Abstract
A 30-year-old man who incidentally fractured his right olecranon and other multiple phalanges was admitted to our hospital. He had a 2-year history of uveitis and bilateral hilar lymphadenopathy (BHL), and pulmonary sarcoidosis was diagnosed from transbronchial lung biopsy. Right elbow arthrodesis was performed, and biopsied specimens showed non-caseating epithelioid cell granuloma, suggesting osseous sarcoidosis. He was discharged uneventfully without further treatment, but BHL had progressed with the appearance of lung parenchymal lesions 3 months later. At that time, involvement of other organs was also noted on Gallium-67 scintigraphy, showing accumulations in BHL, axillary and inguinal lymph nodes, enlarged liver and spleen and subcutaneous areas. After initiation of steroid therapy, multiple organ involvement improved, and no further bone involvement has been recognised to date. Osseous sarcoidosis complicated by bone fracture is an extremely rare presentation, but should be considered in patients with sarcoidosis, especially when multiple organs are involved.
Background
Sarcoidosis is a systemic disease, and the frequency of osseous sarcoidosis is 1–13%, but bone fracture is extremely rare. To the best of our knowledge, only 23 cases have been reported so far. We describe a case of osseous sarcoidosis with multiple organ involvement and review the literature for this pathology associated with bone fracture.
Case presentation
A 30-year-old man was admitted to our orthopaedics ward because of sudden fracture of the right olecranon when he turned to speak to his friends. Two years previously, he had been diagnosed with pulmonary sarcoidosis based on findings of non-caseating epithelioid cell granuloma on transbronchial lung biopsy. He had uveitis and bilateral hilar lymphadenopathy (BHL) on chest X-ray, but had been in good health until then without any treatments during his regular visits to our hospital.
Vital signs and physical examination were normal except for swelling in the area of the right olecranon. Lateral radiography of the right elbow showed the fracture line at the right olecranon (figure 1A; white arrowhead) with cystic lesions, suggesting osteolytic changes. Furthermore, radiography showed multiple osseous erosions (figure 1B,C; arrow) with osteolytic lesions, and fractures of the middle phalanx of the left digitus minimus manus (figure 1B; white arrowhead) and base of the left metacarpal bone of digitus annularis (figure 1B; black arrowhead).
Figure 1.
Lateral radiograph of the right elbow showing the fracture line at the right olecranon (A; white arrowhead) with cystic lesions, suggesting osteolytic changes. Furthermore, radiographs showing multiple osseous erosions (B and C; arrow) with osteolytic lesions, fractures on the middle phalanx of the left digitus minimus manus (B; white arrowhead) and base of the left metacarpal of digitus annularis (B; black arrowhead). Axial T1-weighted imaging (T1WI) demonstrates a low-intensity intramedullary mass measuring 2 cm in the right olecranon (D), appearing hyperintense on axial T2WI (E) and enhancing heterogeneously on fat-suppressed enhanced T1WI (F).
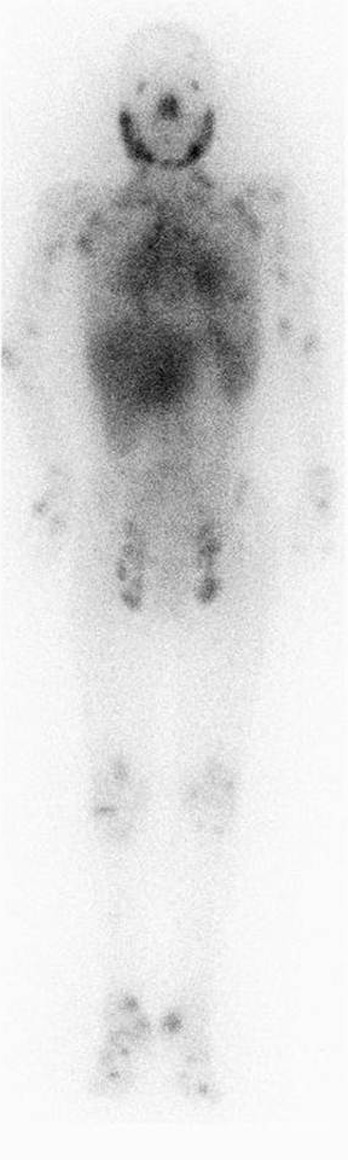
Axial T1-weighted imaging (T1WI) demonstrated a low-intensity intramedullary mass measuring 2 cm in the right olecranon (figure 1D), which appeared hyperintense on axial T2WI (figure 1E) and heterogeneously enhancing on fat-suppressed enhanced T1WI (figure 1F). Tc-99m methylene diphosphonate bone scintigraphy showed multiple hot spots on the left parietal bone, middle thoracic spine, bilateral cubital regions, wrists and knees, and below bilateral ankle joints (figure 2).
Figure 2.

Tc-99m methylene diphosphonate bone scintigraphy showing multiple hot spots on the left parietal bone, middle thoracic spine, cubital regions, wrists and knees, and below bilateral ankle joints.
Right elbow arthrodesis was performed and biopsy specimens showed non-caseating epithelioid cell granuloma on both low-power (figure 3A) or high-power fields (figure 3B). Osseous sarcoidosis with multiple organ involvement was diagnosed and he was discharged uneventfully with no further treatment. Three months later, he presented to our respiratory department with progression of BHL and newly recognised pulmonary involvement with bilateral pleural effusion. Chest X-ray showed BHL with perihilar infiltration and dullness of the left costophrenic angle (figure 4A). Thoracic CT demonstrated consolidation spreading from hilar to peripheral areas showing multiple scattered tiny nodules with bilateral pleural effusions (figure 4B). Gallium-67 scintigraphy showed increased radiotracer accumulation in the lacrimal and parotid glands and normal accumulation in the nasopharynx, creating the mottled appearance of a giant panda, the so-called panda sign. Increased radiotracer accumulation was noted in BHL, axillary and inguinal lymph nodes, subcutaneous nodules, lung parenchyma, enlarged liver and spleen and subcutaneous areas (figure 5). Furthermore, cardiac echography showed interventricular septal thinning and erythema nodosum was noted. Finally, osseous sarcoidosis accompanied by multiple organ involvements (eye, heart, skin, lungs, lymph nodes, liver and spleen) was diagnosed.
Figure 3.
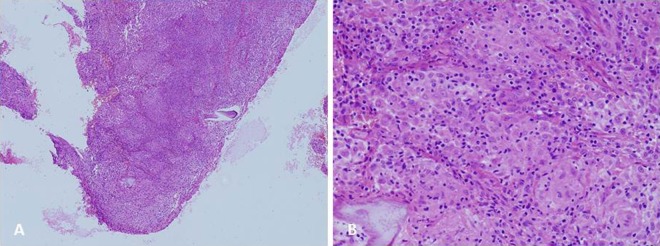
Biopsied specimens obtained from right elbow arthrodesis showing non-caseating epithelioid cell granuloma on both low-power (A) and high-power fields (B).
Figure 4.
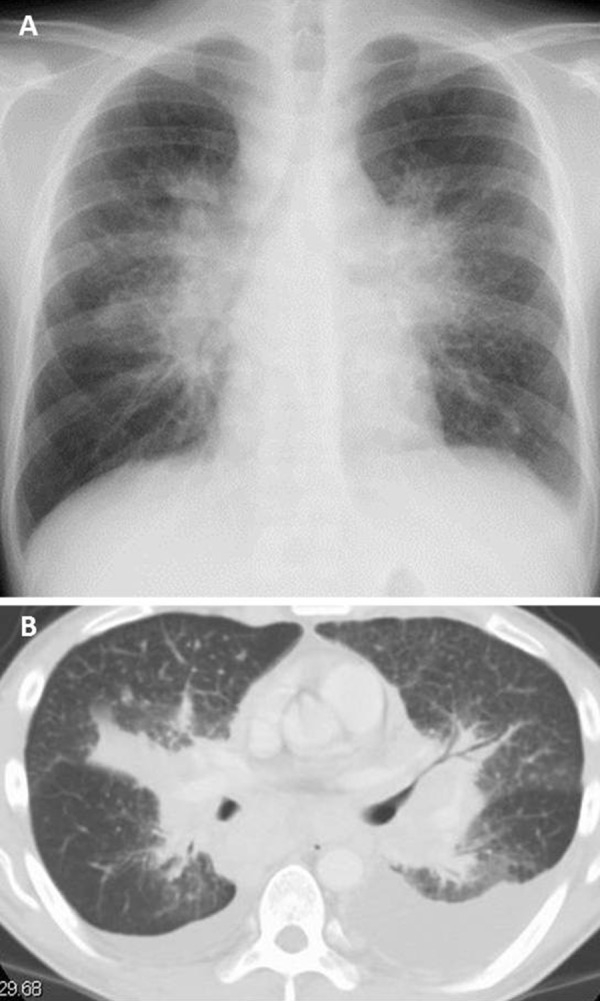
Chest X-ray showing bilateral hilar lymphadenopathy (BHL) with perihilar infiltration and dullness of the left costophrenic angle (A). Thoracic CT depicts massive consolidation from hilar to peripheral portion with bilateral pleural effusions and multiple scattered tiny nodules (B).
Figure 5.
Gallium-67 scintigraphy showing increased radiotracer accumulation in the lacrimal and parotid glands, the so-called panda sign. Increased radiotracer accumulation was noted in BHL, axillary and inguinal lymph nodes, subcutaneous nodules, lung parenchyma, enlarged liver and spleen and subcutaneous areas.
Treatment
Multiple organ involvement including pulmonary lesions was considered to represent sarcoidosis, and the patient was treated with prednisolone at a dose of 0.5 mg/kg/day.
Outcome and follow-up
After initiation of treatment, multiple subcutaneous nodules and lymphadenopathies disappeared, and almost all lung lesions were improved. No further bone involvement has been recognised to date.
Discussion
Sarcoidosis is a systemic disease, and the frequency of osseous sarcoidosis ranges from 1% to 13%.1 Radiological features of osseous sarcoidosis include osteolytic lesions, bone erosions, and a lacework pattern, which show a predilection for small bones in the hands and feet,2 as in the present case.
To the best of our knowledge, only 24 cases of bone fracture with sarcoidosis have been reported2–21 including the present case (table 1). The patients were of the age group ranging from 15 to 59 years old (mean±SD 37.8±12.2 years), with a male-to-female ratio of 9–15. Among these, racial diversity was noted, but people of African descent/origin (n=8) and Asian patients all of whom were Japanese (n=9) appear as prominent populations. Although few reports have described the racial incidence of bone fractures in patients with osseous sarcoidosis, Handa et al3 indicated that people of African descent/origin tended to experience bone fractures, with no mention of Japanese cases. Our results suggest that the number of Japanese cases was equal to that of African descent/origin people. In our review, the areas of bone involvement were the phalanges (n=15), joints (n=5), vertebrae (n=4) and others (n=2), respectively. This means the phalanges were the most affected by bone fracture in osseous sarcoidosis, like our case. O’Daly et al4 described the incidence of osseous involvement as low in patients with early-stage sarcoidosis and absence of cutaneous lesions. Indeed, the present case had sudden bone fractures 2 years after diagnosis of sarcoidosis together with subcutaneous nodules. While, our review showed insidious onset of bone fracture in the clinical course (median: 0.95 years) after diagnosis of sarcoidosis (table 1) with or without skin involvement.
Table 1.
| Reference | Age (years) | Sex | Race | Bone | Duration (years) | New diagnosis | Atraumatic | Operation | Medication | Multiple organ involvement | Number of organs involved except for bone |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 2 | 55 | M | NA, not applicable | Vertebra | NA, not applicable | N | Y | Y | PSL | Y | 3 |
| 3 | 22 | M | Japanese | Phalange | 7 | N | Y | N | PSL+MTX | Y | 2 |
| 4 | 39 | F | Black | Joint | 0.08 | N | N | Y | PSL | Y | 2 |
| 5 | 31 | F | Black | Joint | 3 | N | N | Y | PSL | Y | 2 |
| 6 | 26 | M | Black | Vertebra | 2 | N | NA, not applicable | Y | PSL | Y | 1 |
| 7 | 27 | F | Black | Rib | 0 | Y | N | N | PSL | Y | 2 |
| 8 | 36 | F | Black | Phalange | 1 | N | NA, not applicable | Y | PSL | Y | 1 |
| 8 | 19 | M | Black | Joint | NA, not applicable | N | NA, not applicable | Y | None | NA, not applicable | NA, not applicable |
| 9 | 59 | F | NA | Phalange | 0 | Y | Y | N | PSL | N | 0 |
| 10 | 29 | M | Black | Phalange | 0 | Y | N | N | None | Y | 1 |
| 11 | 49 | F | Japanese | Phalange | 0 | Y | Y | Y | PSL | N | 0 |
| 11 | 35 | M | Japanese | Phalange | 6 | N | N | Y | None | Y | 2 |
| 11 | 43 | F | Japanese | Phalange | 32 | N | Y | Y | PSL | Y | 3 |
| 12 | 48 | F | NA | Phalange | 0 | Y | Y | Y | PSL | N | 0 |
| 13 | 25 | F | Moroccan | Phalange | 2 | N | Y | Y | None | Y | 2 |
| 14 | 59 | F | Japanese | Phalange | 0.5 | N | Y | Y | None | Y | 1 |
| 15 | 38 | F | Black | Phalange | 12 | N | Y | Y | PSL | Y | 2 |
| 16 | 45 | F | Portugese | Femur, Ulna | 0 | Y | NA, not applicable | Y | None | N | 0 |
| 17 | 55 | M | Japanese | Vertebra | 3 | N | Y | Y | PSL | Y | 2 |
| 18 | 34 | M | Japanese | Phalange | 0 | Y | N | Y | PSL | Y | 6 |
| 19 | 36 | F | NA, not applicable | Vertebra | 0.9 | N | Y | N | PSL+CQ | Y | 3 |
| 20 | 52 | F | NA, not applicable | Phalange | 0 | Y | Y | Y | PSL | Y | 4 |
| 21 | 15 | F | Japanese | Phalange | 2 | N | Y | Y | PSL | Y | 2 |
| Present case | 30 | M | Japanese | Joint, Phalange | 2 | N | Y | Y | PSL | Y | 5 |
Interestingly, new diagnosis of sarcoidosis due to bone fracture was found in 33.3% (n=8) of all cases. The precise mechanism of bone fracture in patients with sarcoidosis is unknown. Importantly, 70% (n=14) of the 20 cases for whom records are available showed bone fracture with no apparent traumatic events and none of them had obvious clinical findings for bone involvement, as was the present case. Although predicting the possibility for bone fracture is difficult, multiple bone scans might be useful for detecting undiscovered bone involvement in whole body even in patients with asymptomatic osseous sarcoidosis, and accumulation of such cases might lead to evaluate the efficacy of treatments via comparing the two phases (pretreatment and posttreatment). The appropriate treatment for bone fracture in sarcoidosis remains contentious. Furthermore, corticosteroids have not been shown to influence the clinical course of osseous sarcoidosis.22 The present study showed that 75.0% (n=18) of patients were treated with oral steroids with or without other drugs (methotrexate, n=1; chloroquine, n=1), and orthopaedic operation was performed in 79.2% (n=19) of all patients.
In our review, multiple organ involvement was noted in 79.2% (n=19) of all cases, potentially representing a risk factor for bone fracture in sarcoidosis, as reported by a previous study.3
Given these findings, the possibility of bone fracture should always be considered in sarcoidosis patients with various clinical findings via multiple organ involvement. Our case and review of the literatures demonstrated that the incidence of osseous sarcoidosis among Japanese patients seemed to be greater than that of previous recognition.
Learning points.
Frequency of osseous sarcoidosis is 1–13%, but bone fracture is rare.
Bone fracture can be an initial presentation of sarcoidosis.
The phalanges are the part most affected by bone fracture in osseous sarcoidosis.
The precise mechanisms of bone fracture in patients with sarcoidosis are unclear, and appropriate treatments are still under debate.
Multiple organ involvement might be one risk factor for bone fracture.
Footnotes
Contributors: MS and TS wrote the manuscript and managed the patient in a hospital setting; HI and HG managed the patient in the outpatient department.
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Neville E, Carstairs LS, James DG. Sarcoidosis of bone. Q J Med 1977; 46:215–27 [PubMed] [Google Scholar]
- 2.Ito M, Motomiya M, Abumi K, et al. Vertebral osteonecrosis associated with sarcoidosis. Case report. J Neurosurg Spine 2005;2:222–5 [DOI] [PubMed] [Google Scholar]
- 3.Handa T, Nagai S, Ito I, et al. Multiple bone fractures found in a young sarcoidosis patient with long stable disease. Intern Med 2005;44:1269–75 [DOI] [PubMed] [Google Scholar]
- 4.O'Daly BJ, Harty JA, O'Malley N, et al. Bilateral olecranon fracture as first presentation of sarcoidosis: case report and review of the literature. J Shoulder Elbow Surg 2008;17:e1–5 [DOI] [PubMed] [Google Scholar]
- 5.Watoson RC, Cahen I. Pathological fracture in long bone sarcoidosis. Report of a case. J Bone Joint Surg Am 1973;55:613–17 [PubMed] [Google Scholar]
- 6.Engle EA, Cooney FD. Tetraplegia secondary to cervical sarcoidosis. Case report. J Neurosurg 1979;50:665–7 [DOI] [PubMed] [Google Scholar]
- 7.Guilford WB, Mentz WM, Kopelman HA, et al. Sarcoidosis presenting as a rib fracture. Am J Roentgenol 1982;139:608–9 [DOI] [PubMed] [Google Scholar]
- 8.Adelaar RS. Sarcoidosis of the upper extremity: case presentation and literature review. J Hand Surg Am 1983;8:492–6 [DOI] [PubMed] [Google Scholar]
- 9.Landi A, Brooks D, De Santis G, et al. Sarcoidosis of the hand—report of two cases. J Hand Surg Am 1983;8:197–200 [DOI] [PubMed] [Google Scholar]
- 10.Terranova WA, Williams GS, Kuhlman TA, et al. Acute phalangeal fractures due to undiagnosed sarcoidosis. J Hand Surg Am 1985;10:902–3 [DOI] [PubMed] [Google Scholar]
- 11.Ito T, Ando Y, Ono E, et al. A case of pathological phalangeal fracture due to sarcoidosis. The Japanese Journal of Sarcoidosis and Other Granulomatous Disorders 2005;25:45–51 [Google Scholar]
- 12.Lunn PG, McGlone R, Varian JP. Sarcoidosis presenting with pathological fracture of a metacarpal. J Hand Surg Br 1986;11:137–8 [DOI] [PubMed] [Google Scholar]
- 13.Schuind F, Quintin J, Schils J, et al. Skeletal involvement in sarcoidosis: a case report. J Hand Surg Br 1987;12:279–83 [DOI] [PubMed] [Google Scholar]
- 14.Yasuwaki Y, Tanaka S, Ryose Y, et al. Three cases of sarcoidosis in upper extremity. The Journal of Japanese Society for Surgery of the Hand 1989;6:554–7 [Google Scholar]
- 15.Posner MA, Melendez E, Steiner G. Solitary osseous sarcoidosis in a finger. J Hand Surg Am 1991;16:827–31 [DOI] [PubMed] [Google Scholar]
- 16.Zickel RE, Bernstein RS, Ryan SF, et al. Pathological ununited fractures of the long bones in a patient who had sarcoidosis. A case report. J Bone Joint Surg Am 1995;77:440–3 [DOI] [PubMed] [Google Scholar]
- 17.Isoyama H, Urakami Y, Hasegawa J, et al. A case of sarcoidosis with pathological fracture of second lumber vertebra. Journal of the Hokkaido Rehabilitation Association 2004;32:61–5 [Google Scholar]
- 18.Yamaguchi T, Kono C, Yamada Y, et al. Clinical investigation of sarcoidosis with bone involvement. The Japanese Journal of Sarcoidosis and Other Granulomatous Disorders 2005;25:11–16 [Google Scholar]
- 19.Ertürk A, Ertürk IO, Gülhan M, et al. Vertebral sarcoidosis: an unusual presentation. Sarcoidosis Vasc Diffuse Lung Dis 2007;24:155–6 [PubMed] [Google Scholar]
- 20.Liu B, Zhang X, Zhang W, et al. Solitary osseous sarcoidosis: a rare reason for pathologic fracture. Rheumatol Int 2012;32:2535–8 [DOI] [PubMed] [Google Scholar]
- 21.Kashiwa T, Watanabe K, Yamashita T, et al. A case of osseous sarcoidosis of the foot. J Jpn Soc Surg Foot 2012;33:169–74 [Google Scholar]
- 22.Wilcox A, Bharadwaj P, Sharma OP. Bone sarcoidosis. Curr Opin Rheumatol 2000;12:321–30 [DOI] [PubMed] [Google Scholar]



