Abstract
Purpose
Laparoscopic resection for transverse colon cancer is a technically challenging procedure that has been excluded from various large randomized controlled trials of which the long-term outcomes still need to be verified. The purpose of this study was to evaluate long-term oncologic outcomes for transverse colon cancer patients undergoing laparoscopic colectomy (LAC) or open colectomy (OC).
Methods
This retrospective review included patients with transverse colon cancer who received a colectomy between January 2006 and December 2010. Short-term and five-year oncologic outcomes were compared between these groups.
Results
A total of 131 patients were analyzed in the final study (LAC, 84 patients; OC, 47 patients). There were no significant differences in age, gender, body mass index, tumor location, operative procedure, or blood loss between groups, but the mean operative time in LAC was significantly longer (LAC, 246.8 minutes vs. OC, 213.8 minutes; P = 0.03). Hospital stay was much shorter for LAC than OC (9.1 days vs. 14.5 days, P < 0.01). Postoperative complication rates were not statistically different between the two groups. In terms of long-term oncologic data, the 5-year disease-free survival and overall survival were not statistically different between both groups, and subgroup analysis according to cancer stage also revealed no differences.
Conclusion
LAC for transverse colon cancer is feasible and safe with comparable short- and long-term outcomes.
Keywords: Laparoscopic surgery, Colonic neoplasm, Colon, Transverse
INTRODUCTION
Laparoscopic colon surgery (LAC) was first introduced for the treatment of colorectal cancer in 1991 [1]. Since its introduction, there have been many technical improvements to this procedure. Several randomized controlled trials have demonstrated its safety, oncologic efficacy and short-term benefits including shorter hospital stays, less postoperative pain and earlier return to normal activity compared to an open colectomy (OC) [2-11].
Given the technical difficulty involved in performing complete mesocolic excision and ligation of the middle colic vessels by laparoscopy, many of these trials have not included patients with transverse colon cancer [12,13]. Recently, several experienced surgeons have started to report on the oncologic outcomes for laparoscopic colectomy in patients with transverse colon cancer [11,14-16], but long-term outcomes still need to be verified.
As a tertiary referral care center, our institution has many experiences with laparoscopic surgery for transverse colon cancer. This study investigated the oncologic outcomes for laparoscopic surgery compared to open surgery in patients with transverse colon cancer in our institution.
METHODS
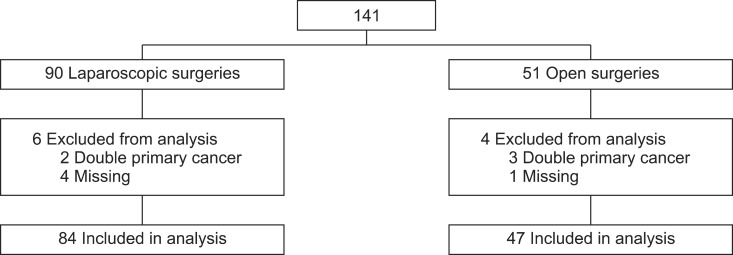
This retrospective study included 141 consecutive patients who underwent a curative colectomy for transverse colon cancer (pathologic TNM stage I-III) at the Yonsei University Health System between January 2006 and December 2010. Then 10 patients were excluded due to a previous malignancy, double primary cancer and missing follow-up (Fig. 1).
Fig. 1.
Overall study design and overview of patient population.
Diagnosis of colon cancer was confirmed by a colonoscopic biopsy. For evaluation of distant metastasis, an abdominopelvic and a chest computed tomography (CT) were performed. If necessary, a positron emission tomography (PET)-CT and liver magnetic resonance imaging (MRI) were also performed. Any tumor distal to the hepatic flexure and proximal to the splenic flexure was defined as transverse colon cancer.
Tumor staging was based on the 7th American Joint Committee on Cancer guidelines.
The decision to perform a laparoscopic colectomy versus an OC was at the surgeon's discretion. In cases of early transverse colon cancer detection, unless the tumor was greater than T3 or proved to be bulky on the CT scan, colonoscopic tattooing was performed preoperatively for easier intraoperative localization. For primary lesions distal to the hepatic flexure, an extended right hemicolectomy was performed by ligation of the ileocolic, the midcolic and the right colic vessels (if present). Lesions proximal to the splenic flexure underwent an extended left hemicolectomy with ligation of the midcolic, left colic and the first branch of the sigmoid vessels. Transverse colectomy was performed by ligation of the midcolic vessels when the remaining transverse colon was free enough of tension to be anastomosed. Subtotal colectomy was also performed if it was necessary. We utilized a medial to lateral no-touch isolation technique, which enabled dissection of lymph nodes along the surgical trunk, followed by transection of the colon and mesentery without tumor manipulation. This degree of resection was similar to the technique used in Hohenberger et al. [17]. Methods for anastomosis were determined based on surgical preference and performed extracorporially in laparoscopic colectomy cases in a manner similar to the open procedure.
Clinical characteristics, short-term surgical outcomes and midterm oncologic outcomes were compared between the laparoscopic and open surgery groups. Postoperative complications were classified as grades I-V according to the Dindo classification scale, which were further subdivided into minor (stages I-II) and major (stages III-V) complications [18]. We routinely examined patients in the outpatient clinic at 1 and 3 months postdischarge, then every 3 months for the first three years and finally every 6 months for the subsequent 2 years. Carcinoembryonic antigen was performed prior to surgery, at postoperative day 7 and whenever the patient had postoperative follow-up in the outpatient clinic. For diagnosis of local and systemic recurrence, an abdominopelvic CT and a chest CT were performed at every 6 months during the follow-up period. A PET-CT and liver MRI were also performed if it was necessary.
Data were analyzed using the IBM SPSS ver. 18.0 (IBM Co., Armonk, NY, USA). An independent t-test for continuous values and Fisher exact test for parametric values were performed. Categorical variables were compared using the chi-square test (Tables 1-3). We constructed survival curves using the Kaplan-Meier method (Figs. 2, 3) and comparisons were made using the log-rank test. A P-value less than 0.05 was considered statistically significant.
Table 1.
Clinical characteristics and surgical data in the laparoscopic and conventional open surgery groups
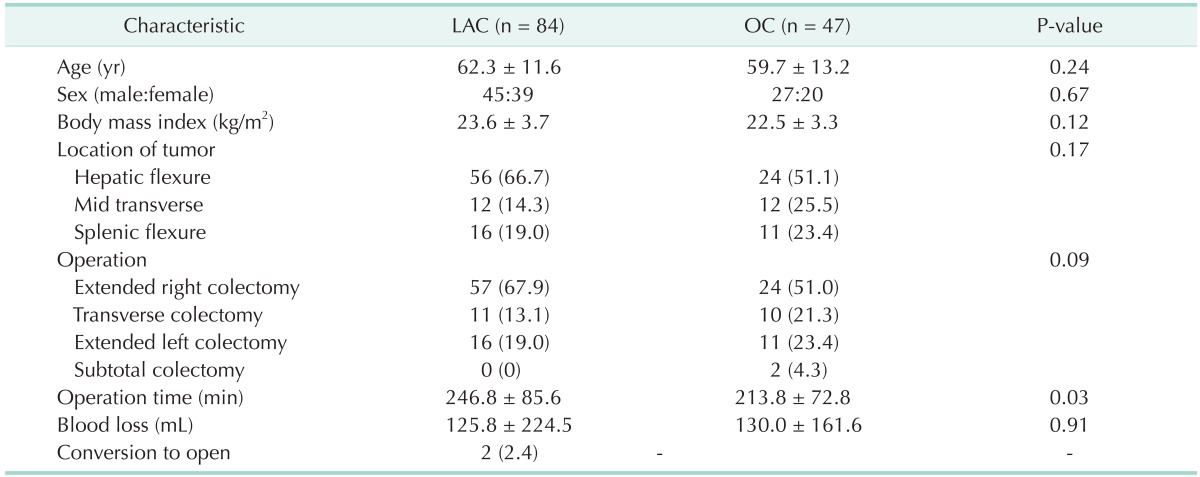
Values are presented as mean ± standard deviation or number (%). An independent t-test for continuous values and chi-square test for categorical values.
LAC, laparoscopic colectomy; OC, open colectomy.
Table 3.
Postoperative short-term outcomes in the laparoscopic and conventional open surgery groups
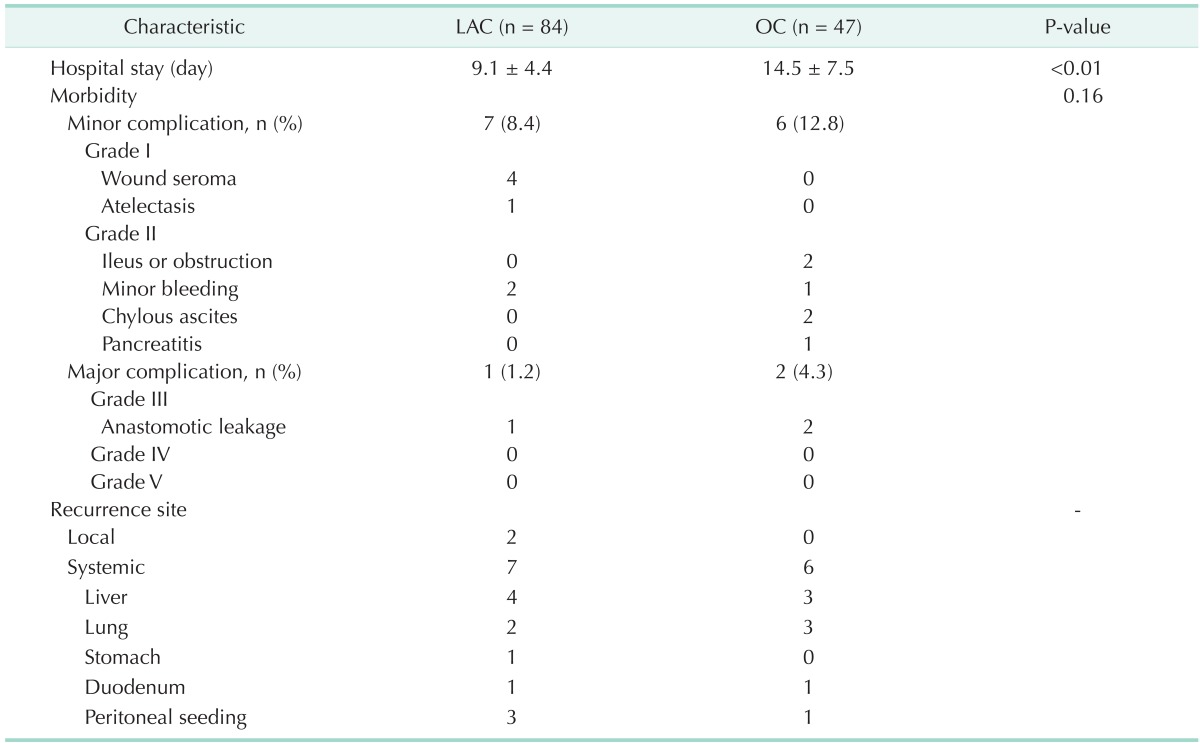
Values are presented as mean ± standard deviation or number (%). An independent t-test for continuous values and chi-square test for categorical values.
LAC, laparoscopic colectomy; OC, open colectomy.
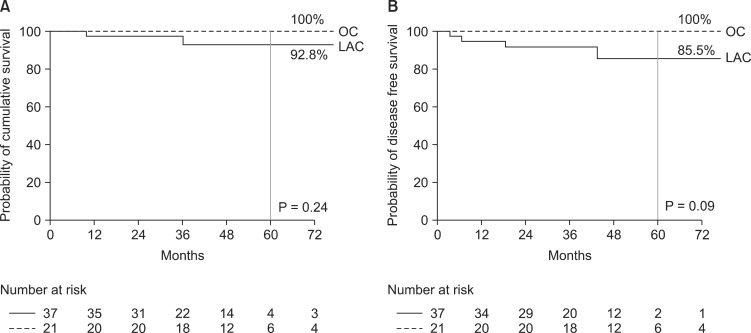
Fig. 2.
Kaplan-Meier estimates of overall survival (A) and disease free survival (B) in the laparoscopic and conventional open group for stage II transverse colon cancer. OC, open colectomy; LAC, laparoscopic colectomy.
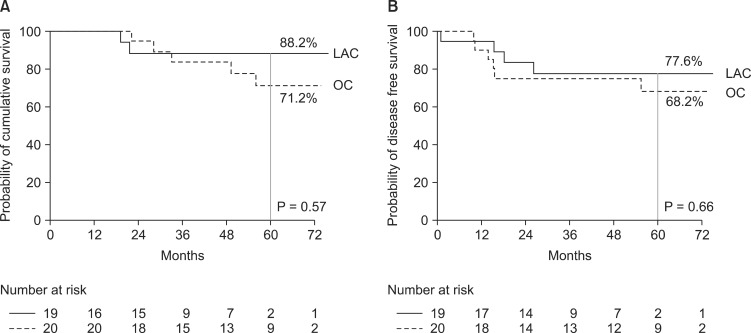
Fig. 3.
Kaplan-Meier estimates of overall survival (A) and disease free survival (B) in the laparoscopic and conventional open group for stage III transverse colon cancer. LAC, laparoscopic colectomy; OC, open colectomy.
RESULTS
A total of 131 patients were analyzed in the final study (LAC, 84 patients; OC, 47 patients). Patient demographics and operative data are presented in Table 1. There was no difference in sex, age, body mass index, tumor location, operative procedure or blood loss between the groups, but the mean operative time in LAC was significantly longer (LAC, 246.8 minutes vs. OC, 213.8 minutes; P = 0.03). Two cases (2.4%) were converted to open surgery due to the presence of severe adhesions.
There were no significant differences in tumor size, histology type between the two groups (Table 2). No intergroup differences in proximal margin, distal margin and number of harvested lymph nodes were also observed. According to the TNM classification system, early stage transverse colon cancer (Tis, stage I) was observed more frequently in the LAC group compared to the OC group (33.3% vs. 12.7%), whereas stage III disease was more prevalent in the OC group than the LAC group (42.6% vs. 22.6%) (P = 0.01).
Table 2.
Tumor characteristics in the laparoscopic and conventional open surgery groups
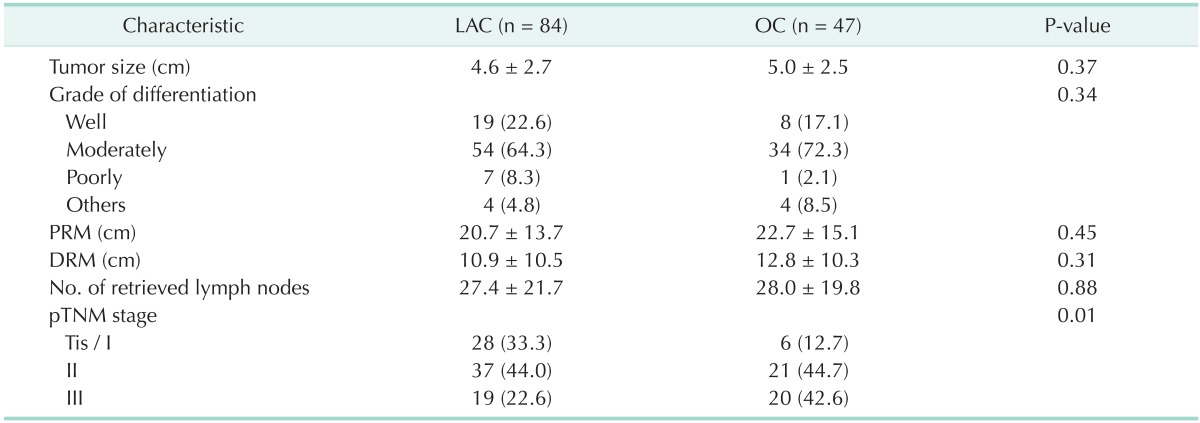
Values are presented as mean ± standard deviation or number (%). An independent t-test for continuous values and chi-square test for categorical values.
LAC, laparoscopic colectomy; OC, open colectomy; PRM, proximal resection margin; DRM, distal resection margin.
Hospital stay was considerably shorter for LAC than for OC (9.1 days vs. 14.5 days, P < 0.01) (Table 3). Rates of postoperative complications were not statistically different between the two groups (OC, 17.1% vs. LAC, 9.6%, P = 0.16). Most complications were minor including wound seroma, postoperative ileus or obstruction, minor bleeding and chylous ascites. Regarding major complications, two cases of grade 3 complications included major anastomotic leakages in the OC group, which required mandatory reoperations. One case of a grade 3 complication included a minor anastomotic leakage in the LAC group requiring only supportive care. There were no cases of immediate postoperative mortality in the two groups.
Median follow-up was 58 months (range, 10-85 months) for OC and 42 months (range, 7-82 months) for LAC. Nine patients (10.7%) had cancer recurrence in the LAC group during the follow-up period. Four patients died from systemic recurrence and cancer progression. In the OC group, 6 patients (12.8%) had cancer recurrences. Five of them had systemic recurrence and died from cancer progression. Five-year disease free survival (DFS) was 87.4% for LAC and 85.7% for OC, with no statistically significant difference between the two groups (P = 0.89). There were no intergroup differences in the 5-year overall survival (OS) (LAC, 94.3% vs. OC, 86.7%, P = 0.40).
We performed a subgroup analysis to evaluate any group differences attributable to the discrepancy of the cancer stage. According to our data, it was statistically impossible to compare DFS and OS in stage I patients between the two groups because there were no recurrence or disease-related death except only one recurrence in the LAC group. According to a subgroup analysis of stage II and III transverse colon cancer patients, there were no significant differences in OS and DFS between the two groups (Figs. 2, 3). The results demonstrated that there were no statistically significant differences in 5-year DFS for stage II patients (LAC, 85.5% vs. OC, 100%, P = 0.09). In terms of 5-year OS, there were no statistical differences between the two groups (LAC, 92.8% vs. OC, 100%, P = 0.24). Similarly, there were no differences in 5-year DFS for stage III patients between both groups (LAC, 77.6% vs. OC, 68.2%, P = 0.66). 5-year OS in stage III patients were similar between two groups (LAC, 88.2% vs. OC, 71.2%, P = 0.57).
DISCUSSION
Laparoscopic approaches have been proposed in several surgical fields, and these modalities provide widely-recognized clinical benefits, including less pain and intraoperative blood loss, shorter recovery and hospitalization times, and better cosmetics. Laparoscopic colectomy has been shown not only to be technically safe and feasible, but also offers similar long-term outcomes for colorectal cancer compared to open surgical procedures based on large, randomized controlled trials [4-8]. However, all these studies have excluded transverse colon cancer due to the technical difficulty in performing an adequate oncologic resection laparoscopically, and very few studies are available for laparoscopic colectomy of the transverse colon cancer.
In our results, LAC for transverse colon cancer was found to be quite safe and feasible. The rates of postoperative complications were not statistically different between the LAC and OC groups (OC, 17.1% vs. LAC, 9.6%, P = 0.16). These similar rates are comparable with other reports. Akiyoshi et al. [19] and Kim et al. [20] also reported in their studies that short-term postoperative complications were acceptable in laparoscopic colectomy for transverse colon cancer.
Generally, oncologic feasibility can be assessed from three points of view. First of all, adequate oncologic resection should be evaluated. Secondly, the recurrence rate should be acceptable. Lastly, OS should not be influenced by the surgical methods. Recently, some studies have started to report oncologic outcomes for LAC in transverse colon cancer. Hahn et al. [15] reported acceptable oncologic outcomes compared to other previous randomized trials. The 5-year OS rate and disease-free survival rate was 84.7% and 89.3%, respectively in their study. However, the laparoscopic results were compared to results of other previous clinical trials instead of the results for open surgery results from the same period. On the other hand, our study showed acceptable oncologic outcomes of LAC for transverse colon cancer compared to OC during the follow-up observation.
In our study, 5-year DFS was 87.4% in LAC and 85.7% in OC (P = 0.89), whereas 5-year OS was 94.3% in LAC and 86.7% in OC (P = 0.40). These are also comparable oncologic results to others. We suspect that these favorable oncologic results can be attributed to the surgical technique and planning. All laparoscopic colectomies in this study had complete mesocolic excision (CME) and central vascular ligation (CVL), first named by Hohenberger et al. [17] in 2008. There have been some debates of feasibility for CME-CVL in LAC. Gouvas et al. [21] insisted that laparoscopic CME-CVL surgery for transverse colon cancer was incomplete in comparison to open surgical resection in their study. However, Fujita et al. [22] described a medial approach to overcome this obstacle. They utilized a no-touch technique, which dissected lymph nodes along the surgical trunk, followed by transection of the transverse colon, terminal ileum, and mesentery without tumor manipulation. We also utilized this medial to lateral no-touch isolation technique. We also reported no significant differences in proximal resection margin (LAC, 20.7 cm vs. OC, 22.7 cm, P = 0.45), distal resection margin (LAC, 10.9 cm vs. OC, 12.8 cm, P = 0.31), and harvested lymph nodes (LAC, 27.4 vs. OC, 28.0, P = 0.88) between the LAC and OC groups. Therefore, we can confirm that laparoscopic transverse colectomy could be oncologically feasible for transverse colon cancer compared to open surgery.
This study does have some limitations. First, there was the selection bias often inherent in retrospective studies. The decision to undergo a laparoscopic colectomy was at the surgeon's discretion. Early stage transverse colon cancer (stages 0, I) more frequently proceeded to laparoscopic resection (LAC, 33.3% vs. OC, 12.7%). Meanwhile, advanced transverse colon cancer (stage III) was more frequently associated with open surgery (OC, 42.6% vs. LAC, 22.6%). For this reason, we performed a subgroup analysis for each stage, and similar results for the long-term follow-up between the two groups were also shown in the subgroup analysis. The second imitation is the small number of cases.
Based on the results of this study, laparoscopic colectomy for transverse colon cancer was feasible and safe with good short-term outcomes. Moreover, there were no significant differences in long-term oncologic outcomes between laparoscopy and open surgery. However, our conclusion cannot be generalized because of our study limitation. Nevertheless, we expect that our study may help lead to conduct future prospective randomized trials for investigation of long-term oncologic outcomes for laparoscopic colectomy in transverse colon cancer to confirm our study results.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Fowler DL, White SA. Laparoscopy-assisted sigmoid resection. Surg Laparosc Endosc. 1991;1:183–188. [PubMed] [Google Scholar]
- 2.Colon Cancer Laparoscopic or Open Resection Study Group. Buunen M, Veldkamp R, Hop WC, Kuhry E, Jeekel J, et al. Survival after laparoscopic surgery versus open surgery for colon cancer: long-term outcome of a randomised clinical trial. Lancet Oncol. 2009;10:44–52. doi: 10.1016/S1470-2045(08)70310-3. [DOI] [PubMed] [Google Scholar]
- 3.Fleshman J, Sargent DJ, Green E, Anvari M, Stryker SJ, Beart RW, Jr, et al. Laparoscopic colectomy for cancer is not inferior to open surgery based on 5-year data from the COST Study Group trial. Ann Surg. 2007;246:655–662. doi: 10.1097/SLA.0b013e318155a762. [DOI] [PubMed] [Google Scholar]
- 4.Green BL, Marshall HC, Collinson F, Quirke P, Guillou P, Jayne DG, et al. Long-term follow-up of the Medical Research Council CLASICC trial of conventional versus laparoscopically assisted resection in colorectal cancer. Br J Surg. 2013;100:75–82. doi: 10.1002/bjs.8945. [DOI] [PubMed] [Google Scholar]
- 5.Guillou PJ, Quirke P, Thorpe H, Walker J, Jayne DG, Smith AM, et al. Short-term endpoints of conventional versus laparoscopic-assisted surgery in patients with colorectal cancer (MRC CLASICC trial): multicentre, randomised controlled trial. Lancet. 2005;365:1718–1726. doi: 10.1016/S0140-6736(05)66545-2. [DOI] [PubMed] [Google Scholar]
- 6.Jayne DG, Thorpe HC, Copeland J, Quirke P, Brown JM, Guillou PJ. Five-year follow-up of the Medical Research Council CLASICC trial of laparoscopically assisted versus open surgery for colorectal cancer. Br J Surg. 2010;97:1638–1645. doi: 10.1002/bjs.7160. [DOI] [PubMed] [Google Scholar]
- 7.Lacy AM, Garcia-Valdecasas JC, Delgado S, Castells A, Taura P, Pique JM, et al. Laparoscopy-assisted colectomy versus open colectomy for treatment of non-metastatic colon cancer: a randomised trial. Lancet. 2002;359:2224–2229. doi: 10.1016/S0140-6736(02)09290-5. [DOI] [PubMed] [Google Scholar]
- 8.Leung KL, Kwok SP, Lam SC, Lee JF, Yiu RY, Ng SS, et al. Laparoscopic resection of rectosigmoid carcinoma: prospective randomised trial. Lancet. 2004;363:1187–1192. doi: 10.1016/S0140-6736(04)15947-3. [DOI] [PubMed] [Google Scholar]
- 9.Lujan HJ, Plasencia G, Jacobs M, Viamonte M, 3rd, Hartmann RF. Long-term survival after laparoscopic colon resection for cancer: complete five-year follow-up. Dis Colon Rectum. 2002;45:491–501. doi: 10.1007/s10350-004-6227-8. [DOI] [PubMed] [Google Scholar]
- 10.Veldkamp R, Kuhry E, Hop WC, Jeekel J, Kazemier G, Bonjer HJ, et al. Laparoscopic surgery versus open surgery for colon cancer: short-term outcomes of a randomised trial. Lancet Oncol. 2005;6:477–484. doi: 10.1016/S1470-2045(05)70221-7. [DOI] [PubMed] [Google Scholar]
- 11.Yamamoto M, Okuda J, Tanaka K, Kondo K, Tanigawa N, Uchiyama K. Clinical outcomes of laparoscopic surgery for advanced transverse and descending colon cancer: a single-center experience. Surg Endosc. 2012;26:1566–1572. doi: 10.1007/s00464-011-2071-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kuwabara K, Matsuda S, Fushimi K, Ishikawa KB, Horiguchi H, Fujimori K. Quantitative comparison of the difficulty of performing laparoscopic colectomy at different tumor locations. World J Surg. 2010;34:133–139. doi: 10.1007/s00268-009-0292-z. [DOI] [PubMed] [Google Scholar]
- 13.Zmora O, Bar-Dayan A, Khaikin M, Lebeydev A, Shabtai M, Ayalon A, et al. Laparoscopic colectomy for transverse colon carcinoma. Tech Coloproctol. 2010;14:25–30. doi: 10.1007/s10151-009-0551-x. [DOI] [PubMed] [Google Scholar]
- 14.Fernandez-Cebrian JM, Gil Yonte P, Jimenez-Toscano M, Vega L, Ochando F. Laparoscopic colectomy for transverse colon carcinoma: a surgical challenge but oncologically feasible. Colorectal Dis. 2013;15:e79–e83. doi: 10.1111/codi.12067. [DOI] [PubMed] [Google Scholar]
- 15.Hahn KY, Baek SJ, Joh YG, Kim SH. Laparoscopic resection of transverse colon cancer: long-term oncologic outcomes in 58 patients. J Laparoendosc Adv Surg Tech A. 2012;22:561–566. doi: 10.1089/lap.2011.0422. [DOI] [PubMed] [Google Scholar]
- 16.Schlachta CM, Mamazza J, Poulin EC. Are transverse colon cancers suitable for laparoscopic resection? Surg Endosc. 2007;21:396–399. doi: 10.1007/s00464-006-9042-6. [DOI] [PubMed] [Google Scholar]
- 17.Hohenberger W, Weber K, Matzel K, Papadopoulos T, Merkel S. Standardized surgery for colonic cancer: complete mesocolic excision and central ligation: technical notes and outcome. Colorectal Dis. 2009;11:354–364. doi: 10.1111/j.1463-1318.2008.01735.x. [DOI] [PubMed] [Google Scholar]
- 18.Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–213. doi: 10.1097/01.sla.0000133083.54934.ae. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Akiyoshi T, Kuroyanagi H, Fujimoto Y, Konishi T, Ueno M, Oya M, et al. Short-term outcomes of laparoscopic colectomy for transverse colon cancer. J Gastrointest Surg. 2010;14:818–823. doi: 10.1007/s11605-010-1182-2. [DOI] [PubMed] [Google Scholar]
- 20.Kim HJ, Lee IK, Lee YS, Kang WK, Park JK, Oh ST, et al. A comparative study on the short-term clinicopathologic outcomes of laparoscopic surgery versus conventional open surgery for transverse colon cancer. Surg Endosc. 2009;23:1812–1817. doi: 10.1007/s00464-009-0348-z. [DOI] [PubMed] [Google Scholar]
- 21.Gouvas N, Pechlivanides G, Zervakis N, Kafousi M, Xynos E. Complete mesocolic excision in colon cancer surgery: a comparison between open and laparoscopic approach. Colorectal Dis. 2012;14:1357–1364. doi: 10.1111/j.1463-1318.2012.03019.x. [DOI] [PubMed] [Google Scholar]
- 22.Fujita J, Uyama I, Sugioka A, Komori Y, Matsui H, Hasumi A. Laparoscopic right hemicolectomy with radical lymph node dissection using the no-touch isolation technique for advanced colon cancer. Surg Today. 2001;31:93–96. doi: 10.1007/s005950170230. [DOI] [PubMed] [Google Scholar]