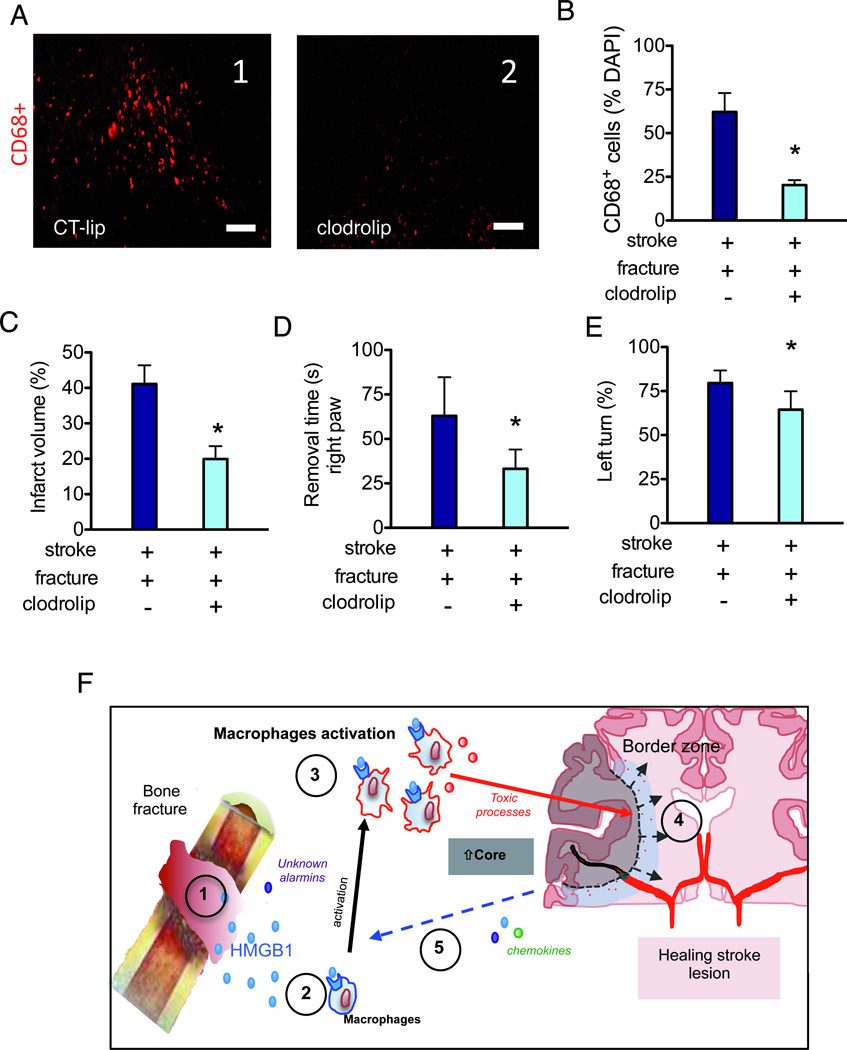
Figure 6. Depletion of macrophage reduces the negative impact of bone fracture on stroke injury.
A. Representative picture taken in the peri-infarct region (bregma 1.3 mm) of mice treated with control liposome (A1, CT-lip) and clodrolip (A2). Scale bar: 100 µm. B. A bar graph shows the quantification of CD68+ cells in the peri-infarct region C. Quantification of infarct volume (n=7, *: P<0.001). D. Quantification of adhesive removal time of the right paw (n=10, *: P<0.001). E. Quantification of the percentage of left turn (n=10, *: P<0.001). F. Synthesis of possible mechanisms underlying the negative impact of bone fracture on stroke injury: 1-Alarmins including HMGB1 is released into blood after bone fracture. 2-HMGB1 interacts with its receptors on innate immune cells including macrophages. 3-Systemic macrophages are recruited to the stroke lesion site in the brain; together with activated microglia, they release neurotoxic molecules 4-Exacerbation of neuro-inflammation, neuronal cell death and behavior dysfunction. 5-Increased neuronal death further increases the release of alarmins and chemokines, triggering a vicious cycle through HMGB1-macrophage activation. CT-lip: control liposome; HMGB1:High-mobility-group box chromosomal protein-1.