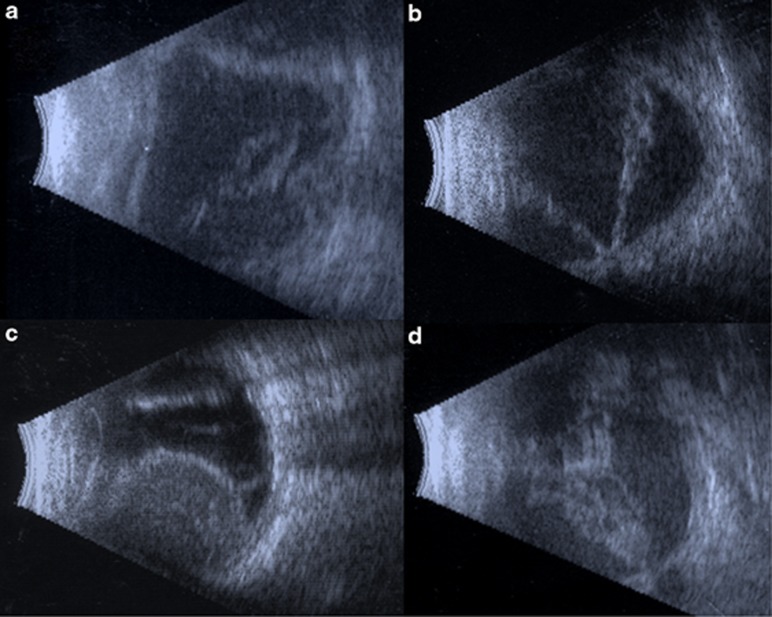
Figure 1.
Ultrasonography examples in ocular trauma. (a) A 71-year-old man with a ruptured globe in a motor vehicle accident. The wound involved zones II and III. B-scan performed 20 days after operation showed loose and membranous vitreous debris, flattening of the globe, and diffuse choroidal thickening with bulging of the optic nerve into the eye suggestive of hypotony. At 2 months after operation, the patient had light perception vision with phthisis. (b) A 14-year-old female who sustained a BB to the eye with retained intraocular FB. B-scan 24 days after the repair and removal of the BB showed a V-shaped membrane, nonmobile, diffusely thickened with cystic components, attaching at the optic nerve, suggestive of a total open funnel retinal detachment. This was verified and repaired 1 week later with PPV/retinectomy/laser and oil. She ultimately developed LP vision and pain and received a retrobulbar chlorpromazine injection for pain. (c) A 76-year-old man with a blunt rupture of his globe resulting in a ruptured extracapsular cataract extraction wound, limbal laceration, and uveal extrusion. B-scan 2 days after the repair showed large dome-shaped membranous elevations containing nonmobile moderate reflective debris with anterior attachment suggestive of non-kissing hemorrhagic choroidal detachments. An overlaying membrane off the base of the choroidal detachment is suggestive of a retinal detachment. After 6 weeks, B-scan showed shallow choroidal detachment, and total retinal detachment. He then underwent scleral buckle, lensectomy, PPV, laser and gas 6 weeks later. Final vision was LP. (d) A 57-year-old man with a blunt rupture resulting in a zone II and III scleral rupture. B-scan 5 weeks later showed diffusely thickened, nonmobile, V-shaped membrane with a point of attachment at the optic nerve, representing a total funnel retinal detachment. After 2 months, the patient had no light perception vision with phthisis.