites for metastases are liver, lungs, lymph nodes and peritoneal cavity. Metastatic disease carries poor prognosis, with median survival of less than 3 mo. We report two cases where metastases from pancreato-biliary cancers were identified in the colon and anal canal. In both cases specific immunohistochemical staining was utilised in the diagnosis. In the first case, the presenting complaint was obstructive jaundice due to an ampullary tumour for which a pancreato-duodenectomy was carried out. However, the patient re-presented 4 wk later with an atypical anal fissure which was found to be metastatic deposit from the primary ampullary adenocarcinoma. In the second case, the patient presented with obstructive jaundice due to a biliary stricture. Subsequent imaging revealed sigmoid thickening, which was confirmed to be a metastatic deposit. Distal colonic and anorectal metastases from pancreato-biliary cancers are rare and can masquerade as primary colorectal tumours. The key to the diagnosis is the specific immunohistochemical profile of the intestinal lesion biopsies.
Keywords: Pancreatobiliary cancer, Rare metastatic sites, Colonic metastasis, Anal metastasis, Immunohistochemistry
Core tip: Pancreato-biliary malignancies often present with locally advanced or metastatic disease. Surgery is the mainstay of treatment although less than 20% are suitable for resection at presentation. Common sites for metastases are liver, lungs, lymph nodes and peritoneal cavity and carry poor prognosis, with median survival of less than 3 mo. Distal colonic and anorectal metastases from pancreato-biliary cancers are rare and can masquerade as primary colorectal tumours. The key to the diagnosis is the specific immunohistochemical profile of the intestinal lesion biopsies.
INTRODUCTION
Pancreato-biliary malignancies often present with locally advanced or metastatic disease[1,2]. The commonest tumour type is adenocarcinoma followed by rarer varieties such as neuroendocrine and adeno-squamous cell carcinomas[3-5]. Surgery is the mainstay of treatment although less than 20% are deemed resectable at the time of presentation[1,5-8]. Metastatic disease carries a poor prognosis with median survival of less than 3 mo[5-12].
The common sites for metastases are the liver, lungs, lymph nodes and peritoneal cavity[2]. Unusual metastatic sites such as kidney[13], colon[14-17] and skin[18], have also been reported. We report two cases where metastases from pancreato-biliary cancers were identified in the colon and anal canal.
CASE REPORT
Case 1
A 79-year-old lady presented with obstructive jaundice. A computed tomography (CT) scan and a subsequent endoscopic ultrasound scan identified a resectable ampullary mass. Staging CT did not reveal any evidence of metastases and the patient underwent a Whipple’s resection following which she made an uncomplicated recovery. The histopathology of the resected specimen confirmed poorly differentiated ampullary adenocarcinoma. The tumour demonstrated a pancreato-bilary immunophenotype being cytokeratin-7/cytokeratin-17/mucin-1 (CK7/CK17/MUC1) positive and cytokeratin-20/homeobox protein CDX2/mucin-2 (CK20/CDX2/MUC2) negative (Figure 1A). Approximately 4 wk after discharge, the patient re-presented with perianal pain exacerbated by defecation. Examination under anaesthesia (EUA) confirmed the presence of an atypical anal fissure, biopsies of which revealed anal mucosa extensively infiltrated by a poorly differentiated carcinoma, demonstrating similar morphological appearance to the original ampullary adenocarcinoma. Subsequent, immunohistochemistry also demonstrated an identical pancreato-biliary phenotype as seen previously (Figure 1B), suggesting that this was a metastatic deposit from the ampullary cancer. The patient underwent two cycles of palliative radiotherapy to the anal canal for control of pain and was discharged with full palliative support. She died approximately 3 wk after discharge.
Figure 1.
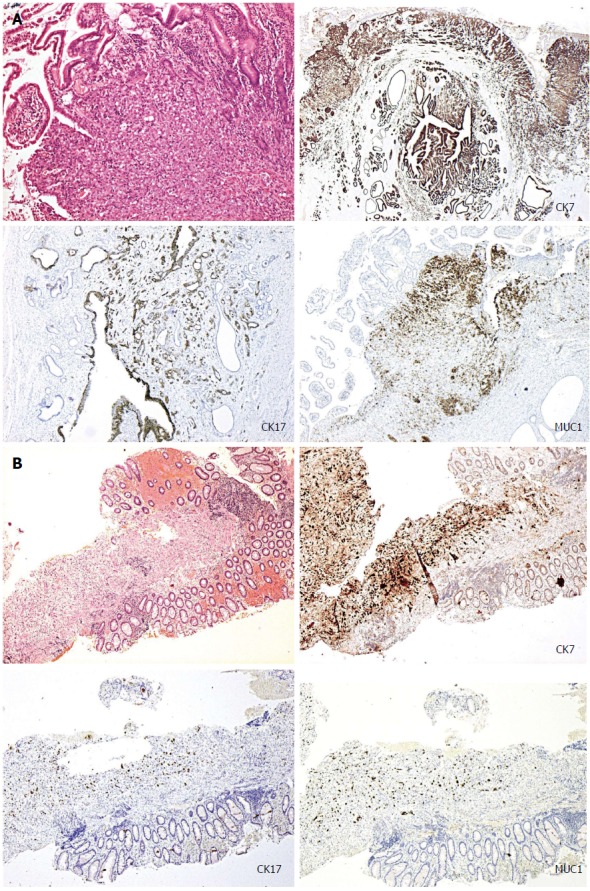
Immunohistochemical staining. A: Immunohistochemical staining of the surgical specimen demonstrating pancreato-biliary phenotype: cytokeratin-7/cytokeratin-17/mucin-1 (CK7/CK17/MUC1) positive and cytokeratin-20/homeobox protein CDX2/mucin-2 (CK20/CDX2/MUC2) negative; B: Immunohistochemical staining of the anal fissure biopsy demonstrating pancreato-biliary phenotype similar to the ampullary adenocarcinoma.
Case 2
A 63-year-old lady presented with obstructive jaundice due to a biliary stricture involving the hilum of the bile ducts and extending longitudinally into the distal common bile duct. Endoscopic retrograde cholangiopancreatographic brushings were inconclusive. She underwent further staging with a CT scan and laparoscopy. The laparoscopy showed no evidence of peritoneal disease, however the CT scan revealed thickening of the sigmoid colon. Colonoscopic biopsies confirmed a submucosal infiltrating moderately differentiated adenocarcinoma with no associated mucosal dysplasia. This was not supportive of a colorectal primary and favoured an extrinsic origin. Subsequent immunohistochemical analysis showed strong staining for CK7, with occasional positive staining for CK20; and negative CDX2, CK17 and Estrogen Receptor (ER) immunoreactivity. This profile, although not specific, was consistent with metastatic deposit from a hilar cholagiocarcinoma. She underwent palliative biliary stenting and was referred for palliative chemotherapy.
DISCUSSION
The colon, rectum and anal canal are rare sites for metastases for any type of malignancy. However, such cases have been reported from primary carcinomas of breast[19-22], lung[23,24], colon[25,26] and prostate[27]. Additionally, a small number of such metastases have been reported to occur in relation to cholangiocarcinomas[14,15] and pancreatic adenocarcinomas[13,16,17]. To the best of our knowledge metastasis to the anal canal from pancreato-biliary malignancies has not been reported before in the literature.
The extrinsic nature of these metastatic deposits may not be apparent in superficial mucosal biopsies. Immunohistochemical studies may be warranted in such cases where there is a suspicion of metastases or if there are unusual features such as adenocarcinoma undermining an intact, non-dysplastic mucosal surface. In the two cases that we have presented (Table 1) the immunohistochemical profiles of the tumours were more consistent with pancreato-bilary origin than lower gastrointestinal tract origin although are not definitive and final diagnosis requires correlation with the clinical and radiological parameters. Ampullary adenocarcinomas can demonstrate either an intestinal (CK20/CDX2/MUC2 positive) or pancreaticobilary immunophenotype (CK7/CK17/MUC1 positive)[28-31], as in case 1. The tumours demonstrating a pancreato-bilary phenotype can also co-express CK20, but this is usually only focal in distribution. On the contrary, the vast majority of colorectal adenocarcinomas demonstrate a typical lower gastrointestinal immunophenotype, being CK20 and CDX2 positive (CDX2 is an intestine-specific nuclear transcription factor, which can be used as a marker for intestinal-type differentiation of colorectal adenocarcinomas)[29,30].
Table 1.
Summarising characteristics of the 2 cases
| Demographic information | Mode of presentation | Initial investigations and findings | Site of primary lesion | Site of metastases | Histology of metastasis | Outcome |
| 79, female | Presented with obstructive jaundice | EUS, CT, ERCP, tissue diagnosis obtained after Whipple resection | Ampullary | Anal canal | Adeno carcinoma, PB type. CK7/CK17/MUC1 positive, (negative for K20/CDX2/MUC2) | Palliation |
| 63, female | Presented with obstructive jaundice | Colonoscopy and biopsy, staging CT | Hilum of bile ducts | Sigmoid colon | Microscopy Immunohistochemistry strong CK7 staining, with occasional positive staining for CK20; (negative CDX2, CK17 and ER immunoreactivity) | Palliative percutaneous biliary stenting and chemotherapy |
CT: Computed tomography; EUS: Endoscopic ultrasound scan; ERCP: Endoscopic retrograde cholangiopancreatography.
We acknowledge that we do not have direct corroborative histology of the pancreato-biliary primary in the second case. However, unequivocal evidence of a locally advanced malignant pancreatic mass noted on staging CT. Pancreatic biopsy was not attempted due to poor performance status of the patient. In this case there was sufficient radiological and immunohistochemical evidence to support the diagnosis of metastatic deposit in the large intestine from the primary biliary cancer.
Although pancreato-biliary malignancies commonly lead to metastatic deposits on the peritoneal surfaces, the cases described here did not have any evidence of diffuse peritoneal involvement. There was no evidence of peritoneal nodules, omental infiltration or ascites on any of the CT scans or staging laparoscopy. Therefore we believe that these are focal metastases to the colon and anal canal rather than a part of diffuse peritoneal involvement.
Distal colonic and anorectal metastases are rare. They may present simultaneously with or in isolation from the primary, with symptoms identical to a primary colo-rectal tumour. The key to diagnosis is a high index of suspicion if the clinical picture is atypical coupled with specific immunohistochemical staining. Atypical immunohistochemical pattern that does not fit with a colorectal primary should raise suspicion regarding metastases from an extrinsic source.
COMMENTS
Case characteristics
Case 1, a 79-year-old lady presented with peri-anal pain approximately 4 wk after discharge following a Whipple's procedure for an ampullary mass; case 2, a 63-year-old lady presented with obstructive jaundice.
Clinical diagnosis
Perianal pain, with an atypical anal fissure on examination under anaesthesia; obstructive jaundice, nil else.
Differential diagnosis
Benign anal fissure, anal cancer, metastatic disease; gallstone disease, benign biliary stricture, pancreatic cancer, cholangiocarcinoma, ampullary cancer, metastatic disease from unknown primary.
Laboratory diagnosis
Nortmal blood indices; liver function tests of obstructive picture.
Imaging diagnosis
Not applicable; endoscopic retrograde cholangiopancreatographic showed a proximal biliary stricture and staging computed tomography scan revealed thickening of the sigmoid colon.
Pathological diagnosis
Histopathological analysis revealed anal mucosa extensively infiltrated by a poorly differentiated carcinoma, demonstrating similar morphological appearance to the original ampullary adenocarcinoma [cytokeratin-7/cytokeratin-17/mucin-1 (CK7/CK17/MUC1) positive CK20/CDX2/MUC2 negative]; colonoscopic biopsies confirmed a submucosal infiltrating moderately differentiated adenocarcinoma with strong positivity for CK7, occasional positive staining for CK20 and negative CDX2, CK17 and ER immunoreactivity, profile consistent with metastatic deposit from a hilar cholagiocarcinoma.
Treatment
Palliative chemoradiotherapy; palliative palliative biliary stenting and chemotherapy.
Related reports
Metastases of pancreatobiliary malignancies to the colon are extremely rare and metastasis to the anal canal has not been reported before in the literature to the best of our knowledge.
Term explanation
Immunohistochemistry is refers to the process of detecting antigens (e.g., proteins) in cells of a tissue section by exploiting the principle of antibodies binding specifically to antigens in biological tissues.
Experiences and lessons
Symptoms from distal colonic and anorectal metastases may be identical to a primary colorectal tumour and the key to diagnosis is a high index of suspicion if the clinical picture is atypical coupled with specific immunohistochemical staining.
Peer review
This is a report of two unusual metastases of pancreato-biliary malignancies to the sigmoid colon and anal canal. The cases stress the importance of complete physical examination, including rectodigital examination, and surveillance of the lower gastro-intestinal tract in upper gastro-intestinal and pancreato-biliary malignancies, even though the incidence of such metastasis is rare.
Footnotes
P- Reviewers: Lin JK, Redondo-Cerezo E S- Editor: Song XX L- Editor: A E- Editor: Ma S
References
- 1.Patel T. Cholangiocarcinoma. Nat Clin Pract Gastroenterol Hepatol. 2006;3:33–42. doi: 10.1038/ncpgasthep0389. [DOI] [PubMed] [Google Scholar]
- 2.Yeo TP, Hruban RH, Leach SD, Wilentz RE, Sohn TA, Kern SE, Iacobuzio-Donahue CA, Maitra A, Goggins M, Canto MI, et al. Pancreatic cancer. Curr Probl Cancer. 2002;26:176–275. doi: 10.1067/mcn.2002.129579. [DOI] [PubMed] [Google Scholar]
- 3.Carter JT, Grenert JP, Rubenstein L, Stewart L, Way LW. Tumors of the ampulla of vater: histopathologic classification and predictors of survival. J Am Coll Surg. 2008;207:210–218. doi: 10.1016/j.jamcollsurg.2008.01.028. [DOI] [PubMed] [Google Scholar]
- 4.Ghaneh P, Costello E, Neoptolemos JP. Biology and management of pancreatic cancer. Postgrad Med J. 2008;84:478–497. doi: 10.1136/gut.2006.103333. [DOI] [PubMed] [Google Scholar]
- 5.Khan SA, Davidson BR, Goldin R, Pereira SP, Rosenberg WM, Taylor-Robinson SD, Thillainayagam AV, Thomas HC, Thursz MR, Wasan H. Guidelines for the diagnosis and treatment of cholangiocarcinoma: consensus document. Gut. 2002;51 Suppl 6:VI1–VI9. doi: 10.1136/gut.51.suppl_6.vi1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.David M, Lepage C, Jouve JL, Jooste V, Chauvenet M, Faivre J, Bouvier AM. Management and prognosis of pancreatic cancer over a 30-year period. Br J Cancer. 2009;101:215–218. doi: 10.1038/sj.bjc.6605150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Beger HG, Treitschke F, Gansauge F, Harada N, Hiki N, Mattfeldt T. Tumor of the ampulla of Vater: experience with local or radical resection in 171 consecutively treated patients. Arch Surg. 1999;134:526–532. doi: 10.1001/archsurg.134.5.526. [DOI] [PubMed] [Google Scholar]
- 8.Talamini MA, Moesinger RC, Pitt HA, Sohn TA, Hruban RH, Lillemoe KD, Yeo CJ, Cameron JL. Adenocarcinoma of the ampulla of Vater. A 28-year experience. Ann Surg. 1997;225:590–599; discussion 599-600. doi: 10.1097/00000658-199705000-00015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Albores-Saavedra J, Schwartz AM, Batich K, Henson DE. Cancers of the ampulla of vater: demographics, morphology, and survival based on 5,625 cases from the SEER program. J Surg Oncol. 2009;100:598–605. doi: 10.1002/jso.21374. [DOI] [PubMed] [Google Scholar]
- 10.Young JL Jr, Roffers SD, Ries LAG, Fritz AG, Hurlburt AA., editors. SEER summary staging manual-2000: Codes and coding instructions. Bethesda, MD: National Cancer Institute; 2001. [Google Scholar]
- 11.Lee JH, Lee KG, Ha TK, Jun YJ, Paik SS, Park HK, Lee KS. Pattern analysis of lymph node metastasis and the prognostic importance of number of metastatic nodes in ampullary adenocarcinoma. Am Surg. 2011;77:322–329. [PubMed] [Google Scholar]
- 12.Yeh CC, Jeng YM, Ho CM, Hu RH, Chang HP, Tien YW. Survival after pancreaticoduodenectomy for ampullary cancer is not affected by age. World J Surg. 2010;34:2945–2952. doi: 10.1007/s00268-010-0759-y. [DOI] [PubMed] [Google Scholar]
- 13.Bellows C, Gage T, Stark M, McCarty C, Haque S. Metastatic pancreatic carcinoma presenting as colon carcinoma. South Med J. 2009;102:748–750. doi: 10.1097/SMJ.0b013e3181a8fad7. [DOI] [PubMed] [Google Scholar]
- 14.Tokodai K, Kawagishi N, Miyagi S, Takeda I, Sato K, Akamatsu Y, Sekiguchi S, Ishida K, Satomi S. Intestinal obstruction caused by colonic metastasis from intrahepatic cholangiocarcinoma 6 years after removal of the primary tumor: report of a case. Surg Today. 2012;42:797–800. doi: 10.1007/s00595-012-0138-4. [DOI] [PubMed] [Google Scholar]
- 15.Fujii K, Goto A, Yoshida Y, Suzuki K, Matunaga Y, Shinomura Y. Education and imaging. Gastrointestinal: Transmural colonic metastasis arising from primary cholangiocarcinoma. J Gastroenterol Hepatol. 2010;25:1329. doi: 10.1111/j.1440-1746.2010.06396.x. [DOI] [PubMed] [Google Scholar]
- 16.Ogu US, Bloch R, Park G. A rare case of metachronous skip metastasis of pancreatic cancer to the colon. Am Surg. 2012;78:E342–E343. [PubMed] [Google Scholar]
- 17.Fukatsu H, Nagahara Y, Ishiki K, Iwamura M, Hamada F. Pancreatic cancer metastasis to the rectum detected on colonoscopy. Endoscopy. 2009;41 Suppl 2:E167–E168. doi: 10.1055/s-0029-1214732. [DOI] [PubMed] [Google Scholar]
- 18.Hafez H. Cutaneous pancreatic metastasis: a case report and review of literature. Indian J Cancer. 2007;44:111–114. doi: 10.4103/0019-509x.38943. [DOI] [PubMed] [Google Scholar]
- 19.Bochicchio A, Tartarone A, Ignomirelli O, Latorre G, Cangiano R, Gallucci G, Coccaro M, Feudale E, Aieta M. Anal metastasis from breast cancer: a case report and review of the literature. Future Oncol. 2012;8:333–336. doi: 10.2217/fon.12.9. [DOI] [PubMed] [Google Scholar]
- 20.Puglisi M, Varaldo E, Assalino M, Ansaldo G, Torre G, Borgonovo G. Anal metastasis from recurrent breast lobular carcinoma: a case report. World J Gastroenterol. 2009;15:1388–1390. doi: 10.3748/wjg.15.1388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Efthimiadis C, Kosmidis C, Fotiadis P, Anthimidis G, Vasiliadou K, Mekras A, Ioannidou G, Basdanis G. Breast cancer metastatic to the rectum: a case report. Tech Coloproctol. 2011;15 Suppl 1:S91–S93. doi: 10.1007/s10151-011-0740-2. [DOI] [PubMed] [Google Scholar]
- 22.Matsuda I, Matsubara N, Aoyama N, Hamanaka M, Yamagishi D, Kuno T, Tsukamoto K, Yamano T, Noda M, Ikeuchi H, et al. Metastatic lobular carcinoma of the breast masquerading as a primary rectal cancer. World J Surg Oncol. 2012;10:231. doi: 10.1186/1477-7819-10-231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kawahara K, Akamine S, Takahashi T, Nakamura A, Kusano H, Nakagoe T, Nakazaki T, Ayabe H, Tomita M. Anal metastasis from carcinoma of the lung: report of a case. Surg Today. 1994;24:1101–1103. doi: 10.1007/BF01367465. [DOI] [PubMed] [Google Scholar]
- 24.Sakai H, Egi H, Hinoi T, Tokunaga M, Kawaguchi Y, Shinomura M, Adachi T, Arihiro K, Ohdan H. Primary lung cancer presenting with metastasis to the colon: a case report. World J Surg Oncol. 2012;10:127. doi: 10.1186/1477-7819-10-127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Takahashi H, Ikeda M, Takemasa I, Mizushima T, Yamamoto H, Sekimoto M, Doki Y, Mori M. Anal metastasis of colorectal carcinoma origin: implications for diagnosis and treatment strategy. Dis Colon Rectum. 2011;54:472–481. doi: 10.1007/DCR.0b013e318205e116. [DOI] [PubMed] [Google Scholar]
- 26.Smiley D, Goldberg RI, Phillips RS, Barkin JS. Anal metastasis from colorectal carcinoma. Am J Gastroenterol. 1988;83:460–462. [PubMed] [Google Scholar]
- 27.Abbas TO, Al-Naimi AR, Yakoob RA, Al-Bozom IA, Alobaidly AM. Prostate cancer metastases to the rectum: a case report. World J Surg Oncol. 2011;9:56. doi: 10.1186/1477-7819-9-56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Duval JV, Savas L, Banner BF. Expression of cytokeratins 7 and 20 in carcinomas of the extrahepatic biliary tract, pancreas, and gallbladder. Arch Pathol Lab Med. 2000;124:1196–1200. doi: 10.5858/2000-124-1196-EOCAIC. [DOI] [PubMed] [Google Scholar]
- 29.Groisman GM, Bernheim J, Halpern M, Brazowsky E, Meir A. Expression of the intestinal marker Cdx2 in secondary adenocarcinomas of the colorectum. Arch Pathol Lab Med. 2005;129:920–923. doi: 10.5858/2005-129-920-EOTIMC. [DOI] [PubMed] [Google Scholar]
- 30.De Lott LB, Morrison C, Suster S, Cohn DE, Frankel WL. CDX2 is a useful marker of intestinal-type differentiation: a tissue microarray-based study of 629 tumors from various sites. Arch Pathol Lab Med. 2005;129:1100–1105. doi: 10.5858/2005-129-1100-CIAUMO. [DOI] [PubMed] [Google Scholar]
- 31.Moriya T, Kimura W, Hirai I, Takasu N, Mizutani M. Expression of MUC1 and MUC2 in ampullary cancer. Int J Surg Pathol. 2011;19:441–447. doi: 10.1177/1066896911405654. [DOI] [PubMed] [Google Scholar]


