Abstract
Metastatic spread from non-head and neck tumours (H&N) to the paranasal and orbital region is extremely rare. We present a case of breast cancer metastasis to the left sphenoid wing, lateral wall left orbit, lateral wall left sphenoid sinus, medial and lateral wall left maxillary sinus and left pterygoid plates. We provide an exhaustive clinicoradiological imaging with a brief literature review.
Background
All paranasal sinuses (PNS) and the orbit are potential sites for metastases and spread to the PNS from breast cancer (BC) has been documented previously.1 About 2.5–13% overall orbital tumours are metastatic, usually in the context of multisystem, end-stage, diagnosed cancer disease. Although metastasis to the orbit is rare, it must be considered in the differential diagnosis of any patient with known history of cancer, presenting with ophthalmic symptoms. The orbital metastasis may be the presenting problem in 25% of patients with cancer of which BC is the most common primary source with a median presentation in the fifth or sixth decade of life.2
Case presentation
A 62-year-old, postmenopausal woman, diagnosed and treated case of left breast infiltrating ductal carcinoma (IDC), post neoadjuvant (NA) chemotherapy (CT), post modified radical mastectomy (MRM), post adjuvant CT, post radiotherapy (RT) both locoregional (LR) and spine presented to us with a diagnosis of expansile bony lesion involving left retro-orbitosphenoidotemporal region with intracranial extension causing proptosis, visual loss and pain (figure 1).
Figure 1.

Clinical picture of the patient.
Investigations
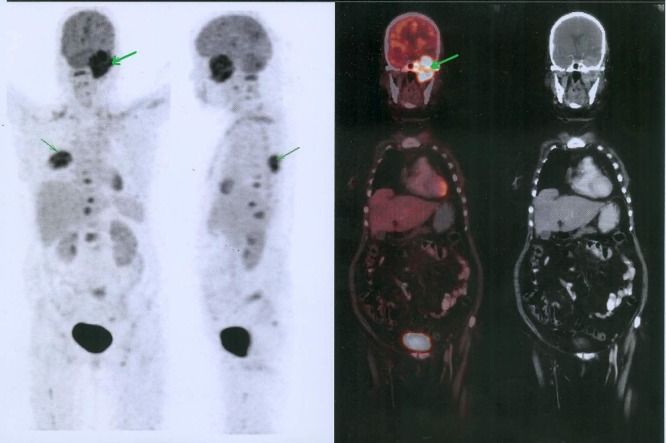
The patient underwent a whole-body (WB) 18 fluorodeoxy glucose (FDG) positron emission tomography (PET) CT that revealed an FDG avid standard uptake value (SUV max 10.6) mass measuring approximately 5.8 (AP)×5.7 (TR)×5.7 (CC) cm, involving the anterior pole of the left temporal lobe, left orbit, left parasellar region, left half of the sphenoid sinus, apex of left maxillary sinus and left ethmoid sinus and extending inferiorly into the left infratemporal fossa and left pterygopalatine fossa. Another avid (SUV max 8.7) enhancing lesion measuring 1.1×1.1 cm is evident in the left temporal lobe, with additional abnormalities seen in the left parietal lobe and left basal ganglia (figures 2–4). There was subcutaneous oedema on the left side of the face. No focal uptake was seen on the left anterior chest wall, right breast and bilateral axillae. Liver was normal.
Figure 2.
Whole-body 18 fluorodeoxy glucose positron emission tomography-CT images.
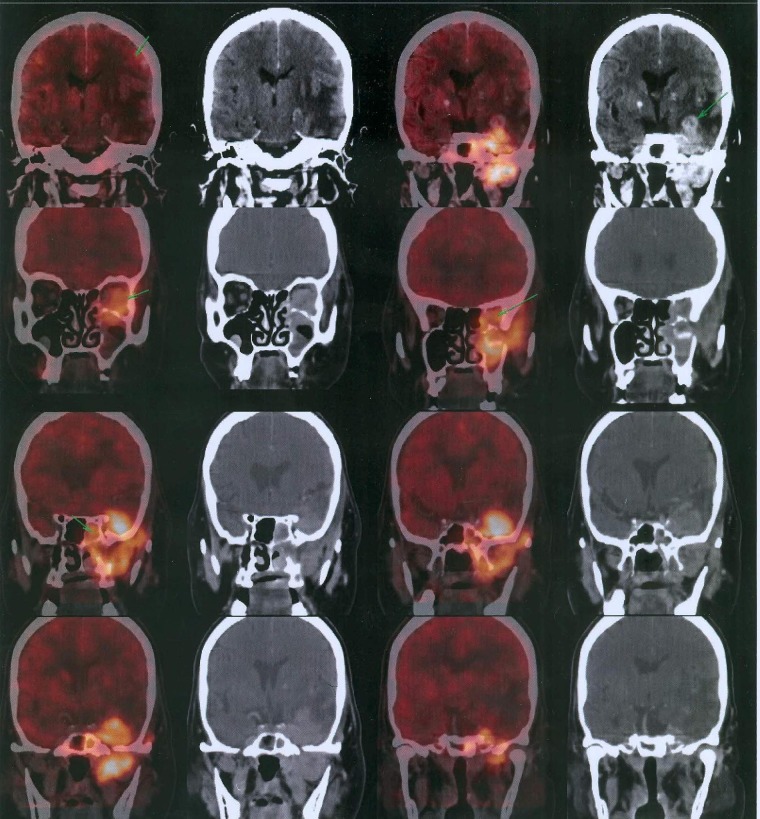
Figure 3.
Coronal positron emission tomography-CT images depicting the lesion.
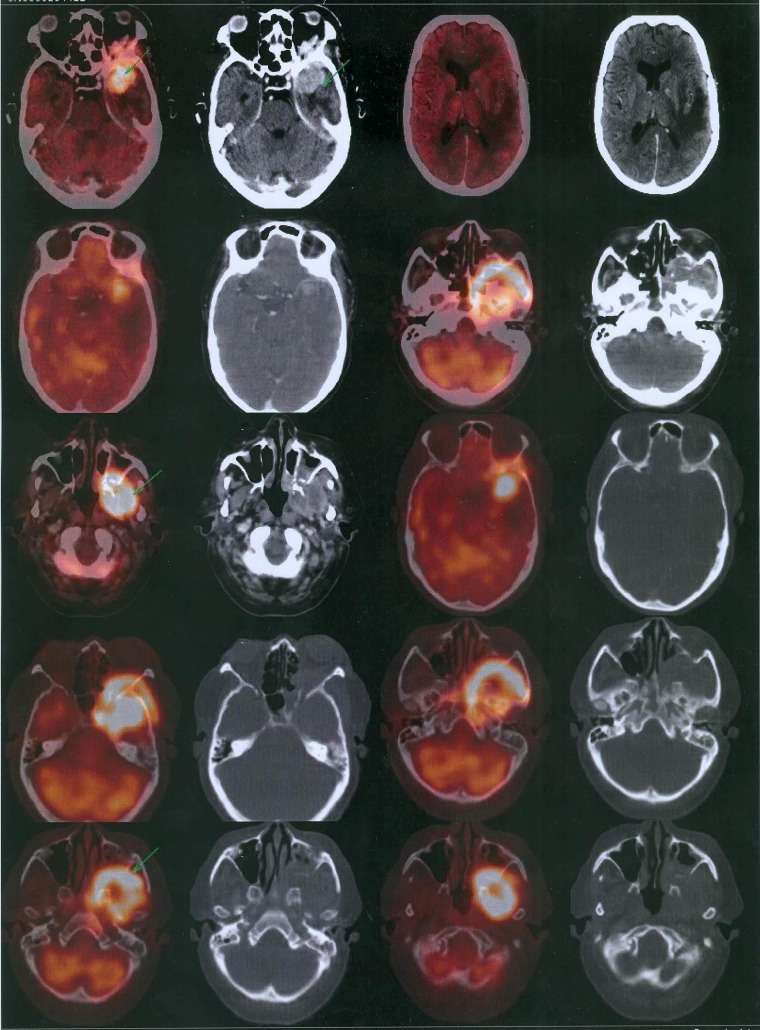
Figure 4.
Axial positron emission tomography-CT images depicting the lesion.
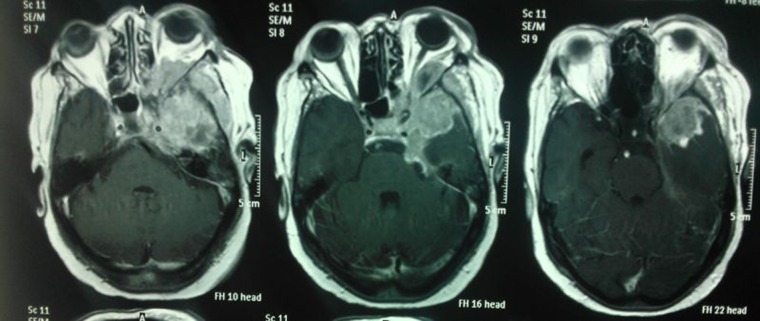
She was further subjected to a contrast-enhanced MRI of the brain to rule out any intracranial involvement that revealed marrow infiltration of the left sphenoid wing, lateral wall left orbit, lateral wall left sphenoid sinus, medial and lateral wall left maxillary sinus and left pterygoid plates with associated enhancing extra-axial soft tissue mass as the likely bony metastases (figures 5 and 6). She was then referred for palliative RT.
Figure 5.
Axial MRI postcontrast images.
Figure 6.
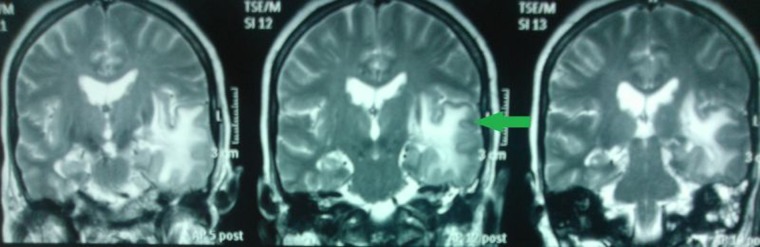
Coronal MRI T2 FLAIR images.
Treatment
She was planned for RT to a total dose of 3000 cGy in 12 sessions to the whole brain along with a dose of 3600 cGy to the clinical target volume that comprised the left orbital region (figure 7). The patient tolerated the treatment well with no radiation-related morbidities.
Figure 7.
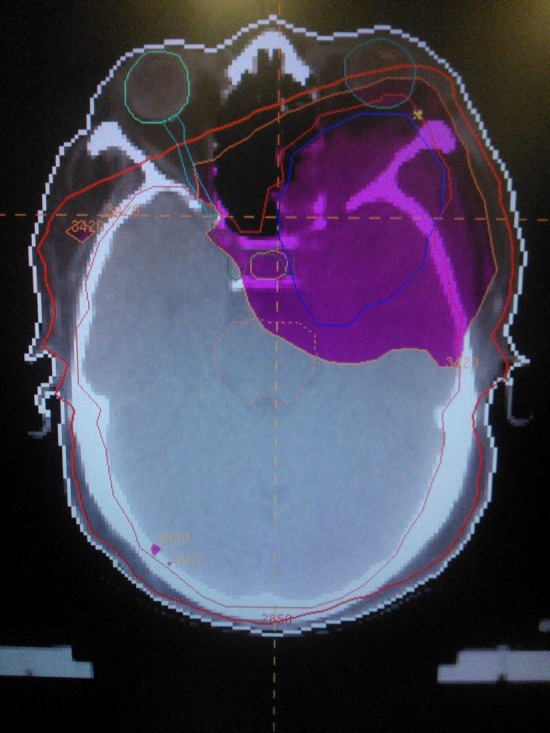
Radiation dose distribution.
Her treatment was completed as per schedule with a good relief in pain and reduction in the need for pain killers. At completion of the therapy she was in a fair general condition with normal vital parameters. She had no headache, vomiting or any neurological deficit.
Discussion
BC metastases have a relatively wide distribution; however, the most common sites of spread are bone, regional lymphatics, lung, liver and the brain.3
The incidence of BC metastases to the H&N region remains largely unknown. It is postulated that many metastases to this region go undetected, as they are ‘obscured’ by more evident metastatic disease at other sites. Haematogenous spread is the most likely route, via the classical venous route of Batson along the prevertebral venous plexus.4 Investigating orbitoparanasal lesions starts with clinical history and examination and includes tissue diagnosis via biopsy and histopathological analysis.
F18-FDG-PET CT can detect the primary with a sensitivity of 79–90%. Its sensitivity is 80–95% for detection of distant metastasis. The negative predictive value of FDG PET CT is 90%. Metastasis can occur at any location. Axillary lymph nodes, internal mammary lymph nodes, bone, liver and brain are the organs involved in order of frequency.5 MRI provides better delineation and higher resolution when there is need to investigate intracranial and soft tissue spread, including nodal involvement. Radiation therapy is an effective means of palliation in such a scenario.
Learning points.
Breast cancer may metastasise to uncommon anatomic sites.
Appropriate use of newer radiographic technologies has revealed a greater incidence of spread to the sino-orbital region than was previously recognised.
New and advanced imaging technologies have the advantage of precise diagnosis and demarcation of these lesions and may assist in an efficient and targeted radiation delivery to the same.
Acknowledgments
The authors thank Dr Sachin Arora, Classified Specialist, Department of Nuclear Medicine, Artemis Hospital, Gurgaon, Haryana, India.
Footnotes
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Walker DT, Barbur S, Mathew R, et al. Sinus involvement in breast cancer: case report. J Laryngol Otol 2013;127:619–20 [DOI] [PubMed] [Google Scholar]
- 2.Asproudis I, Gorezis S, Charalabopoulos K, et al. Breast carcinoma metastasis to the orbit and paranasal sinuses: a case report. Exp Oncol 2004;26:246–8 [PubMed] [Google Scholar]
- 3.Klein A, Olendrowitz C, Schmutzler R. et al. Identification of brain- and bone-specific breast cancer metastasis genes. Cancer Lett 2009;276:212–20 [DOI] [PubMed] [Google Scholar]
- 4.Debois JM. TxNxM1: the anatomy and clinics of metastatic cancer. Boston: Kluwer Academic Publishers, 2002 [Google Scholar]
- 5.Morton KA, Clark PB. Diagnostic imaging—nuclear medicine. 1st edn Utah, USA: Amirsys Inc. Salt Lake, 2007:11–35 [Google Scholar]