Figure 1.
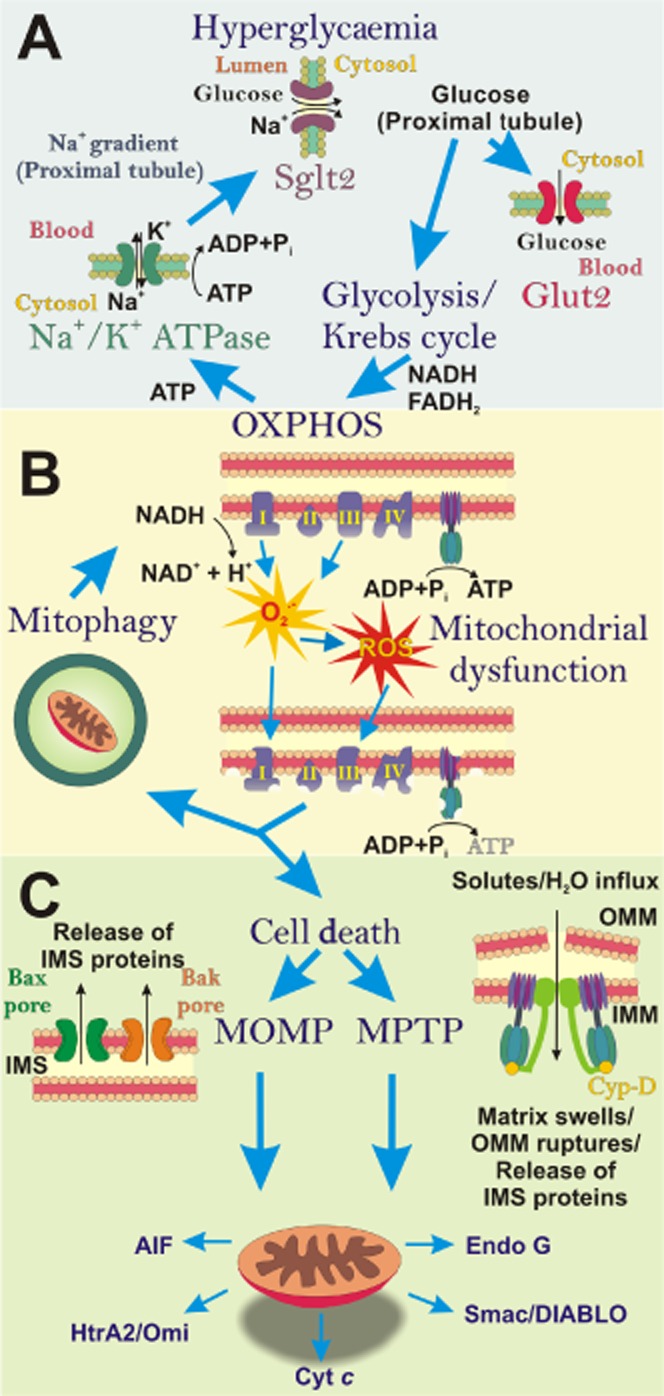
The ‘vicious cycle’ of diabetic nephropathy (DN): impact of hyperglycaemia on mitochondrial function. (A) In the diabetic milieu, excess blood glucose, filtered by the kidneys has to be reabsorbed, predominantly by the S1 segment of the proximal tubule. Glucose is transported through the proximal tubule epithelial cell (PTEC) via Sglt2 (on the apical/luminal surface) and GLUT2 (on the basolateral surface). Within the PTEC, this increased pool of glucose is metabolized and ATP is produced by oxidative phosphorylation (OXPHOS). The resultant ATP is utilized to fuel the Na+/K+-ATPase pump, which drives the Na+ gradient across the proximal tubule, required for co-transport of glucose via Sglt2. (B) During hyperglycaemia, superoxide (O2−) is generated from the electron transport chain (ETC) and can be subsequently converted into other reactive oxygen species (ROS). Excess ROS causes damage to mitochondria and the ETC, resulting in impaired ATP production. These dysfunctional mitochondria can be eliminated by mitophagy. However, when the number of damaged mitochondria overwhelms the mitophagy process, dysfunctional mitochondria can initiate cell death. (C) Apoptosis or programmed necrosis ensues via mitochondria outer membrane permeabilization (MOMP) or mitochondrial permeability transition pore (MPTP). These mechanisms result in the release of inter-membrane space (IMS) proteins from mitochondria into the cytosol, which promote cell death.
