Abstract
Pectoralis major tendon ruptures can lead to significant functional deficits that affect high-level athletic and labor-intensive activities. In active populations operative repair of the ruptured pectoralis major tendon has shown significant advantages over nonoperative treatment. We describe a novel surgical technique for pectoralis major repair with tension button fixation. This study included 12 recreational athletes and 2 professional athletes. The initial results were measured subjectively after a minimum of 6 months by the Single Assessment Numeric Evaluation score, the American Shoulder and Elbow Surgeons score, and the ability to return to the patient's sport at a preinjury level. Objectively, strength was measured with resisted horizontal adduction of the arm for both repaired and contralateral sides. Of the 12 recreational patients, 8 returned to their sport at preinjury levels, and the 2 professional athletes returned to their sport at full capacity in the National Football League. The mean Single Assessment Numeric Evaluation score was 87, and the mean American Shoulder and Elbow Surgeons scores were 99 for both the operative and contralateral sides. Isokinetic strength testing showed no significant differences between the operative and nonoperative sides. Patients with pectoralis major tendons repaired with the proposed tensioned cortical button technique had excellent results. This new technique provides a reliable method of repair in an efficient and safe manner.
Ruptures of the pectoralis major tendon are rare and are most commonly associated with athletes (especially weightlifters) and heavy laborers.1,2 These injuries occur through an indirect mechanism such as forced abduction against resistance, high forces of traction on the arm, and involuntary contraction of the muscle.3-6 In weightlifters, particularly when bench pressing, the injury occurs during the eccentric phase of contraction as tension increases.4,7,8 Professional football players often incur this injury when an arm tackle is attempted on an opposing player. During rupture, patients will often report hearing or feeling a “pop” in their lateral chest wall or proximal arm.
Pectoralis major tendon ruptures most commonly occur at the tendinous insertion site on the humerus.3 Because the pectoralis major is a powerful adductor and internal rotator of the arm,1,9 rupture of the tendon can lead to significant functional deficits and impede high-level athletic or labor-intensive activities. In addition, rupture of the pectoralis major tendon leads to cosmetic deficits in the anterior axillary fold.
Low-demand individuals may be able to return to activities of daily living with nonoperative measures; however, athletes and laborers may not be able to return to their desired level of activity. In this latter group, operative management of a ruptured pectoralis major tendon has been shown to have significant clinical benefits over nonoperative management.3,10-12
Several surgical techniques to reattach the avulsed tendon back to its footprint in the humerus have been described in the literature. These techniques include transosseous sutures and bone troughs, suture anchors, and endosteal buttons.13-15 A biomechanical study performed by Sherman et al.14 has shown no significant differences in the techniques just described. Moreover, there are no studies in the literature showing any differences in clinical outcome among these techniques.
We present a surgical technique and initial results of patients who have undergone pectoralis major repairs (Table 1). Instead of using bone tunnels, which can act as stress risers in the humerus, our proposed technique uses a tendon-to-bone repair with tensioning button fixation at the footprint.
Table 1.
Pearls, Pitfalls and Risks, Key Points, Indications, and Contraindications
| Pearls |
| During drilling of the unicortical drill hole, the drill is slightly angled with respect to the humeral cortex to provide sufficient room in the intramedullary canal and thus aid in flipping the button. |
| Before repair fixation, the arm is placed into an adducted, neutral position. |
| The sternocostal head is repaired first, followed by the clavicular head. The sternocostal head insertion is posterior-superior relative to the clavicular head insertion. |
| A C-arm is used to confirm the final and correct positioning of the buttons. |
| Pitfalls and risks |
| An insufficient amount of bone bridge between each button placement site can increase the risk of fracture. |
| Implant cost is a consideration when using the cortical button method. |
| Cortical buttons may lead to metal artifact on postoperative magnetic resonance imaging studies. |
| Key points |
| In athletes and laborers, operative management of pectoralis major ruptures has been shown to have significant clinical benefits over nonoperative management. |
| Our technique uses a tendon-to-bone repair with tension button fixation at the footprint. |
| Bone trough fixation can lead to a higher propensity to fracture, which is a smaller risk with the cortical button technique. |
| The patient may return to collision sports at a minimum of 6 months after surgery, predicated on reaching each of the rehabilitation benchmarks, including sport- and position-specific components. |
| Indications |
| Insertional or intrasubstance pectoralis major tendon ruptures |
| Higher-demand individuals (athletes and laborers) |
| Cosmetic deformity of axillary fold |
| Contraindications |
| Pectoralis major muscle strains |
| Low-demand individuals (elderly persons, non-laborers, or sedentary individuals) |
| Comorbid factors that obviate the need for elective surgery |
Surgical Technique
Appropriate preoperative planning is conducted for every patient. This includes a thorough history and physical examination. A magnetic resonance imaging study will help delineate which heads of the pectoralis major tendon are involved, assess muscle quality, and determine the amount of retraction of the tendon (Video 1, Fig 1).
Fig 1.

Axial magnetic resonance image showing complete rupture of pectoralis major tendon.
A regional block is performed followed by beach-chair positioning with the arm placed in an arm positioner. An Ioban drape (3M, St. Paul, MN) is used to cover the operative area and seal the drapes around the involved arm and chest. A deltopectoral approach is performed, followed by elevation of flaps. Hemostasis is achieved with an electrocautery device. Blunt dissection is then performed to identify the pectoralis major tendon. Any soft-tissue adhesions are freed. Nonviable tissue is then debrided of the ruptured ends of the tendon. Each ruptured head of the pectoralis major tendon is secured with 2 sets of No. 2 FiberWire suture (Arthrex, Naples, FL) using a modified Krackow suture configuration. The No. 2 FiberWire stitches are placed on the superior and inferior aspects of the ruptured tendon head, respectively (Video 1, Fig 2).
Fig 2.
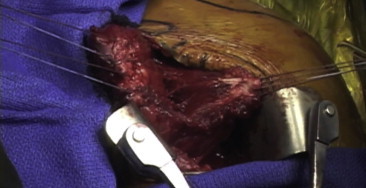
Exposure through a deltopectoral approach with the patient in the beach-chair position. Each ruptured head of the pectoralis major tendon is prepared with 2 sets of No. 2 FiberWire suture using a modified-Krackow suture configuration. The sternocostal head (right) and clavicular head (left) are shown.
A retractor is placed along the lateral aspect of the humeral shaft to retract the deltoid. The pectoralis major tendon footprint is then identified lateral to the bicipital groove. An electrocautery device is used to mark the button placement sites in a staggered fashion. A sufficient amount of bone bridge should be planned between each button placement site to avoid increasing the risk of fracture. Next, a 3.2-mm Drill Pin (Arthrex) is used to create a unicortical drill hole at each anchor site. During drilling, the drill is slightly angled with respect to the humeral cortex to provide sufficient room in the intramedullary canal and thus aid in flipping of the button.
The arm is placed into an adducted, neutral rotation position before fixation of the repair. The sternocostal head is repaired first, followed by the clavicular head. The repair is conducted in an anatomic fashion with the sternocostal head placed posteriorly and superiorly relative to the clavicular head. Each Distal Biceps Cortical Button (Arthrex) is threaded with each set of No. 2 FiberWire sutures coming from the pectoralis major tendon and inserted into each drill hole with the Button Inserter (Arthrex) (Fig 3). The button is then flipped within the intramedullary canal by pulling on the suture. Once each button is deployed, the button is provisionally tensioned along the footprint. Final tension is placed to reduce the tendon to its footprint, followed by standard knot-tying techniques (Fig 4).
Fig 3.
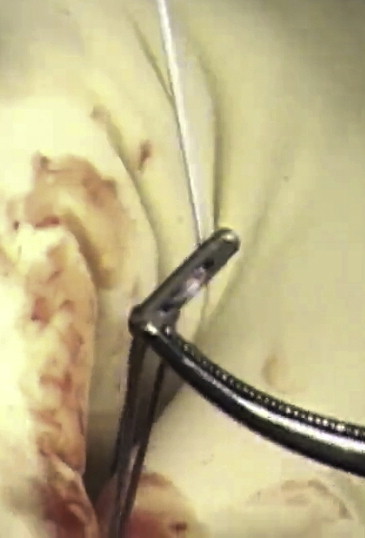
Distal Biceps Cortical Button loaded with No. 2 FiberWire suture, with each suture loaded in an opposite direction. After the buttons are loaded, they are placed on the endosteal surface of the humerus after a 3.2-mm drill is used to create a unicortical hole. These buttons are positioned in the humerus at the anatomic footprint of the pectoralis major tendon, lateral to the bicipital groove, in a staggered fashion.
Fig 4.
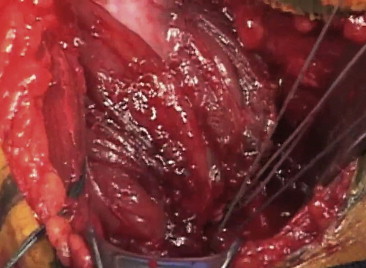
Once all of the Distal Biceps Cortical Buttons have been inserted into the humerus, the sutures undergo final tensioning to pull the tendon to the footprint. Once the tendon is fully reduced, the sutures are then tied down with standard knot-tying techniques. The excess suture is then cut, followed by irrigation and wound closure. It is advisable to obtain an intraoperative C-arm image of the fixation to ensure that the buttons are positioned correctly.
For a complete rupture, 2 buttons per head will be used, for a total of 4 buttons. A C-arm is used to confirm final and correct positioning of the buttons. After wound irrigation and closure, the patient is placed into a sling with the arm in an adducted position.
Postoperative Rehabilitation
The patient will remain in a sling for 4 to 6 weeks depending on the chronicity and quality of the tissue. The next 6 to 12 weeks will comprise progressively increasing range of motion and strengthening. The patient may return to collision sports at a minimum of 6 months after surgery, predicated on reaching each of the rehabilitation benchmarks, including sport- and position-specific components.
Clinical Results
Patients were enrolled between October 2009 and September 2012. There were 12 recreational athletes and 2 professional athletes in the study. The minimum follow-up was 6 months, and the mean follow-up was 12 months (Figs 5 and 6). The mean Single Assessment Numeric Evaluation score was 87 (range, 75 to 100), and the mean American Shoulder and Elbow Surgeons scores were 99 for both the operative (range, 93 to 100) and nonoperative (range, 94 to 100) sides, with no significant differences (P = .89). The average percent difference in isokinetic strength between the repaired side and the contralateral side was evaluated with the Nicholas Manual Muscle Tester (Lafayette Instrument Company, Lafayette, IN) performed with resisted horizontal adduction of the arm (with the shoulder in 90° of forward flexion and elbow in 90° of flexion). The average of 3 trials of isokinetic testing was used for evaluation. The average percent difference in isokinetic strength testing was 10.5%, with the operative side being weaker than the nonoperative side. This difference was not significant (P = .27). In addition, 8 of the 12 recreational athletes were able to return to their sport at the preinjury level. There were also 2 National Football League players in our study. One of these players had bilateral ruptures incurred at different times. Both players have returned to playing professional football at full capacity. There were no complications.
Fig 5.

Anteroposterior radiograph taken at follow-up showing intact positions of Distal Biceps Cortical Buttons.
Fig 6.

Patient at 1 year after left pectoralis major tendon repair. The intact cosmetic appearance of the anterior axillary fold, as well as the symmetry of the chest wall, should be noted.
Discussion
We describe a technique for repairing a ruptured pectoralis major tendon. This type of injury typically occurs in athletes such as weightlifters and football players, as well as heavy laborers. An intact and functional pectoralis major is very important to the profession and quality of life for this population. Thus it is important to restore the anatomy of the ruptured tendon to re-establish function to the athlete. A critical consideration in repairing the pectoralis major tendon is to ensure that the sternal head is placed posterior and superior relative to the insertion of the clavicular head.13
The literature describes several techniques for fixation of the ruptured pectoralis major tendon. A biomechanical study by Sherman et al.14 included 24 pectoralis major cadaveric specimens. These specimens were divided into 4 different groups based on fixation method, consisting of an intact group, Pec Button (Arthrex) group, transosseous suture group, and suture anchor group. A modified Mason-Allen suture configuration was used to secure the tendon. Load-to-failure testing showed no significant differences among the different fixation methods. However, all repair constructs had inferior maximum load-to-failure results compared with the intact state. Rabuck et al.16 conducted a cadaveric study with 30 specimens. They studied 3 different groups based on fixation method: a bone trough group, a cortical button group, and a suture anchor group. Load-to-failure testing showed no statistical differences between the bone trough group and the cortical button group. However, the bone trough group had a higher maximum load-to-failure than the suture anchor group. On the other hand, the authors did report failure in 1 specimen in the bone trough group due to fracture.
The bone trough fixation method has been widely used but does yield a higher propensity for fracture than other methods.17 It also takes more time to perform this fixation method than the cortical button method. Another advantage of the cortical button method is that it allows the surgeon to pull the tendon to the footprint, rather than pushing it to the footprint. We believe that this has a greater potential biomechanical advantage over other methods. However, the potential disadvantages of using the cortical button method include the added cost for the implant and metal artifact on magnetic resonance imaging studies that may be obtained in the future.
Conclusion
Our patients who have undergone pectoralis major repairs with the described surgical technique, using tensioning cortical buttons, had excellent results. This technique is reproducible and provides a reliable method of repairing pectoralis major ruptures without the use of bone tunnels. Biomechanical studies are needed to compare this technique with other documented repair techniques.
Footnotes
The authors report that they have no conflicts of interest in the authorship and publication of this article.
Supplementary Data
Surgical technique for repairing complete rupture of pectoralis major tendon. The patient is a 31-year-old man with a chronic pectoralis major tendon rupture due to a bench-pressing incident. This technique is performed with 4 Arthrex distal biceps buttons. These are placed just lateral to the bicipital groove in a staggered fashion.
References
- 1.Provencher M.T., Handfield K., Boniquit N.T. Injuries to the pectoralis major muscle: Diagnosis and management. Am J Sports Med. 2010;38:1693–1705. doi: 10.1177/0363546509348051. [DOI] [PubMed] [Google Scholar]
- 2.Cordasco F.A., Delos D. Pectoralis major rupture: Diagnosis and treatment. In: Iannnotti J.P., Miniaci A., Williams G.R., Zuckerman J.D., editors. Disorders of the shoulder: Diagnosis and management. Volume II: Shoulder sports injuries. Ed 3. Lippincott Williams & Wilkins; Philadelphia: 2013. pp. 373–380. [Google Scholar]
- 3.Bak K., Cameron E.A., Henderson I.J. Rupture of the pectoralis major: A meta-analysis of 112 cases. Knee Surg Sports Traumatol Arthrosc. 2000;8:113–119. doi: 10.1007/s001670050197. [DOI] [PubMed] [Google Scholar]
- 4.Wolfe S.W., Wickiewicz T.L., Cavanaugh J.T. Rupture of the pectoralis major muscle: An anatomic and clinical analysis. Am J Sports Med. 1992;20:587–593. doi: 10.1177/036354659202000517. [DOI] [PubMed] [Google Scholar]
- 5.Kretzler H.H., Jr., Richardson A.B. Rupture of the pectoralis major muscle. Am J Sports Med. 1989;17:453–458. doi: 10.1177/036354658901700401. [DOI] [PubMed] [Google Scholar]
- 6.Tietjen R. Closed injuries of the pectoralis major muscle. J Trauma. 1980;20:262–264. doi: 10.1097/00005373-198003000-00015. [DOI] [PubMed] [Google Scholar]
- 7.Garrett W.E., Jr. Muscle strain injuries: Clinical and basic aspects. Med Sci Sports Exerc. 1990;22:436–443. [PubMed] [Google Scholar]
- 8.Garrigues G.E., Kraeutler M.J., Gillespie R.J., O’Brien D.F., Lazarus M.D. Repair of pectoralis major ruptures: Single-surgeon case series. Orthopedics. 2012;35:e1184–e1190. doi: 10.3928/01477447-20120725-17. [DOI] [PubMed] [Google Scholar]
- 9.Iannotti J.P., Williams G.R. Traumatic muscle ruptures. In: Iannotti J.P., Williams G.R., editors. Disorders of the shoulder: Diagnosis and management. Lippincott Williams & Wilkins; Philadelphia: 1999. pp. 191–197. [Google Scholar]
- 10.Hanna C.M., Glenny A.B., Stanley S.N., Caughey M.A. Pectoralis major tears: Comparison of surgical and conservative treatment. Br J Sports Med. 2001;35:202–206. doi: 10.1136/bjsm.35.3.202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.de Castro Pochini A., Ejnisman B., Andreoli C.V. Pectoralis major muscle rupture in athletes: A prospective study. Am J Sports Med. 2010;38:92–98. doi: 10.1177/0363546509347995. [DOI] [PubMed] [Google Scholar]
- 12.He Z.M., Ao Y.F., Wang J.Q., Hu Y.L., Yin Y. Twelve cases of the pectoralis major muscle tendon rupture with surgical treatment—An average of 6.7-year follow-up. Chin Med J (Engl) 2010;123:57–60. [PubMed] [Google Scholar]
- 13.Petilon J., Carr D.R., Sekiya J.K., Unger D.V. Pectoralis major muscle injuries: Evaluation and management. J Am Acad Orthop Surg. 2005;13:59–68. doi: 10.5435/00124635-200501000-00008. [DOI] [PubMed] [Google Scholar]
- 14.Sherman S.L., Lin E.C., Verma N.N. Biomechanical analysis of the pectoralis major tendon and comparison of techniques for tendo-osseous repair. Am J Sports Med. 2012;40:1887–1894. doi: 10.1177/0363546512452849. [DOI] [PubMed] [Google Scholar]
- 15.Metzger P.D., Bailey J.R., Filler R.D., Waltz R.A., Provencher M.T., Dewing C.B. Pectoralis major muscle rupture repair: Technique using unicortical buttons. Arthrosc Tech. 2012;1:e119–e125. doi: 10.1016/j.eats.2012.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rabuck S.J., Lynch J.L., Guo X. Biomechanical comparison of 3 methods to repair pectoralis major ruptures. Am J Sports Med. 2012;40:1635–1640. doi: 10.1177/0363546512449291. [DOI] [PubMed] [Google Scholar]
- 17.Silverstein J.A., Goldberg B., Wolin P. Proximal humerus shaft fracture after pectoralis major tendon rupture repair. Orthopedics. 2011;34:222. doi: 10.3928/01477447-20110427-24. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Surgical technique for repairing complete rupture of pectoralis major tendon. The patient is a 31-year-old man with a chronic pectoralis major tendon rupture due to a bench-pressing incident. This technique is performed with 4 Arthrex distal biceps buttons. These are placed just lateral to the bicipital groove in a staggered fashion.


