Abstract
Background
Rapid treatment of acute coronary syndromes (ACS) is important; causes of delay in emergency medical services (EMS) care of ACS are poorly understood.
Methods and results
Analysis of data from the IMMEDIATE randomized controlled trial of EMS treatment of people with symptoms suggesting ACS, using hierarchical multiple regression of elapsed time. Out-of-hospital electrocardiograms were performed on 54,230 adults calling 9-1-1; 871 had presumed ACS, 303 of whom had ST-segment elevation myocardial infarction and underwent percutaneous coronary intervention. Compared to their counterparts, women, participants with diabetes, and participants without prior cardiovascular disease waited longer to call 9-1-1(by 28, p <0.01; 10, p 0.03; and 6 minutes, p 0.02, respectively). EMS arrival to electrocardiogram was longer for women (1.5 minutes, p <0.01), older individuals (1.3 minutes, p <0.01), and those without a primary complaint of chest pain (3.5 minutes, p <0.01). On-scene times were longer for women (2 minutes, p < 0.01) and older individuals (2 minutes, p <0.01). Older individuals and participants presenting on weekends and nights had longer door-to-balloon times (by 10, 14 and 11 minutes respectively, p < 0.01). Women and older individuals had longer total times (medical contact to balloon inflation 16, p 0.01, and 9 minutes, p <0.01, respectively; symptom onset to balloon inflation 31.5 minutes for women, p 0.02).
Conclusions
We found delays throughout ACS care, resulting in substantial differences in total times for women and older individuals. These delays may impact outcomes; a comprehensive approach to reduce delay is needed.
Keywords: acute coronary syndrome, emergency medical services, women
INTRODUCTION
Acute coronary syndromes (ACS) are a major cause of death in the US. 1, 2 The majority of these deaths occur in the first hours after symptom onset, approximately half from ischemia induced arrhythmias. 2–5 Therefore, reducing delays in treatment of patients with ACS should reduce morbidity and mortality. 6–14
Over half of patients hospitalized for ACS arrive via emergency medical services (EMS). 15 Thus, quantifying the time that patients with possible ACS spend in the sequence of EMS care through initiating care at the receiving hospital, and determining the causes of greater durations, are important for developing strategies to reduce delays and thereby improve clinical outcomes. Yet few studies have described time that patients with ACS spend in EMS care or factors associated with longer time in EMS care, 16, 17 and no prior studies have looked at this starting with the population of all patients who have out-of-hospital ECGs performed.
We conducted an exploratory analysis of data from the IMMEDIATE (Immediate Myocardial Metabolic Enhancement During Initial Assessment and Treatment in Emergency care) Trial, a randomized controlled trial of EMS treatment of patients for symptoms suggestive of ACS. 18 The goal was to ascertain durations of time that patients with potential ACS spend in the entire sequence of care from initial EMS contact until initiation of definitive treatment at the receiving hospital (e.g., inflation of a percutaneous coronary intervention (PCI) balloon) and to determine which patient characteristics are associated with longer times. We hypothesized that female sex, older age, minority race/ethnicity, presence of diabetes mellitus, a lack of history of cardiovascular disease, and occurrence of event on weekend and overnight would be associated with longer times.
METHODS
Study design and setting
This was a retrospective analysis of data from the IMMEDIATE Trial. 18 The IMMEDIATE Trial was a multicenter, double-blind, randomized placebo controlled clinical effectiveness trial of intravenous glucose-insulin-potassium (GIK) evaluating whether GIK reduced progression of unstable angina pectoris to myocardial infarction, and if it reduced mortality, cardiac arrest, development of heart failure, and infarct size in patients with a high suspicion of ACS. The IMMEDIATE Trial methods have been previously published. 18, 19 The study was conducted between 2006 and 2011 and enrolled participants from 13 US cities. Identification of participants with ACS by paramedics was aided by the ECG-based acute cardiac ischemia time-insensitive predictive Instrument (ACI-TIPI) and thrombolytic predictive instrument (TPI) decision support, using an ACI-TIPI threshold of 75% or higher predicted probability of having ACS, detection of suspected STEMI by the TPI, or both. 20 This resulted in a population of study participants with a high rate of ACS.
Selection of participants
We analyzed data from three cohorts from the IMMEDIATE Trial: all participants aged 18 years and older with a 12-lead out-of-hospital ECG who were screened to determine eligibility for inclusion; participants with high risk of ACS who met the trial eligibility criteria, agreed to have the study drug started in the ambulance and provided written informed consent; and participants who had an adjudicated diagnosis of STEMI and underwent percutaneous coronary intervention (PCI) within 12 hours of their initial presentation to EMS. For each outcome measure, we analyzed the largest sample for which we had data available.
This study was reviewed and approved by the Tufts Medical Center institutional review board. All participants with out-of-hospital ECG performed had de-identified data collected as part of the screening process to determine eligibility for enrollment into the IMMEDIATE Trial. All participants enrolled in the IMMEDIATE Trial provided written informed consent that allows for analyses of these data presented.
Independent variables
We assessed for differences in time intervals by sex, age, past medical history of cardiovascular disease (CVD), history of diabetes, minority ethnicity or race, day of week and time of day. Age was entered into the model as a categorical variable, while all other independent predictors were entered as binary variables (day of week was entered as weekend and weekday and time of day as overnight or daytime). Ethnicity and race were combined into a single variable for purposes of analysis. Non-Hispanic whites were defined as participants of white race and were not Hispanic ethnicity. Minorities were defined as all participants of non-white race (including black, Native American, Asian, and Hawaiian) and Hispanic ethnicity.
Outcome measures
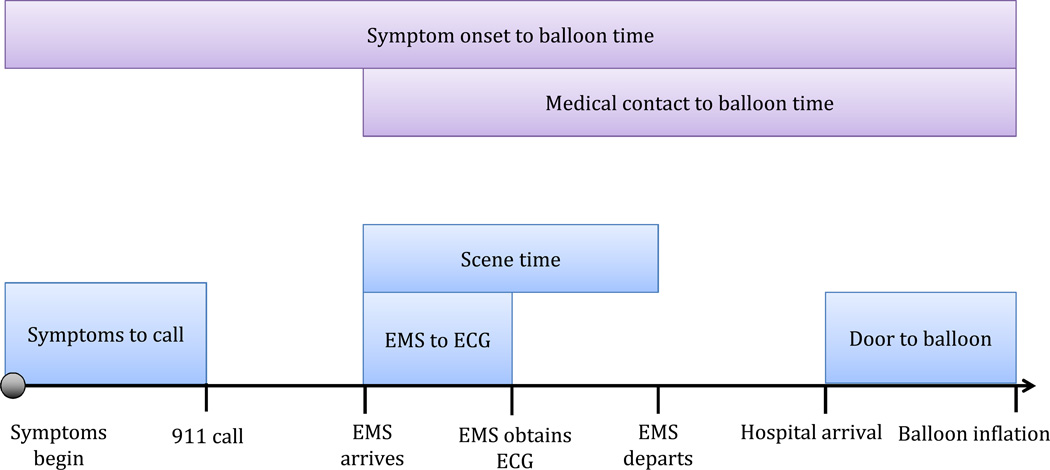
We analyzed time intervals (in minutes) from the time of symptom onset through PCI balloon inflation (figure 1). Each time interval was analyzed as a continuous outcome. Time of symptom onset was obtained via patient recall at the time of transport. All times in EMS care were obtained from EMS runsheets with the exception of the ECG time, which was taken from the ECG timestamp. Hospital times, including time of arrival at the hospital and time of PCI balloon inflation, were obtained from medical records. All time interval definitions were agreed upon prior to conducting the study.
Figure 1.
Time intervals and goals for each time interval
Blue boxes display the individual time intervals, purple boxes depict comprehensive time intervals
Goal times are derived from AHA/ACC guidelines
Measured time intervals
Time from symptom onset to 9-1-1 call
Time from symptom onset to 9-1-1 call was defined as the time interval from the onset of symptoms concerning for ACS until the participant called 9-1-1. Data for this time interval were analyzed for participants with a high risk of ACS.
Time from EMS arrival to out-of-hospital ECG
Time from EMS arrival to out-of-hospital ECG was defined as the time interval from EMS arrival on scene and out-of-hospital ECG timestamp. Data for this time interval were analyzed for all participants receiving an out-of-hospital ECG.
Scene time
Scene time was defined as the time interval between EMS arrival on scene and EMS departure from scene. Data for this time interval were analyzed for participants with a high risk of ACS.
Hospital arrival to balloon inflation
Hospital arrival to balloon inflation was defined as the time interval between arrival at the hospital and PCI balloon inflation. Data for this time interval were analyzed for the STEMI cohort.
Cumulative time intervals
In addition to the analysis of individual time intervals as defined above, two cumulative time intervals were analyzed.
Medical contact to balloon inflation
First medical contact to balloon inflation was defined as the time interval between EMS arrival on scene and time of PCI balloon inflation.
Symptom onset to balloon inflation
Symptom onset to balloon inflation was defined as the time interval between the onset of symptoms and PCI balloon inflation.
Data handling
Minutes for each time interval were calculated from collected date and time information using excel. For the largest dataset (all participants receiving out-of-hospital ECGs), some times were improbable (546 times between 0 and 1 minute, 1790 times less than 0 minutes, 866 times greater than 60 minutes). Where likely to be a reporting error (i.e. around daylight savings times), these times were corrected by hand to the likely value. This resulted in 2,084 of 51,975(4%) data points being corrected. The remaining 1,118 of 51,975 improbable times were excluded. A sensitivity analysis was conducted without this data, but resulted in little impact on the model coefficients. One door-to-balloon time was recorded as 1 minute and was also removed from the analysis.
Missing data were excluded from the analysis. Data were missing for 194 of 871 (22%) participants for the interval of symptom onset to 9-1-1 call, 2,838 of 51,975 participants for EMS arrival to out-of-hospital ECG (5.4%), 12 of 871 participants (1.4%) for on-scene time, 1 of 303 (0.3%) for door-to-balloon time, 5 of 303 (1.7%) for medical contact to balloon time, and 51 of 303 (17%) for symptom onset to balloon time.
Statistical analysis
Descriptive statistics were used to report median times for each time interval. We then assessed for an association of each time interval with study site. There were significant associations between study site and time, therefore hierarchical multiple regression models were used for all analyses. All p values are the product of hierarchical multiple regression models, adjusting for all other variables in the model. Hierarchical multiple regressions were used to assess for differences in times by sex, age, primary complaint of chest pain, day of week, time of day, medical history of CVD (including history of myocardial infarction, PCI, coronary artery bypass grafting, congestive heart failure, and prior stroke), and participant race and ethnicity, while controlling for clustering of outcomes at the site level. Patient factors were forced into the models as fixed effects and the study site was forced into the models as a random effect. Log transformations of time were performed prior to regression analysis due to right skewed distributions. Linear regressions were used to model elapsed time (in log minutes). For time intervals with outliers, sensitivity analyses were performed with truncated times. All analyses were conducted using R statistical software, version 2.13.1.
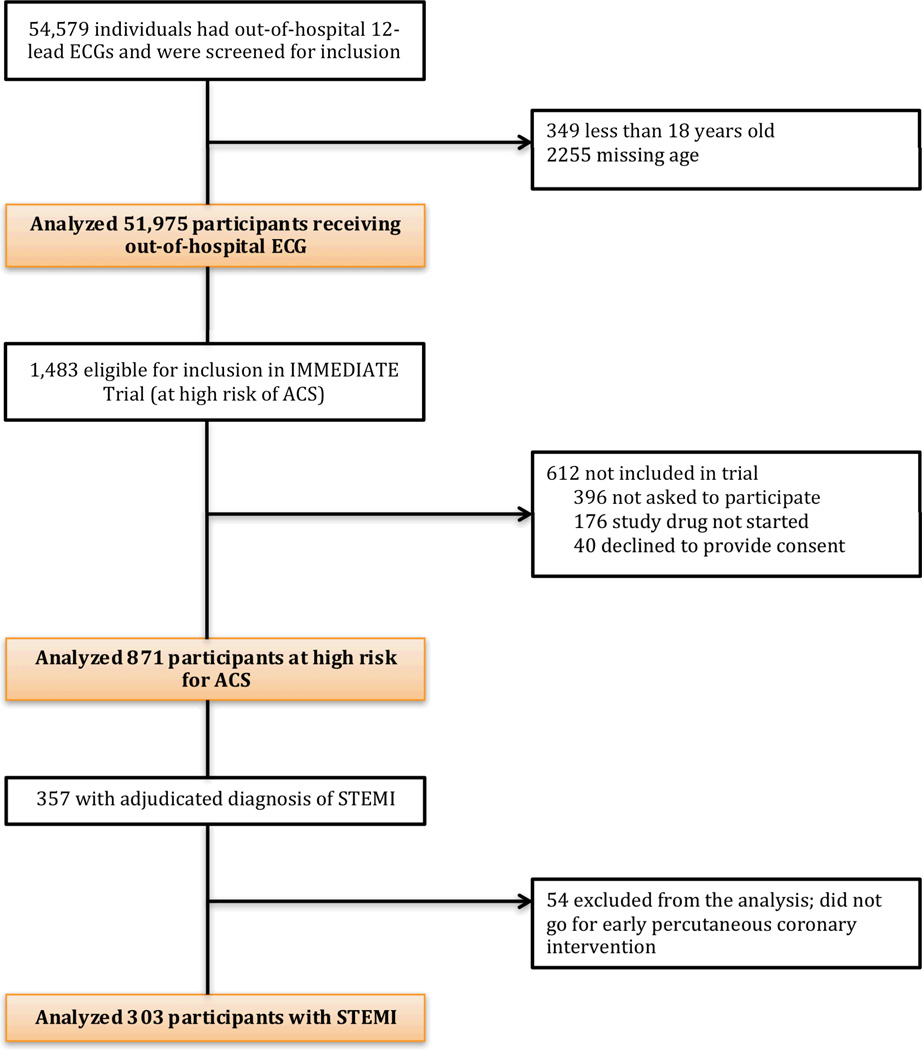
RESULTS
Table 1 presents patient characteristics. Of the 54,579 individuals with out-of-hospital 12 lead ECGs performed, 51,975 were aged 18 or over and were included in the analysis (figure 2). A total of 871 of the 51,975 were enrolled in the IMMEDIATE Trial18 and were included in the analysis of participants with high risk of ACS. There were 303 of the 871 who had an adjudicated diagnosis of STEMI and went for PCI within 12 hours of the study drug starting. These participants were included in the analysis of participants with STEMI.
Table 1.
Baseline characteristics of study participants
| All participants receiving ECG* (N=51,975) |
Participants at high risk of ACS (N=871) |
Participants with STEMI (N=303) |
|
|---|---|---|---|
| Age, mean (SD), y | 63 (17.9) | 63.6 (14) | 61.3 (12.3) |
| Male sex | 26,201 (50%) | 618 (71%) | 228 (75%) |
| Race | |||
| White | 724 (83%) | 267 (89%) | |
| Black | 94 (11 %) | 17 (6%) | |
| Native American | 16 (2%) | 7 (2%) | |
| Asian | 16 (2%) | 4 (1%) | |
| Native Hawaiian | 3 (0.3%) | 1 (0.3%) | |
| Other | 8 (1%) | 3 (1%) | |
| Hispanic ethnicity | 102 (12%) | 43 (14%) | |
| Chest pain primary complaint | 21,834 (44%) | 749 (86%) | 282 (93%) |
| Weekend | 13,676 (26%) | 243 (28%) | 94 (31%) |
| Overnight | 19,067 (37%) | 323 (37%) | 104 (34%) |
| Past Medical History | |||
| Myocardial infarction | 311 (36%) | 70 (23%) | |
| Coronary artery bypass grafting | 141 (16%) | 11 (4%) | |
| Congestive heart failure | 145 (17%) | 14 (5%) | |
| Cerebrovascular accident | 86 (10%) | 18 (6%) | |
| Percutaneous coronary intervention | 264 (30%) | 67 (22%) | |
| Diabetes mellitus | 242 (28%) | 61 (20%) |
Abbreviations: ECG, electrocardiogram; ACS, acute coronary syndrome; STEMI, ST-segment myocardial infarction
Data on race, ethnicity and past medical history not available for all participants receiving an out-of-hospital ECG
Figure 2.
Study population
Overall median times
Overall median times were 53 minutes for the interval of symptom onset to 9-1-1 call, 15.2 minutes from EMS arrival to out-of-hospital ECG, 20 minutes on-scene, and 62 minutes from door to balloon time. Six percent of participants received an out-of-hospital ECG within 5 minutes and 27% within 10 minutes. Participants with STEMI had median times of 94 minutes from medical contact to PCI balloon inflation, and 156 minutes from symptom onset to balloon inflation.
Association of sex with time
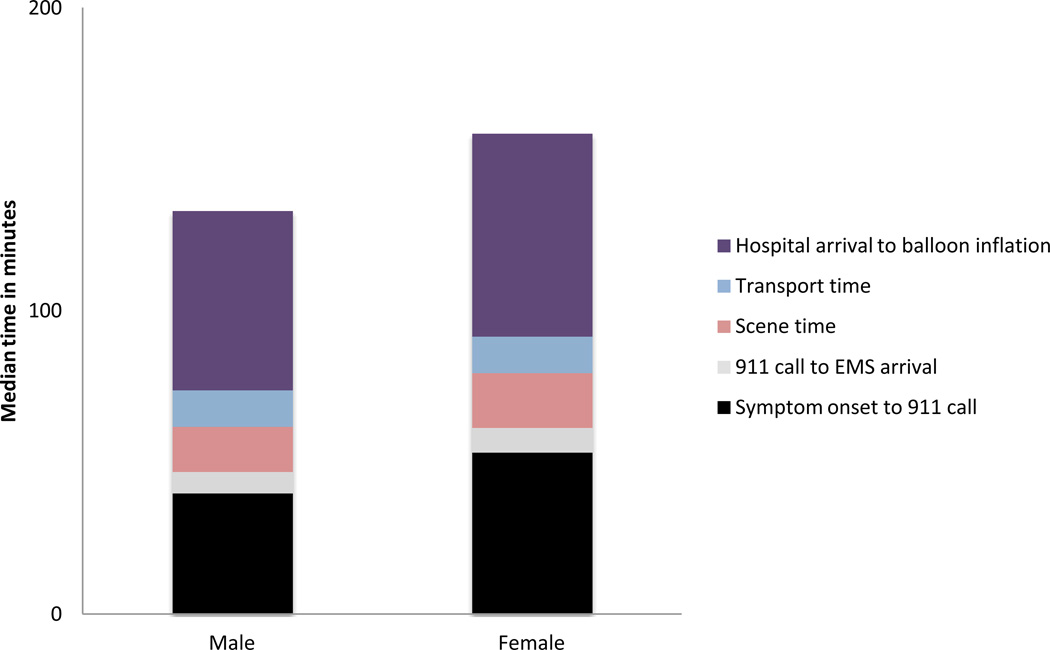
Table 2 presents median times for each time interval by sex and figure 3 displays time intervals for participants with STEMI by sex. For interest, figure 3 provides the breakdown of all time intervals from symptom onset until balloon inflation. The time intervals of 9-1-1 call to EMS arrival and transport time were not separately analyzed due to concern for confounding by distance, which was unmeasured in this study.
Table 2.
Association of demographic variables with median times
| Median times (minutes)* | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Sex | Age group, years | Race/ethnicity | |||||||||
| Interval | Males | Females | P- value* |
<55 | 55–64 | >64 | P- value† |
Non-Hispanic whites |
Minorities | P- value† |
|
| Symptom onset to 9-1-1 call (n=677) | 45 | 73 | <0.01 | 41 | 54 | 56 | 0.4 | 50 | 58 | 0.99 | |
| EMS arrival to out-of-hospital ECG (n=49,061) | 14.5 | 16 | <0.01 | 14.1 | 14.9 | 16.2 | <0.01 | n/a* | n/a | ||
| Scene time (n=859) | 19 | 21 | <0.01 | 19 | 18 | 21 | <0.01 | 19 | 22 | 0.26 | |
| Hospital arrival to balloon inflation (n=301) | 59 | 67 | 0.05 | 63.5 | 56 | 66 | <0.01 | 60.5 | 65.5 | 0.53 | |
| Medical contact to balloon inflation (n=298) | 90.5 | 106.5 | 0.01 | 95.5 | 88 | 97 | <0.01 | 91 | 97 | 0.62 | |
| Symptom onset to balloon inflation (N=252) | 148.5 | 180 | 0.02 | 144 | 157 | 167.5 | 0.09 | 150 | 162.5 | 0.61 | |
Abbreviations: EMS, emergency medical service; ECG, electrocardiogram
Median times are unadjusted
P-values are adjusted for age, race/ethnicity, presence of chest pain as the primary complaint, day of week, time of day, past medical history of cardiovascular disease and past medical history of diabetes mellitus
Data on race, ethnicity and past medical history not available for all participants receiving an out-of-hospital ECG
Figure 3.
Participants with STEMI time intervals*
*Times presented are unadjusted. For interest, times are separated into intervals.
The time intervals of 911 call to EMS arrival and transport time were not separately analyzed in this study.
Compared to men, median times were longer for women for the time intervals from symptom onset to 9-1-1 call (unadjusted medians 73 versus 45 minutes; multivariate adjusted p value <0.01), EMS arrival to out-of-hospital ECG (unadjusted medians 16 versus 14.5 minutes; multivariate adjusted p value <0.01), and on-scene time (unadjusted medians 21 versus 19 minutes; multivariate adjusted p value <0.01). A sensitivity analysis was conducted on the time interval of hospital arrival to balloon inflation due to the presence of outliers but removing the 4 points identified as outliers resulted in little impact on model coefficients (change in beta coefficient of 4%), so the original analysis is presented here.
Comprehensive time intervals
Women had an unadjusted median time from medical contact to balloon inflation of 106.5 minutes compared to 90.5 minutes for men (multivariate adjusted p value 0.01). Time from symptom onset through balloon inflation was 180 minutes for women compared to 148.5 minutes for men (multivariate adjusted p value 0.02).
Association of age with time
Table 2 shows median times by age.
There was no association of age with time from symptom onset to 9-1-1 call. Older age was associated with longer time to ECG (unadjusted median times 14.1 minutes for individuals aged < 55 years, 14.9 minutes for individuals aged 55–64 years, and 16.2 minutes for individuals aged > 64 years; multivariate adjusted p value <0.01), on-scene time (unadjusted median times 19 minutes for individuals aged < 55 years, 18 minutes for individuals aged 55–64 years, and 21 minutes for individuals aged > 64 years; multivariate adjusted p value <0.01), and hospital arrival to balloon inflation (unadjusted median times 63.5 minutes for individuals aged < 55 years, 56 minutes for individuals aged 55–64, and 66 minutes for individuals aged > 64 years; multivariate adjusted p value<0.01). A sensitivity analysis was conducted for the time interval of hospital arrival to balloon inflation due to the presence of outliers, but removing the 4 points identified as outliers had little impact on model coefficients (change of 1% in beta coefficient for the eldest group and 15% for the middle age group).
Comprehensive time intervals
After adjusting for covariates there was a significant association of age with longer time from medical contact to balloon inflation (unadjusted median times 95.5 minutes for individuals aged <55 years, 88 minutes for individuals aged 55–64 years, and 97 minutes for individuals aged >64 years; multivariate adjusted p value <0.01).
Association of race/ethnicity with time
Table 2 shows median times by race/ethnicity.
After adjusting for covariates, race/ethnicity was not associated with significant differences in median time from symptom onset to 9-1-1 call, on-scene time, hospital arrival to balloon inflation. Race/ethnicity data was not available for the largest cohort of participants (all participants receiving an out-of-hospital ECG), for whom the analysis of time from EMS arrival to out-of-hospital ECG was conducted.
Comprehensive time intervals
After adjusting for covariates, race/ethnicity was not associated with significant differences in median time from medical contact to balloon inflation or symptom onset to balloon inflation
Association of chest pain as the primary complaint with time
Table 3 shows median times by presence of chest pain as the primary complaint.
Table 3.
Association of primary complaint and past medical history with median times
| Median times (minutes)* | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Chest pain primary complaint | History of Diabetes Mellitus |
History of cardiovascular disease | |||||||
| Interval | Yes | No | P-value† | No | Yes | P- value† |
No | Yes | P- value† |
| Symptom onset to 9-1-1 call (n=677) | 54 | 37 | <0.01 | 50 | 60 | 0.02 | 56 | 50 | 0.03 |
| EMS arrival to out-of-hospital ECG (n=49,061) | 13.5 | 17 | <0.01 | n/a‡ | n/a‡ | n/a‡ | n/a‡ | ||
| Scene time (n=859) | 19 | 21 | 0.89 | 19 | 21 | 0.47 | 19 | 20.5 | 0.35 |
| Hospital arrival to balloon inflation (n=301) | 63 | 53 | 0.85 | 61 | 67 | 0.41 | 60 | 66.5 | 0.49 |
| Medical contact to balloon inflation (n=298) | 94 | 85.5 | 0.78 | 94 | 97 | 0.46 | 92.5 | 97 | 0.47 |
| Symptom onset to balloon inflation (n=252) | 158 | 122 | 0.16 | 156 | 159 | 0.81 | 159 | 152 | 0.07 |
Abbreviations: EMS, emergency medical services; ECG, electrocardiogram
Median times are unadjusted
P-values are adjusted for age, race/ethnicity, presence of chest pain as the primary complaint, day of week, time of day, past medical history of cardiovascular disease and past medical history of diabetes mellitus
Data on race, ethnicity and past medical history not available for all participants receiving an out-of-hospital ECG
After adjusting for covariates, participants without chest pain as a primary complaint called 9-1-1 compared to participants with chest pain (unadjusted median times 37 minutes compared to 54 minutes; multivariate adjusted p value <0.01). The primary complaints that were associated with shorter median times to call were abdominal pain (n=6, median 17.5 minutes), cardiac arrest (n=1, 2 minutes), chest numbness (n=1, 41 minutes), diaphoresis (n=2, median 3 minutes), dizziness (n=4, median 24 minutes), epigastric pain (n=1, 17 minutes), heartburn (n=3, median 24 minutes), implantable cardiac defibrillator firing (n=1, 16 minutes), loss of consciousness (n=9, median 11 minutes), near syncope (n=1, 10 minutes), seizure (n=2, median 34 minutes), shoulder/arm pain (n=7, median 45 minutes), sudden collapse (n=1, 1 minute), and syncope (n=3, median 5 minutes). Additionally, some of the participants with shortness of breath, palpitations and weakness called EMS faster than the median time for those with chest pain.
Participants without a primary complaint of chest pain had longer time from EMS arrival to out-of-hospital ECG after adjusting for covariates (unadjusted median times 17 minutes compared to 13.5 minutes; multivariate adjusted p value <0.01). There were no associations of chest pain as the primary complaint with on-scene time, hospital arrival to balloon inflation, medical contact to balloon inflation, or symptom onset to balloon inflation.
Association of past medical history of CVD and diabetes with time intervals
Table 3 shows median times by medical history of diabetes and CVD.
Symptom onset to 9-1-1 call
After adjusting for covariates, participants with a history of diabetes had longer time from symptom onset to 9-1-1 call (unadjusted median times 60 minutes compared to 50 minutes; multivariate adjusted p value 0.02), and those with a history of CVD had shorter time from symptom onset to 9-1-1 call (unadjusted median times 50 minutes compared to 56 minutes; multivariate adjusted p value 0.03). There were no associations of history of diabetes mellitus or CVD with on-scene times or hospital arrival to balloon inflation. Data on medical history was not available for the largest cohort of participants, on whom the analysis of EMS arrival to out-of-hospital ECG was conducted.
Comprehensive time intervals
After adjusting for covariates, participants with a history of CVD had a trend toward faster time from symptom onset to balloon inflation (unadjusted median times 152 minutes compared to 159 minutes; multivariate adjusted p value 0.07). There was no difference in medical contact to balloon inflation by past medical history.
Association of weekend and night presentations with time
Table 4 shows median times by day of week and time of day.
Table 4.
Association of day of week and time of day with median times
| Median times (minutes)* | ||||||
|---|---|---|---|---|---|---|
| Day of week | Time of day | |||||
| Interval | Weekday | Weekend | P-value† | 7am-7pm | 7pm-7am | P-value† |
| Symptom onset to 9-1-1 call (n=677) | 55 | 44 | 0.51 | 53 | 34.5 | 0.37 |
| EMS arrival to out-of-hospital ECG (n=49,061) | 15.3 | 15.1 | 0.12 | 15.4 | 14.9 | 0.03 |
| Scene time (n=859) | 20 | 19 | 0.39 | 19 | 20 | 0.4 |
| Hospital arrival to balloon inflation (n=301) | 58 | 72 | <0.01 | 58 | 69 | <0.01 |
| Medical contact to balloon inflation (n=298) | 90 | 104.5 | <0.01 | 89 | 98.5 | <0.01 |
| Symptom onset to balloon inflation (n=252) | 160 | 147.5 | 0.6 | 155.5 | 156 | 0.51 |
Abbreviations: EMS, emergency medical services; ECG, electrocardiogram
Median times are unadjusted
P-values are adjusted for age, race/ethnicity, presence of chest pain as the primary complaint, day of week, time of day, past medical history of cardiovascular disease and past medical history of diabetes mellitus
There were no associations of night or weekend presentation with time from symptom onset to 9-1-1 call or on-scene time. Participants presenting during daytime hours had longer time from EMS arrival to out-of-hospital ECG compared to those presenting during overnight hours, after adjusting for covariates (unadjusted median times 14.9 minutes compared to 15.4 minutes; multivariate adjusted p value 0.03). After adjusting for covariates, participants who presented on weekends had longer time from hospital arrival to balloon inflation than those who presented on weekdays (unadjusted median times 72 minutes compared to 58 minutes; multivariate adjusted p value <0.01). Participants who presented during overnight hours (7pm-7am) had longer time than those who presented during daytime hours (7am-7pm) (unadjusted median times 69 minutes compared to 58 minutes; multivariate adjusted p value <0.01). A sensitivity analysis was conducted for hospital arrival to balloon inflation due to the presence of outliers, but removing the 4 points identified as outliers had little impact on model coefficients (change of 5% in beta coefficient for night presentation and 6% in beta coefficient for weekend presentation).
Comprehensive time intervals
After adjusting for covariates, participants who presented on weekends had longer time from medical contact to balloon inflation than those who presented on weekdays (unadjusted median times 104.5 minutes compared to 90 minutes; multivariate adjusted p value <0.01). Participants presenting during overnight hours had longer time than those presenting during daytime hours (unadjusted median times 98.5 minutes compared to 89 minutes; multivariate adjusted p value <0.01).
Additional analyses
A sensitivity analysis excluding corrected times for the analysis of all participants receiving an out-of-hospital ECG was conducted. This had little impact on the estimates, so the corrected times were included in the final analysis.
A sensitivity analysis was conducted for participants with STEMI using truncated door to balloon times due to outliers in the door to balloon time interval. This resulted in little impact in the model estimates, so the raw data was used for the final analysis.
DISCUSSION
In this study of patients calling 9-1-1 for symptoms suggesting ACS, we found delays in the entire chain of care, from the calling of 9-1-1, to care on-scene, to care at the hospital. Delays were present for women and the elderly in most time intervals, culminating in larger magnitude differences in total times. These findings indicate the need for a comprehensive approach to improving early detection of ACS, starting with patients themselves.
For the interval from symptom onset to 9-1-1 call, overall median times were close to an hour. This is substantially better than reported in prior studies, 21–23 but much longer than the goal time of 5 minutes that is advised by the ACC/AHA, 24 which only 10% of participants met. Reducing delays in this time interval has great potential to improve the outcomes of patients with ACS, given that so many deaths occur early. 2–5 Consistent with prior studies, we found that women, 21, 25–29 participants with a history of diabetes, 21–23, 26–29 and those without a history of CVD, 21, 26 took longer to call for help. It is possible that women consider themselves to be at lower risk for ACS, and therefore delay calling for help. Patients with diabetes may delay calling due to less severe symptoms, whereas those with a history of CVD may recognize the symptoms and call sooner than those without a CVD history. It is not clear why a primary complaint of chest pain was associated with a longer time to call 9-1-1 in participants at high risk of ACS. This may represent the alternate symptoms still being characteristic of ACS, and this finding was not present in participants with STEMI. This association is difficult to interpret due to potential inconsistencies in the descriptions of symptoms, and further study is needed.
To our knowledge, this is the first description of time from EMS arrival to out-of-hospital ECG, a critical time interval in the diagnosis and management of ACS. In our study, time from EMS arrival to out-of-hospital ECG was 15 minutes in all participants. This interval could likely be reduced, leading to earlier detection of ACS. Women, older individuals, members of minorities and those with a primary complaint other than chest pain had longer median times from EMS arrival to out-of-hospital ECG. Reasons for these differences are unclear. Perhaps women are perceived as lower risk and the EMS provider takes longer to decide to obtain an ECG. It may take longer to obtain an ECG in an older individual due to more difficulty performing the other pre-hospital tasks, such as obtaining IV access, and placing the patient on a stretcher. It likely takes longer for EMS to obtain a history concerning for possible ACS in patients without a primary complaint of chest pain, and thus takes longer to obtain an ECG in those patients.
Overall median on-scene times were 20 minutes for participants with ACS and 16 minutes for those with STEMI, which is close to the goals recommended by the ACC/AHA24 and represents good quality care. However, women and older individuals had longer times than their counterparts in this interval as well, and targeted improvements are needed.
Women and older individuals continued to have longer times than their counterparts after arrival at the hospital, with differences of greater magnitude than in the EMS setting. The reasons for these delays are unclear, but our findings are consistent with prior studies, 9, 10, 30 and indicate the need for continued efforts to reduce delays in the hospital setting. Day-of-week and time-of-day were only associated with longer times in the hospital setting. Presumably the absence of this effect in the EMS setting is because of the 24-hour 7-day EMS function. Implementation of a similar shift work structure in the hospital with 24-hour 7-day in-house personnel may result in improved times on weekends and overnights.
This study has several strengths. It addresses an important gap in the knowledge of treatment of patients with suspected ACS as the first study to assess for differences in EMS time intervals for all people evaluated by EMS for a possible cardiac complaint. These time intervals are crucial in the diagnosis and treatment of ACS. The data were prospectively collected in a large clinical effectiveness trial that had a very high rate of inclusion of patients in the community calling 9-1-1 for potential cardiac symptoms, and in a wide variety of communities and ethnic groups. There were 32 participating EMS systems in this geographically diverse sample. This increases the study’s generalizability, and increases the likelihood that our findings are relevant to patients being transported by other EMS systems. There are, however, several limitations to this study that must be kept in mind when interpreting the results. This was intended to be primarily a descriptive study. However, we conducted analyses to assess for differences in times by patient characteristics, and did not adjust p values to account for multiple testing. All of the effects were based on separate hypotheses for which the literature and clinical practice provides support, and the analyses were decided a priori. Second, our largest dataset, for which we analyzed time from EMS arrival to out-of-hospital ECG had more missing data than the smaller datasets. Third, distance information was not collected, and therefore we could not control for possible confounding of effect by distance from hospital. Fourth, the number of participants in our study with STEMI and without chest pain was small. Fifth, the EMS providers in this study had training specific to being involved in a study. This may have affected their clinical performance in terms of identifying STEMI and rapidly transporting those patients to the hospital, which may limit this study’s generalizability to other EMS systems. However, this additional training in recognizing ACS and STEMI would likely bias our study against finding delays. Thus it may be that delays are larger than what we found in this study. Sixth, our comprehensive time intervals are for participants with STEMI, which limits our ability to generalize these findings to the general ACS population. Since the time differences for ACS participants were in the same direction as participants with STEMI, we think it is likely that there is a cumulative effect of time differences for people with ACS as well as those with STEMI, but we are unable to answer this question definitively with our data. Finally, we did not have data on race and past medical history for all participants receiving an out-of-hospital ECG.
In summary, we found delays along the entire spectrum of care for patients with possible ACS, beginning with the patient’s 9-1-1 call. These delays were additive, resulting in longer time differences for women and older individuals in the comprehensive intervals. While reduction of delays in all of these time intervals is important, we think that lessening time from symptom onset to 9-1-1 call and time from EMS arrival to out-of-hospital ECG are the most likely to improve early detection of ACS, and thereby impact patient outcomes.
What is known
There are delays in hospital care of acute coronary syndrome for certain categories of patients including women, elderly, and those without chest pain
What this article adds
Identifies additional delays in pre-hospital care of patients with suspected acute coronary syndrome
Shows cumulative delays over the span of care for women
Acknowledgments
FUNDING SOURCES
This work was supported by the National Center for Research Resources Grant Number UL1RR025752, now the National Center for Advancing Translational Sciences, National Institutes of Health (NIH) Grant Number Ul1 TR000073. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
The IMMEDIATE Trial was funded by the National Institutes of Health cooperative agreement from National Heart, Lung and Blood Institute (U01HL077821, U01HL077826, U01HL077823). The IMMEDIATE Trial is registered at www.ClinicalTrials.gov (NCT00091507).
Footnotes
DISCLOSURES:
No financial conflicts of interest to disclose
References
- 1.Hoyert DL, Xu J. Deaths: Preliminary data for 2011. National vital statistics reports : from the Centers for Disease Control and Prevention, National Center for Health Statistics, National Vital Statistics System. 2012;6:1–52. [PubMed] [Google Scholar]
- 2.Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, Borden WB, Bravata DM, Dai S, Ford ES, Fox CS, Franco S, Fullerton HJ, Gillespie C, Hailpern SM, Heit JA, Howard VJ, Huffman MD, Kissela BM, Kittner SJ, Lackland DT, Lichtman JH, Lisabeth LD, Magid D, Marcus GM, Marelli A, Matchar DB, McGuire DK, Mohler ER, Moy CS, Mussolino ME, Nichol G, Paynter NP, Schreiner PJ, Sorlie PD, Stein J, Turan TN, Virani SS, Wong ND, Woo D, Turner MB American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics-2013 update: a report from the American Heart Association. Circulation. 2013;127:e6–e245. doi: 10.1161/CIR.0b013e31828124ad. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Selker HP, Raitt MH, Schmid CH, Laks MM, Beshansky JR, Griffith JL, Califf RM, Selvester RH, Maynard C, D'Agostino RB, Weaver WD. Time-dependent predictors of primary cardiac arrest in patients with acute myocardial infarction. Am J Cardiol. 2003;91:280–286. doi: 10.1016/s0002-9149(02)03155-7. [DOI] [PubMed] [Google Scholar]
- 4.Oliver MF, Opie LH. Effects of glucose and fatty acids on myocardial ischaemia and arrhythmias. Lancet. 1994;343:155–158. doi: 10.1016/s0140-6736(94)90939-3. [DOI] [PubMed] [Google Scholar]
- 5.Kurien VA, Yates PA, Oliver MF. Free fatty acids, heparin, and arrhythmias during experimental myocardial infarction. Lancet. 1969;2:185–187. doi: 10.1016/s0140-6736(69)91424-x. [DOI] [PubMed] [Google Scholar]
- 6.Boersma E, Maas AC, Deckers JW, Simoons ML. Early thrombolytic treatment in acute myocardial infarction: reappraisal of the golden hour. Lancet. 1996;348:771–775. doi: 10.1016/S0140-6736(96)02514-7. [DOI] [PubMed] [Google Scholar]
- 7.De Luca G, Suryapranata H, Zijlstra F, van 't Hof AW, Hoorntje JC, Gosselink AT, Dambrink JH, de Boer MJ ZWOLLE Myocardial Infarction Study Group. Symptom-onset-to-balloon time and mortality in patients with acute myocardial infarction treated by primary angioplasty. J Am Coll Cardiol. 2003;42:991–997. doi: 10.1016/s0735-1097(03)00919-7. [DOI] [PubMed] [Google Scholar]
- 8.De Luca G, Suryapranata H, Ottervanger JP, Antman EM. Time delay to treatment and mortality in primary angioplasty for acute myocardial infarction: every minute of delay counts. Circulation. 2004;109:1223–1225. doi: 10.1161/01.CIR.0000121424.76486.20. [DOI] [PubMed] [Google Scholar]
- 9.Rathore SS, Curtis JP, Nallamothu BK, Wang Y, Foody JM, Kosiborod M, Masoudi FA, Havranek EP, Krumholz HM. Association of door-to-balloon time and mortality in patients >or =65 years with ST-elevation myocardial infarction undergoing primary percutaneous coronary intervention. Am J Cardiol. 2009;104:1198–1203. doi: 10.1016/j.amjcard.2009.06.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rathore SS, Curtis JP, Chen J, Wang Y, Nallamothu BK, Epstein AJ, Krumholz HM National Cardiovascular Data Registry. Association of door-to-balloon time and mortality in patients admitted to hospital with ST elevation myocardial infarction: national cohort study. BMJ. 2009;338:b1807. doi: 10.1136/bmj.b1807. doi: b1807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tarantini G, Cacciavillani L, Corbetti F, Ramondo A, Marra MP, Bacchiega E, Napodano M, Bilato C, Razzolini R, Iliceto S. Duration of Ischemia Is a Major Determinant of Transmurality and Severe Microvascular Obstruction After Primary Angioplasty: A Study Performed With Contrast-Enhanced Magnetic Resonance. J Am Coll Cardiol. 2005;46:1229–1235. doi: 10.1016/j.jacc.2005.06.054. [DOI] [PubMed] [Google Scholar]
- 12.Terkelsen CJ, Sorensen JT, Maeng M, Jensen LO, Tilsted HH, Trautner S, Vach W, Johnsen SP, Thuesen L, Lassen JF. System delay and mortality among patients with STEMI treated with primary percutaneous coronary intervention. JAMA. 2010;304:763–771. doi: 10.1001/jama.2010.1139. [DOI] [PubMed] [Google Scholar]
- 13.Emergency department: rapid identification and treatment of patients with acute myocardial infarction. National Heart Attack Alert Program Coordinating Committee, 60 Minutes to Treatment Working Group. Ann Emerg Med. 1994;23:311–329. [PubMed] [Google Scholar]
- 14.Garvey JL, MacLeod BA, Sopko G, Hand MM National Heart Attack Alert Program (NHAAP) Coordinating Committee, National Heart, Lung, and Blood Institute (NHLBI), National Institutes of Health. Pre-hospital 12-lead electrocardiography programs: a call for implementation by emergency medical services systems providing advanced life support--National Heart Attack Alert Program (NHAAP) Coordinating Committee; National Heart, Lung, and Blood Institute (NHLBI); National Institutes of Health. J Am Coll Cardiol. 2006;47:485–491. doi: 10.1016/j.jacc.2005.08.072. [DOI] [PubMed] [Google Scholar]
- 15.Canto JG, Zalenski RJ, Ornato JP, Rogers WJ, Kiefe CI, Magid D, Shlipak MG, Frederick PD, Lambrew CG, Littrell KA, Barron HV National Registry of Myocardial Infarction 2 Investigators. Use of emergency medical services in acute myocardial infarction and subsequent quality of care: observations from the National Registry of Myocardial Infarction 2. Circulation. 2002;106:3018–3023. doi: 10.1161/01.cir.0000041246.20352.03. [DOI] [PubMed] [Google Scholar]
- 16.Concannon TW, Griffith JL, Kent DM, Normand SL, Newhouse JP, Atkins J, Beshansky JR, Selker HP. Elapsed time in emergency medical services for patients with cardiac complaints: are some patients at greater risk for delay? Circ Cardiovasc Qual Outcomes. 2009;2:9–15. doi: 10.1161/CIRCOUTCOMES.108.813741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Aguilar SA, Patel M, Castillo E, Patel E, Fisher R, Ochs G, Pringle J, Mahmud E, Dunford JV. Gender Differences in Scene Time, Transport Time, and Total Scene to Hospital Arrival Time Determined by the Use of a Prehospital Electrocardiogram in Patients with Complaint of Chest Pain. J Emerg Med. 2012;43:291–297. doi: 10.1016/j.jemermed.2011.06.130. [DOI] [PubMed] [Google Scholar]
- 18.Selker HP, Beshansky JR, Sheehan PR, Massaro JM, Griffith JL, D'Agostino RB, Ruthazer R, Atkins JM, Sayah AJ, Levy MK, Richards ME, Aufderheide TP, Braude DA, Pirrallo RG, Doyle DD, Frascone RJ, Kosiak DJ, Leaming JM, Van Gelder CM, Walter GP, Wayne MA, Woolard RH, Opie LH, Rackley CE, Apstein CS, Udelson JE. Out-of-Hospital Administration of Intravenous Glucose-Insulin-Potassium in Patients With Suspected Acute Coronary Syndromes: The IMMEDIATE Randomized Controlled Trial. JAMA. 2012;307:1925–1933. doi: 10.1001/jama.2012.426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Selker HP, Beshansky JR, Griffith JL, D'Agostino RB, Massaro JM, Udelson JE, Rashba EJ, Ruthazer R, Sheehan PR, Desvigne-Nickens P, Rosenberg YD, Atkins JM, Sayah AJ, Aufderheide TP, Rackley CE, Opie LH, Lambrew CT, Cobb LA, Macleod BA, Ingwall JS, Zalenski RJ, Apstein CS. Study design for the Immediate Myocardial Metabolic Enhancement During Initial Assessment and Treatment in Emergency Care (IMMEDIATE) Trial: A double-blind randomized controlled trial of intravenous glucose, insulin, and potassium for acute coronary syndromes in emergency medical services. Am Heart J. 2012;163:315–322. doi: 10.1016/j.ahj.2012.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Selker HP, Beshansky JR, Ruthazer R, Sheehan PR, Sayah AJ, Atkins JM, Aufderheide TP, Pirrallo RG, D'Agostino RB, Massaro JM, Griffith JL. Emergency medical service predictive instrument-aided diagnosis and treatment of acute coronary syndromes and ST-segment elevation myocardial infarction in the IMMEDIATE trial. Prehosp Emerg Care. 2011;15:139–148. doi: 10.3109/10903127.2010.545478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Goldberg RJ, Spencer FA, Fox KA, Brieger D, Steg PG, Gurfinkel E, Dedrick R, Gore JM. Prehospital Delay in Patients With Acute Coronary Syndromes (from the Global Registry of Acute Coronary Events [GRACE]) Am J Cardiol. 2009;103:598–603. doi: 10.1016/j.amjcard.2008.10.038. [DOI] [PubMed] [Google Scholar]
- 22.Goldberg RJ, Gurwitz JH, Gore JM. Duration of, and temporal trends (1994–1997) in, prehospital delay in patients with acute myocardial infarction: the second National Registry of Myocardial Infarction. Arch Intern Med. 1999;159:2141–2147. doi: 10.1001/archinte.159.18.2141. [DOI] [PubMed] [Google Scholar]
- 23.Goldberg RJ, Steg PG, Sadiq I, Granger CB, Jackson EA, Budaj A, Brieger D, Avezum A, Goodman S. Extent of, and factors associated with, delay to hospital presentation in patients with acute coronary disease (the GRACE registry) Am J Cardiol. 2002;89:791–796. doi: 10.1016/s0002-9149(02)02186-0. [DOI] [PubMed] [Google Scholar]
- 24.Canadian Cardiovascular Society, American Academy of Family Physicians, American College of Cardiology, American Heart Association. Antman EM, Hand M, Armstrong PW, Bates ER, Green LA, Halasyamani LK, Hochman JS, Krumholz HM, Lamas GA, Mullany CJ, Pearle DL, Sloan MA, Smith SC, Jr, Anbe DT, Kushner FG, Ornato JP, Pearle DL, Sloan MA, Jacobs AK, Adams CD, Anderson JL, Buller CE, Creager MA, Ettinger SM, Halperin JL, Hunt SA, Lytle BW, Nishimura R, Page RL, Riegel B, Tarkington LG, Yancy CW. 2007 focused update of the ACC/AHA 2004 guidelines for the management of patients with ST-elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2008;51:210–247. doi: 10.1016/j.jacc.2007.10.001. [DOI] [PubMed] [Google Scholar]
- 25.Goldberg RJ, Gurwitz JH, Gore JM. Duration of, and temporal trends (1994–1997) in, prehospital delay in patients with acute myocardial infarction: the second National Registry of Myocardial Infarction. Arch Intern Med. 1999;159:2141–2147. doi: 10.1001/archinte.159.18.2141. [DOI] [PubMed] [Google Scholar]
- 26.Meischke H, Eisenberg MS, Larsen MP. Prehospital delay interval for patients who use emergency medical services: the effect of heart-related medical conditions and demographic variables. Ann Emerg Med. 1993;22:1597–1601. doi: 10.1016/s0196-0644(05)81267-3. [DOI] [PubMed] [Google Scholar]
- 27.Ottesen MM, Kober L, Jorgensen S, Torp-Pedersen C. Determinants of delay between symptoms and hospital admission in 5978 patients with acute myocardial infarction. The TRACE Study Group. Trandolapril Cardiac Evaluation. Eur Heart J. 1996;17:429–437. doi: 10.1093/oxfordjournals.eurheartj.a014876. [DOI] [PubMed] [Google Scholar]
- 28.Ottesen MM, Dixen U, Torp-Pedersen C, Kober L. Prehospital delay in acute coronary syndrome--an analysis of the components of delay. Int J Cardiol. 2004;96:97–103. doi: 10.1016/j.ijcard.2003.04.059. [DOI] [PubMed] [Google Scholar]
- 29.Ting HH, Bradley EH, Wang Y, Lichtman JH, Nallamothu BK, Sullivan MD, Gersh BJ, Roger VL, Curtis JP, Krumholz HM. Factors associated with longer time from symptom onset to hospital presentation for patients with ST-elevation myocardial infarction. Arch Intern Med. 2008;168:959–968. doi: 10.1001/archinte.168.9.959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Peterson MC, Syndergaard T, Bowler J, Doxey R. A systematic review of factors predicting door to balloon time in ST-segment elevation myocardial infarction treated with percutaneous intervention. Int J Cardiol. 2012;157:8–23. doi: 10.1016/j.ijcard.2011.06.042. [DOI] [PubMed] [Google Scholar]