Abstract
Arthroscopic labral repair is an effective technique for most cases of traumatic shoulder instability. However, patients with anterior labroligamentous periosteal sleeve avulsion lesions frequently have multiple episodes of subluxation or dislocation and a high recurrence rate after surgery, even with modern methods of labral repair. One reason may be failure of biological healing of the labrum due to an inadequate “footprint” of contact between the capsulolabral tissue and the glenoid bone. We have developed a technique that facilitates a tensioned suture bridge between suture anchors that may improve the results of labral repair in patients with anterior labroligamentous periosteal sleeve avulsion lesions.
Arthroscopic anterior labral repair is a well-established procedure and has been shown to be superior to nonoperative treatment, especially for young male patients with traumatic instability of the shoulder.1 Although the Bankart lesion (detachment of the labrum from the anterior glenoid margin) is regarded as the “essential” lesion of instability and is evident in the vast majority of cases,2 it is recognized that there is a spectrum of other pathologic lesions of the soft tissues of the shoulder, including superior labral tears (SLAP lesions), humeral avulsion of the glenohumeral ligaments, and anterior labroligamentous periosteal sleeve avulsion (ALPSA) lesions.2,3 In the ALPSA lesion (Fig 1), the entire capsulolabral complex becomes detached from its insertion and heals more medially on the anterior aspect of the glenoid neck, exposing the underlying bone.4 Recently, studies have shown that the presence of an ALPSA lesion is more common in younger patients (aged <25 years) and is associated with a higher frequency of preoperative dislocation episodes and a higher rate of recurrence after arthroscopic surgery.5,6 Although the cause of ALPSA lesions is not yet clear, the high recurrence rate after surgery may reflect the relative lack of a “periosteal hinge” along the glenoid neck. In simple terms, when a Bankart lesion is reattached with suture anchors along the anterior glenoid margin, the intact periosteum serves to provide a wide “footprint” of contact between the soft tissue and bone for biological healing to occur (Fig 2A). However, during mobilization of an ALPSA lesion, it is evident that the periosteal hinge is usually absent or is collapsed and deficient. As a result, labral repair with suture anchors is dependent on “rim fixation” over a narrower and smaller surface area adjacent to the articular margin (Fig 2B). The reduction in surface area for healing of soft tissue to bone may, in part, explain the higher recurrence rates after patients return to competitive sports. Double-row suture anchor repair (similar in concept to contemporary arthroscopic methods of rotator cuff repair) has been proposed as a possible solution to improve the footprint of healing along the glenoid neck,7 but it may be difficult to achieve within the confined space of the glenohumeral joint. We have developed a novel technique, deploying a new suture anchor that facilitates a tensioned suture bridge between anchors, that improves fixation of the labrum and contact of tissue to bone and may address this problem.
Fig 1.

Arthroscopic view of glenoid from anterior portal, showing an ALPSA lesion adherent medially with exposure of the glenoid neck and articular margin.
Fig 2.
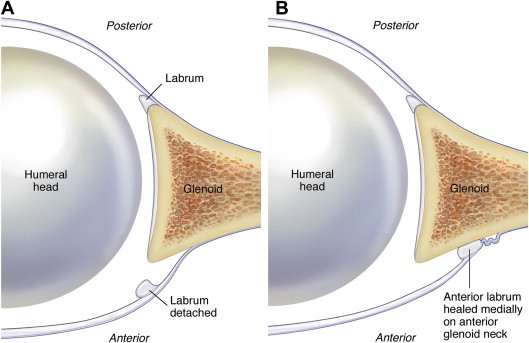
(A) Axial schematic view of a Bankart lesion showing the intact periosteal hinge available for healing along the glenoid neck after the labrum is reattached. (B) Axial schematic view of an ALPSA lesion. The medial periosteal hinge has been collapsed and will be divided as the labrum is mobilized and restored to the glenoid margin.
Surgical Technique
The patient is placed on the operating table in the beach-chair position with the arm draped freely. Translation of the glenohumeral joint is assessed in different positions of arm abduction and rotation to determine the degree and direction of instability and the presence of an engaging Hill-Sachs lesion.
The arthroscope is inserted into the glenohumeral joint through a standard posterior viewing portal. An anterior working portal is created over the superior edge of the subscapularis tendon as laterally as possible. An 8.5-mm cannula is inserted and a probe introduced to assess the integrity of the labrum. The entire joint is inspected thoroughly to exclude associated superior or posterior labral lesions, humeral avulsion of the glenohumeral ligament lesions, chondral defects, or cuff tears. Relative contraindications to this technique include an “inverted-pear” sign, indicative of inferior glenoid bone deficiency, and a Hill-Sachs lesion that engages with the anterior glenoid rim on abduction of the arm.8
An additional anterosuperior working portal is created superiorly in the rotator interval, and a 7-mm cannula is inserted. By use of a sharp periosteal elevator, the entire capsulolabral complex is fully mobilized medially from the base of the glenoid neck. Care should be taken to adequately release all capsular adhesions so that the fibers of the underlying subscapularis muscle can be visualized. Next, the bony surface of the exposed anterior glenoid neck is abraded to a bleeding surface with a soft-tissue shaver or a bony burr. A 2.9-mm flat-tipped drill bit is inserted through a crown-tipped drill guide through the anterior portal. Holes are drilled into the margin of the glenoid at the 1-, 3-, and 5-o'clock positions. A nonabsorbable suture is passed through the labrum opposite the 5-o'clock drill hole using a suture-passing device and suture shuttle, and the suture ends are retrieved through the anterior portal (Table 1). The 2 free ends of the suture are loaded into the eyelet of a Bioraptor Knotless suture anchor (Smith & Nephew, Andover, MA), which is driven into the bone. This anchor, fabricated from poly ether ether ketone, has the facility for clamping sutures in the eyelet by deployment of a small screw located in the apex of the anchor. The suture is tensioned and clamped in the anchor, and the inserter is removed. Only 1 of the suture limbs is divided, whereas the remaining suture limb is temporarily retrieved and “parked” in the anterosuperior portal. The same procedure is repeated for the 1-o'clock anchor. A suture shuttle device (Accu-Pass; Smith & Nephew) or suture retriever is then used to retrieve the remaining suture limb under the labrum adjacent to the 1- and 5-o'clock anchors, exiting through the anterior portal (Fig 3A, Video 1). The suture shuttle device is used to pass a suture loop by penetrating the capsule medial to the labrum opposite the 3-o'clock anchor (Fig 3B). The 2 suture limbs are then shuttled through the labrum and retrieved back through the anterior portal. The 2 sutures are passed through the eyelet of a third Bioraptor Knotless anchor, which is then inserted into the 3-o'clock drill hole. The suture limbs from the 1- and 5-o'clock anchors are tensioned by traction on the suture ends. Once satisfactory tensioning of the resulting suture bridge is completed, the torque-limiting knob on the end of the insertion device is turned, engaging the screw in the apex of the anchor, clamping the sutures in the anchor eyelet. The insertion device is removed, and the suture ends are cut flush with the labrum, completing the repair (Fig 4). When viewed from the posterior portal, a good bumper of labral tissue should be evident, and when the arm is moved into 30° of abduction, additional external rotation results in reconstitution of the “hammock” effect of the inferior glenohumeral ligament. When viewed from the anterior portal, the tensioned suture bridge between the anchor sites is clearly seen (Fig 5), with the 2 limbs of the repair being reminiscent of a swan in flight (Fig 6).
Table 1.
Summary of Key Points
| Pass the sutures and insert the anchors at the 1- and 5-o'clock positions. |
| Cut only 1 suture limb at each anchor. |
| Tunnel the suture limbs back under the labrum, adjacent to each anchor, from the glenoid to capsular side. |
| Shuttle the 2 suture limbs from the capsular to glenoid side at the 3-o'clock position. |
| Retrieve the sutures, and load and insert the anchor at the 3-o'clock position. |
| Perform final tensioning of the suture bridge before clamping in the anchor. |
Fig 3.
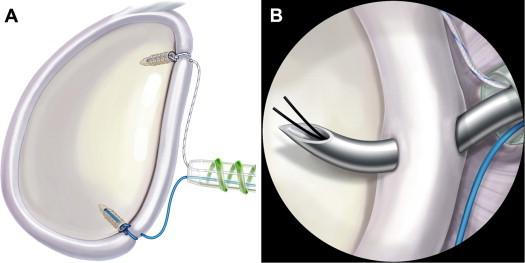
Sagittal schematic view of glenoid. (A) The single suture limbs from both the 1- and 5-o'clock anchors have been tunneled back under the labrum and out the anterior portal. After (B) passage of a suture shuttle using the Accu-Pass device at the 3-o'clock position, these suture limbs will be passed through the labrum and loaded onto the Bioraptor Knotless anchor for final tensioning after the anchor is deployed.
Fig 4.
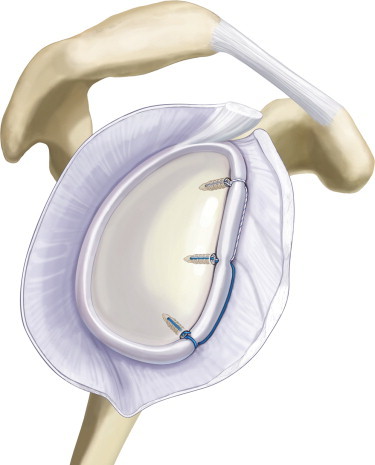
Sagittal schematic view of completed flying swan tensioned suture bridge between 3 anchors.
Fig 5.
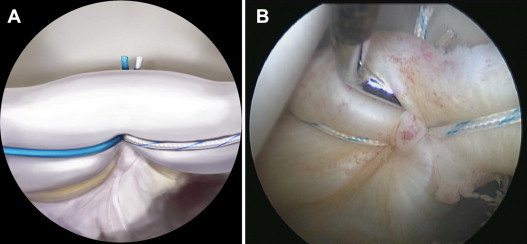
Schematic (A) and arthroscopic (B) views from anterior portal of repaired labrum, showing the buttress effect of the technique with the tensioned suture strands visible medially along the glenoid neck.
Fig 6.

The pattern of sutures in the tensioned suture bridge technique resembles the wings of a flying swan when viewed from the front.
Discussion
Conventional methods of arthroscopic labral repair rely on the deployment of anchors at intervals along the glenoid margin, with sutures passed around the labrum and secured either with hand-tied knots or by various knotless anchor designs based on suture loops or interference fit. The net effect of a standard Bankart repair is to create a series of “spot welds” holding the repaired labrum in position until biological healing occurs. However, even with careful immobilization in a sling after surgery, it is possible that cyclic motion of the labrum occurs, leading to the formation of gaps between the labrum and glenoid bone in the intervals between the anchors. In the presence of an ALPSA lesion, such gap formation may compound the rim fixation effect and increase the risk of failure of the repair by reducing the available surface for biological healing. Our technique relies on the creation of a “double-mattress” suture bridge medial to the glenoid margin that reinforces the buttress effect of the labrum and improves contact between the capsulolabral tissue and the underlying bone between the anchors. Although any of a number of anchor designs can be used for fixation at the 1- and 5-o'clock positions, the Bioraptor Knotless anchor is useful for accurate tensioning of each of the suture limbs, independent of the placement of the anchor in the bone. More research on the biomechanical advantages of this technique is required, but it holds promise in trying to improve the clinical outcome of patients with ALPSA lesions.
Footnotes
The authors report the following potential conflict of interest or source of funding: S.A. receives support from Smith & Nephew; A.L.W. receives support from Hospital of St. John & St. Elizabeth and Smith & Nephew.
Supplementary Data
The key steps of establishing a tensioned suture bridge are highlighted, after deployment of anchors at the 1- and 3-o'clock positions. One limb from each suture anchor is cut, preserving 1 limb for the suture bridge. To achieve this technique, any anchor system that facilitates a simple suture around the labrum at the 1- and 3-o'clock positions can be used. The video describes in detail the suture passage technique and the final tensioning of the key Bioraptor Knotless anchor at the 3-o'clock position. The tensioning of the suture bridge is independent of the placement or position of the anchor in the underlying glenoid bone.
References
- 1.Robinson C.M., Jenkins P.J., White T.O., Ker A., Will E. Primary arthroscopic stabilization for a first-time anterior dislocation of the shoulder: A randomized, double-blind trial. J Bone Joint Surg Am. 2008;90:708–721. doi: 10.2106/JBJS.G.00679. [DOI] [PubMed] [Google Scholar]
- 2.Kim D.-S., Yoon Y.-S., Yi C.H. Prevalence comparison of accompanying lesions between primary and recurrent anterior dislocation in the shoulder. Am J Sports Med. 2010;38:2071–2076. doi: 10.1177/0363546510371607. [DOI] [PubMed] [Google Scholar]
- 3.Yiannakopoulos C.K., Mataragas E., Antonogiannakis E. A comparison of the spectrum of intra-articular lesions in acute and chronic anterior shoulder instability. Arthroscopy. 2007;23:985–990. doi: 10.1016/j.arthro.2007.05.009. [DOI] [PubMed] [Google Scholar]
- 4.Neviaser T.J. The anterior labroligamentous periosteal sleeve avulsion lesion: A cause of anterior instability of the shoulder. Arthroscopy. 1993;9:17–21. doi: 10.1016/s0749-8063(05)80338-x. [DOI] [PubMed] [Google Scholar]
- 5.Ozbaydar M., Elhassan B., Diller D., Massimini D., Higgins L.D., Warner J.J.P. Results of arthroscopic capsulolabral repair: Bankart lesion versus anterior labroligamentous periosteal sleeve avulsion lesion. Arthroscopy. 2008;24:1277–1283. doi: 10.1016/j.arthro.2008.01.017. [DOI] [PubMed] [Google Scholar]
- 6.Lee B.G., Cho N.S., Rhee Y.G. Anterior labroligamentous periosteal sleeve avulsion lesion in arthroscopic capsulolabral repair for anterior shoulder instability. Knee Surg Sports Traumatol Arthrosc. 2011;19:1563–1569. doi: 10.1007/s00167-011-1531-z. [DOI] [PubMed] [Google Scholar]
- 7.Ahmad C.S., Galano G.J., Vorys G.C., Covey A.S., Gardner T.R., Levine W.N. Evaluation of glenoid capsulolabral complex insertional anatomy and restoration with single- and double-row capsulolabral repairs. J Shoulder Elbow Surg. 2009;18:948–954. doi: 10.1016/j.jse.2009.03.022. [DOI] [PubMed] [Google Scholar]
- 8.Burkhart S.S., De Beer J.F. Traumatic glenohumeral bone defects and their relationship to failure of arthroscopic Bankart repairs: Significance of the inverted-pear glenoid and the humeral engaging Hill-Sachs lesion. Arthroscopy. 2000;16:677–694. doi: 10.1053/jars.2000.17715. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The key steps of establishing a tensioned suture bridge are highlighted, after deployment of anchors at the 1- and 3-o'clock positions. One limb from each suture anchor is cut, preserving 1 limb for the suture bridge. To achieve this technique, any anchor system that facilitates a simple suture around the labrum at the 1- and 3-o'clock positions can be used. The video describes in detail the suture passage technique and the final tensioning of the key Bioraptor Knotless anchor at the 3-o'clock position. The tensioning of the suture bridge is independent of the placement or position of the anchor in the underlying glenoid bone.


