Abstract
Objective
We aimed to explore stakeholder views, attitudes, needs, and expectations regarding likely benefits and risks resulting from increased structuring and coding of clinical information within electronic health records (EHRs).
Materials and methods
Qualitative investigation in primary and secondary care and research settings throughout the UK. Data were derived from interviews, expert discussion groups, observations, and relevant documents. Participants (n=70) included patients, healthcare professionals, health service commissioners, policy makers, managers, administrators, systems developers, researchers, and academics.
Results
Four main themes arose from our data: variations in documentation practice; patient care benefits; secondary uses of information; and informing and involving patients. We observed a lack of guidelines, co-ordination, and dissemination of best practice relating to the design and use of information structures. While we identified immediate benefits for direct care and secondary analysis, many healthcare professionals did not see the relevance of structured and/or coded data to clinical practice. The potential for structured information to increase patient understanding of their diagnosis and treatment contrasted with concerns regarding the appropriateness of coded information for patients.
Conclusions
The design and development of EHRs requires the capture of narrative information to reflect patient/clinician communication and computable data for administration and research purposes. Increased structuring and/or coding of EHRs therefore offers both benefits and risks. Documentation standards within clinical guidelines are likely to encourage comprehensive, accurate processing of data. As data structures may impact upon clinician/patient interactions, new models of documentation may be necessary if EHRs are to be read and authored by patients.
Keywords: Electronic Health Records, Electronic Patient Records, Data Structure, Clinical Coding, Patient Communication
Background and significance
There is considerable strategic interest internationally in the potential that electronic health records (EHRs) and the systems and services that utilize EHR information have for improving the quality and safety of clinical care, increasing the availability and quality of clinical information, informing more effective planning of healthcare delivery and public health, and supporting clinical and biomedical research.1–5 Anticipated health and efficiency gains are, however, largely dependent on increasing the proportion of the clinical record that is structured and/or coded, thereby rendering it computable (ie, machine readable). The impact on clinical practice of imposing increased structure (eg, template entries) or requiring greater clinical coding of records has the potential to have a major impact on the everyday lives of frontline clinicians, but this subject has hitherto received very little research attention.6 Our research was commissioned by the National Health Service (NHS) Connecting for Health Evaluation Programme in anticipation of a major information technology (IT)-based transformation of England's NHS.
Structured and/or coded information (box 1) can enable computers to support clinical decision-making.7 Computer applications can readily manipulate such information, for example, in the presentation of trends in tables and charts or highlighting exceptional findings such as abnormal results, or include clinical data within algorithms to provide decision support. Classification systems use codes to organize information within a domain and should allow for the comprehensive labeling of all relevant concepts.8 However, not all decisions in clinical practice are made on the basis of explicit, computable knowledge. Individual and contextual dimensions such as multi-morbidity, tacit knowledge, and intuitive understanding are frequently used in deciding on a clinical management strategy.9 The process of classification may imply false certainty when the concept to be coded may, for example, be an evolving disease or an uncertain clinical condition.10 Clinicians may be reluctant to code during their clinical work,11 and retrospective coding of health records by administrative staff may be prone to inaccuracies.12
Box 1. Key definitions.
Coded data: information represented using terms taken from a terminology or controlled vocabulary
Structured data: information organized according to a logical model
Narrative information: sentences and/or informally grouped lines of text
Recently, debate regarding EHRs has broadened to consider the role of documentation in informing a patient's understanding of their own health, choice of healthcare providers, shared decision-making about care, and self-management, particularly of long-term conditions.3 4 13 14 The provision of medical information by patients is not a new idea, but existing studies have not included patient access to their own health records.15–23 Patient access to their health records is a significant change in the use of clinical documentation that is only just beginning to be investigated and research is currently limited by a lack of universal coverage of EHRs.24 This raises new questions about the use of structured and coded information for lay readership. Today's health record is a biomedically orientated, de-personalized document that provides a distillation of information determined by the authors’ professional points of view. It is intended to primarily serve the needs of professionals.25 26 The need to provide for patients as readers and authors of health records therefore presents a potential challenge to current models of documentation. Investigations into the optimal structuring of health information to facilitate computation need to address more than biomedical analysis and professional decision support.
To understand the potential benefits and risks of the increased use of structuring and/or coding of information, we sought to explore events, processes, and practices that may impact upon the implementation and adoption of EHRs from a range of perspectives among individuals affected by their use.
Materials and methods
We carried out an exploratory qualitative study to better understand different perspectives regarding the increased use of structured and/or coded information within EHRs, particularly in relation to the clinical history. We sampled a broad array of individuals affected by or involved in processes relevant to the coding/structuring of clinical information.27–31 Our work was informed by a sociotechnical perspective (see online supplementary web appendix 1).32–37 This theoretical lens allowed us to examine how EHRs were situated within social, organizational, and wider political environments. Further, it facilitated in-depth investigation into the interplays between social and technical factors shaping each other over time.
Sampling and recruitment
We sought to sample a broad spectrum of stakeholders including patients, healthcare professionals, health service commissioners, policy makers, managers and administrators, systems developers, researchers, and academics based in England in a variety of care settings including community and hospital settings.38 Interviewee recruitment was facilitated by liaison with our own professional networks and by the UK Clinical Research Network and the Primary Care Research Network. In addition to interviews, we hosted expert discussion groups as part of a national conference. This event was free to attend and details were circulated widely among professional networks and existing contacts to encourage maximum participation from a variety of disciplines. Group discussions took place concurrently and each sought to focus in detail on a specific question relating to the structuring and coding of clinical information. Participants selected and attended the focus group of most interest to them. Each discussion group included a range of healthcare professionals, health service commissioners, policy makers, terminology specialists, information professionals, researchers, and academics.
Data generation
Data collection was conducted by a clinical researcher with expertise in health informatics (BF) and a social scientist (ZM) between October 2010 and September 2011. Semi-structured interviews following topic guides tailored to capture varying perspectives were conducted on a predominantly face-to-face basis or by telephone.39 Where possible, written informed consent was sought from all participants, although in some cases, such as telephone interviews, verbal consent was recorded. Each discussion group and interview was recorded subject to participant consent. All data were anonymized to protect the confidentiality of participant organizations and individual interviewees.
The focus of the interviews was on gaining insights regarding perceived benefits and risks surrounding the structuring and/or coding of records. Questions were open-ended and participants were actively encouraged to raise issues important to them relating to the broad topics of structuring, coding, information capture, retrieving information, and decision-making. We adopted a reflexive approach to ensure validity, for example, by adapting our topic guides in response to early findings indicating that participants had not considered structure or coding as discreet topics for discussion. A sample interview topic guide is available in online supplementary web appendix 2. We utilized anonymized replica excerpts of information drawn from the research teams’ clinical practice that might typically be found within health records to stimulate discussion during patient interviews (see online supplementary web appendix 3). Expert discussion involved participants working in groups to focus on particular dimensions of our research. Information on group topics and numbers of participants is available in online supplementary web appendix 4. We collected documentary evidence, observed the working practices of administrative staff and clinical coders, photographed technology, captured computer screen images (‘screenshots’) raised for discussion and/or demonstration by participants, and took reflexive field notes during the course of our data collection.
Data handling and analysis
Recorded data were transcribed verbatim and analyzed together with accompanying field notes, photographs, screenshots, presentations, and documentary evidence. The research team met weekly to review progress, reflect upon their own role in data generation, and discuss areas for possible further enquiry. A broadly deductive approach to analysis was adopted, to reflect the main benefits and risks associated with the introduction of EHRs. Within these broad themes, we used iterative, inductive approaches to analysis using the constant-comparison technique40 to reflect upon key themes emerging from the findings. This thematic analysis ran concurrent to data generation and was initially conducted by two members of the research team (BF and ZM) who worked independently to increase validity.41 Early analysis was discussed by the whole team within a focused workshop to identify areas of interest, consider disconfirming evidence, and reflect on the role of the research team within data generation and themes for further investigation.42 Data generation ended when we felt we had reached theoretical saturation—the point at which no new themes were emerging from the data.43 During the remainder of the study, we met as a research team within a further two data analysis workshops to validate our findings and gain deeper insights into the emergent themes.
Results
We undertook 24 in-depth interviews with 27 participants and hosted six expert discussion groups with 43 participants, thus involving a total of 70 participants. In addition, we undertook observations of healthcare professionals while taking contemporaneous field notes, and we analyzed 20 related documents provided to us by participants. Table 1 details interview participant characteristics.
Table 1.
Interviewee characteristics
| Identifier | Role | Gender | Setting | Interview method |
|---|---|---|---|---|
| 1 | Researcher | Male | Primary care | Face-to-face interview |
| 2 | Researcher | Male | Primary care | Face-to-face interview |
| 3 | Systems developer | Male | Secondary care | Face-to-face interview |
| 4 | Clinical lead | Male | Secondary care | Face-to-face interview |
| 5 | Systems developer | Female | Secondary care | Face-to-face interview |
| 6 | Researcher | Male | Research institution | Face-to-face interview |
| 7 | Researcher | Male | Research institution | Face-to-face interview |
| 8 | GP practice manager | Female | Primary care | Face-to-face interview |
| 9 | Clinical lead | Male | Primary care | Face-to-face interview |
| 10 | GP practice administrator | Female | Primary care | Face-to-face interview |
| 11 | PCT data quality manager | Female | Commissioning | Face-to-face interview |
| 12 | GP practice information manager | Male | Primary care | Face-to-face interview |
| 13 | Diabetes dietician | Female | Secondary care | Face-to-face interview |
| 14 | Diabetes specialist nurse | Female | Secondary care | Face-to-face interview |
| 15 | Head of midwifery | Female | Secondary care | Face-to-face interview |
| 16 | Clinical coding manager | Female | Secondary care | Face-to-face interview |
| 17 | Hospital pharmacist | Female | Secondary care | Face-to-face interview |
| 18 | Clinical coding manager | Female | Secondary care | Face-to-face interview |
| 19 | Research and audit assistant | Female | Unscheduled care | Face-to-face interview |
| 20 | Clinical improvement officer/paramedic | Male | Unscheduled care | Face-to-face interview |
| 21 | Patient 1 | Female | Primary care | Face-to-face interview |
| 22 | Patient 2 | Male | Primary care | Face-to-face interview |
| 23 | Patient 3 | Male | Primary care | Face-to-face interview |
| 24 | Clinical information and records assistant | Female | Unscheduled care | Face-to-face interview |
| 25 | Clinical information and records assistant | Female | Unscheduled care | Face-to-face interview |
| 26 | Clinical coding manager | Female | Unscheduled care | Telephone interview |
| 27 | Senior academic | Female | Research institution | Face-to-face interview |
GP, general practitioner; PCT, primary care trust.
We report our findings under four main themes to reflect current debate regarding the benefits and risks associated with the introduction of EHRs: clinical documentation practice and coding processes; patient care benefits; secondary uses of data; informing and involving patients. A summary of the identified benefits and risks is provided in box 2.
Box 2. Identified benefits and risks of increasing structuring and coding within the electronic health record.
Benefits
Provision of clear information to support patient understanding and involvement in care, for example, in self-management of long-term conditions such as diabetes, and improved self-administration of medication.
Facilitation of patient provision of administrative and intimate information, for example, using forms or kiosks for computerized data collection.
Reduction of duplication and more effective use of information, including reduction of time spent in clinic explaining information.
Exchange of information across clinical and social settings within integrated electronic health records to allow new forms of continuity of care.
Consistent complaints handling and investigations into practice.
Reporting for individual clinicians (eg, for inclusion in appraisal).
Secondary uses, including early alerting of epidemics, identification of particular patterns and trends within patient populations, accelerating awareness of new conditions, commissioning and re-imbursement, education and research, and data mining and cross-sectoral linkages (eg, health and education).
Risks
Inappropriate application of precise codes when a diagnosis is not clear, or incorrect and/or inaccurate retrospective coding.
Use of structured information may be unfamiliar to patients and insensitive in some contexts, where it is felt to stereotype or carry inherent social judgments, for example, regarding obesity. Allowing the patient to see coded information would be particularly inappropriate and possibly counterproductive for the patient. Medical terms should not dominate descriptions of the patient experience of being unwell.
Patient concern regarding what might happen to computerized information as a result of access by legitimate organizations (eg, insurance companies).
Ambiguity and inconsistency in documentation due to the absence of national guidelines, lack of specificity within guidelines, or ambiguity due to local and organizational arrangements.
Duplication of effort due to lack of co-ordination and dissemination of best practice in devising and using information structures.
Different documentation practices between and within professional communities challenge common assumptions regarding collation, comprehension, sharing, and understanding of structured information.
Lack of awareness among clinicians as to how data were being used beyond immediate clinical care and the notable impact of incentives and re-imbursement on structuring and coding practices detract from clinicians’ engagement in this debate and thus potential benefit for direct care.
Variations in clinical documentation practice and the process of coding
We identified several examples of inadequate coding due to variations in the highly interpretive processes of recording clinical information and assigning of clinical codes. We identified some attempts at standardization as a dimension of clinical practice, for example, by midwives. However, we also identified variations in the information structures used by healthcare professionals in the same profession. These local variations resulted from a range of factors including the absence of or lack of detail in some guidelines and/or ambiguity arising due to differences between healthcare providers:
Every ambulance service in the UK has a different patient record… All ambulance services have different codes. (I.26, Clinical coding manager, Unscheduled care)
Variations were compounded by contrasting perspectives on the usefulness and availability of data across clinical specialties and care settings. The sheer range and number of healthcare professionals involved in clinical care provision made it challenging to achieve consensus among multi-professional user groups as to how best to structure information, even within the same computer application. In practice, some healthcare professionals were keeping alternate sets of documentation in locally derived formats. This duplicate documentation was in part attributed to the unavailability of computer systems and/or notes, for example, when patients moved between treatment rooms within an outpatient department that did not have access to inpatient records:
We dieticians keep two sets of records really, one in the patient's medical notes and we have our own patient cards. We do that really only because we never reliably get the patients notes every time they come to see us. (I.13, Diabetes dietician, Secondary care)
The assigning of codes to clinical information was at times a concern due to the inherent challenges in firmly establishing a diagnosis in many cases and the implications of clinical decisions. The collection of information within a health record utilized highly interpretative processes within very short time frames, including not only a clinician's decision-making about the information received, but also what took priority within that information and how it was to be accounted for. Further interpretive processes were required in the assignation of codes and we noted examples where the design of coding systems and coding practices led to inaccurate data, for example, when the procedure was coded instead of a history of a procedure or status post-procedure.
We also identified a need to accommodate ambiguity during diagnosis and non-standard outcomes. In some cases, clinical entries were deliberately made imprecise to reflect uncertainty within diagnostic processes, either leading to the use of less specific codes that were broad enough to capture that imprecision or to bypass the use of overly-precise codes. Issues regarding the labeling of patients and use of language, particularly in relation to conditions with implications for a person's status as a competent individual (such as dementia) or associated social stigma (such as obesity), were also felt to influence documentation and coding as practitioners expressed reluctance to use terminology that might be found pejorative.
Patient care benefits
In exploring the interpretive processes involved in assigning codes to narrative information, we noted the extent of flexibility allowed in everyday work organization and practice styles. While strategic discussions regarding the benefits of increasing structuring and/or coding within the health record often focused on the benefits of the sharing of knowledge about individual patients across care settings, this featured very little in discussions with staff providing direct care. The sharing of information was considered potentially problematic due to the significant variation in practices across locations, care settings, and professional communities.
Within our expert discussion groups, descriptions of local, specialty-specific systems indicated pockets of knowledge and expertise where structured information was being used to improve clinical care. However, these systems were often domain-specific (eg, within a particular specialty, professional group, or care setting) and not always widely available or utilized to their full potential. For example, while one consultant working within a breast cancer clinic provided organized, coded test results to general practitioner (GP) practices to speed up information exchange, another oncologist declined to do so as a matter of person preference. There appeared to be no national co-ordination of these initiatives or natural forum for sharing best practice, resulting in an undue emphasis on word of mouth and informal networks to promote best practice and innovation.
These local variations in information collection were also evident in the uses that these coded data were put to. For example, we identified a number of examples of coded data being used to facilitate the identification of particular patterns and trends within patient populations during clinical practice, accelerating research into new conditions, and drawing on and informing clinical practice deliberations such as the early identification of the influenza epidemic and specific detection of a relationship between anticoagulation and flu vaccination:
We were one of the first people to realize that the flu epidemic for instance last year, avian flu. The avian flu vaccine created havoc with people's anticoagulation… suddenly we twigged and we reported it. (I.4, Clinical lead, Secondary care)
We learned of information structures that had been used to promote patient-centered approaches to care and enable patient self-management, for example, in the use of computerized patient diaries and electronic forms to collect information prior to consultation with a healthcare professional. This offered particular benefits in the management of long-term conditions such as diabetes, for example, consistent meal time recording by patients of their blood glucose levels prior to a clinical review. Despite these tangible benefits, it was not clear how these local examples of best practice could be more widely introduced.
Secondary uses of data
Some data collected within healthcare services were used by local, regional, and national bodies, for example, primary care trusts (PCTs) and the English NHS Hospital Episode Statistics (HES) service. Data were used to assist with service planning, audit, commissioning, and research. This process appeared to be poorly understood by healthcare professionals working directly with patients other than in relation to reimbursement and related incentives:
I can't think of a single GP, even myself working as a GP wouldn't think about how it might be useful for research. No, it's entirely for clinical use, entirely for your own clinical use, for you and your other colleagues in your practice and for medico-legal purposes for recording what you've done and what you haven't done. (I.7, Researcher, Research institute)
This lack of awareness as to how data were used beyond immediate clinical care was accompanied by speculation that commissioning bodies could ‘pick up information, any information they like basically on patients’ (I.8, GP practice manager, Primary care). The patients we interviewed also wondered about the availability and use of computerized information by healthcare professionals. In addition to familiar security concerns (such as information on stolen laptops), patients were concerned about what might happen to this information as a result of access by legitimate organizations:
If you, you know, there was an issue that you didn't particularly want revealed to say insurance people, could they tap into your medical records? (Interview 21, Patient 1, Primary care)
I mean I'm retired now but if you were going for a job could they tap into your records? That is a worry. (Interview 22, Patient 2, Primary care)
Perceptions and attitudes towards coding embedded within organizations were perceived to impact upon clinical staff's willingness to engage with coding, and upon their understandings of the functions and utility of coding. One of the driving forces behind the structuring and/or coding of health records related to the organization of healthcare and the need to report on and account for activity to secure re-imbursement (see box 3). We found that clinical staff often did not see clinical coding as part of their job, but rather as a retrospective process done for administrative purposes.
Box 3. Two key reimbursement methods in the National Health Service (NHS) in England.
Primary care
Scheme: Quality and Outcomes Framework (QOF): the national primary care pay-for-performance scheme introduced in April 2004 as part of the new General Medical Services (GMS) contract
Coding terminology: use of Read Codes within GP IT systems
Secondary care
Scheme: Payment by Results (PbR) scheme, a rule-based system for paying secondary care providers from NHS funds
Coding terminology: predominantly from the International Classification of Diseases (10th Revision) (ICD-10) diagnostic coding – variations in the practice of documentation
Informing and involving patients
The importance of interpersonal and contextual factors when collecting and communicating patient information was highlighted. A non-judgmental and honest environment was considered essential. In some cases, forms and templates presented within a familiar context were felt to have increased patient involvement in care and facilitated more accurate recording and self-management, for example, obstetric and diabetic care. Forms were noted as a useful tool in the collection of intimate information, for example, where a patient was less embarrassed to provide in writing sensitive information they felt they may be judged upon, such as alcohol consumption or substance misuse:
I use it, it's usually with people who don't really, I know that they're gonna struggle to find something to talk about themselves and I'm trying to engage them with their health care. So I might sit with them and help them fill it in or I'll say would you like me to tick and I'll just read it to you. (Interview 14, Diabetes specialist nurse, Secondary care)
One method by which patients were contributing to authorship of their own records was in the use of self-service kiosks in outpatient settings (figure 1). We observed this technology being used as an independent interface with patients in a way that was familiar due to patient experiences with similar kiosks in supermarkets and during airline and train travel. These kiosks allowed patients to check in to a clinic and to review and amend the administrative data held about them within EHRs. This had allowed a significant reduction in patient queuing times when booking in to clinics, which in turn reduced queuing for follow-up appointments and other administration post-consultation. They were described as having improved confidentiality as patient information could not be overheard, in addition to improving access for wheelchair users and minority groups (by offering five languages), providing options for those with visual impairments, and reducing the impact of hearing impairment. Presenting coded information to patients in a readable form allowed them to more easily update or correct it, ensuring that self-declared facts such as ethnicity were accurate. By involving patients in this manner, processes had been automated to release manpower while at the same time improving the accuracy of administrative data within the health record.
Figure 1.

Self-service check-in kiosk.
While patients were unsure about how information recorded during their care might be used by others, they recounted the problems they had with processing the information received about their care. They noted how these problems impacted upon healthcare professionals’ time, describing how they contacted surgeries and attended clinics to gain information or have things explained in a way they could understand:
And I mean some of the technical terms are not known to Joe Bloggs, I mean, you know, you've got to have ology's to understand them, some of the phrases. What I tend to do is I see Dr. [name] more often than I do Dr. [name] and I just say am I alright to take these even if it's only aspirin or Anadin or something, am I alright to take this with that. (I.23, Patient 3, Primary care)
The technology available to patients was felt to be increasing patient desire for information and encouraging them to be proactive in their own healthcare. Examples of this were given in relation to patients managing their own long-term conditions, for example, diabetes, and anti-coagulant medication:
Certainly we get in patients who are self-testing, self-managing and our intent is to make them able to access their own data directly without going through any of the bureaucracy. But only their own data… to download and do whatever they want with it, it's theirs. (I.4, Clinical lead, Secondary care)
Participants further stated that medications management was an area that could greatly benefit from the provision of structured information to and from patients, allowing patients a greater understanding of what they should be doing, and more accurate reporting of what they were doing. There was also the potential for informed patients to be more involved in medicines administration:
The next stage is that we've suggested to some patients an interest that might want to go the whole hog and do self-management and this is where they do the lot, within parameters and they will test their blood as they are doing at the moment but they will then dose themselves. (I.17, Hospital pharmacist)
However, healthcare professionals stressed that levels of literacy and language were not to be automatically assumed when communicating with patients.
While providing information in a structured format was recognized as important for patient information and understanding, professionals were concerned that the use of coded information may be unfamiliar to patients and the displayed value of the code(s) allocated may prove highly insensitive, for example, when related to a condition carrying inherent social stigma such as obesity. It was felt to be particularly inappropriate and possibly counterproductive for the patient when providing information out of context and/or by allowing medical terms to dominate descriptions of the patient experience of being unwell.
Discussion
Summary of findings
Our findings have highlighted the variations in recording practice and extent of usage of the information collected during the provision of individual clinical care, including in the organization of healthcare and for secondary uses relating both to healthcare and to domains beyond healthcare (figure 2). With the exception of a few key examples, stakeholders reported that most of the gains thus far from structured and/or coded records had been for population health sciences, clinical research, and health service management purposes, or for reimbursement. While we noted a number of specific examples of immediate value to be gained by clinicians and patients in the provision of clinical care from the increased use of structuring and/or coding within health records, we also identified significant risks (box 2).
Figure 2.
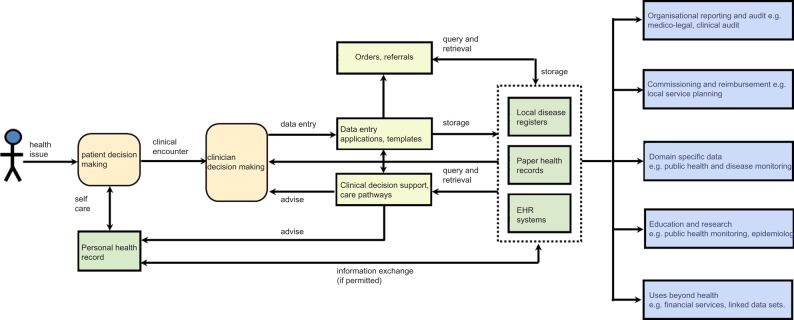
Health records and the information journey. EHR, electronic health record.
Strengths and limitations
A particular strength of this exploratory study is its isolation of structuring and/or coding within health records as a subject of qualitative enquiry across a wide range of stakeholders. We noted that discussions about the recording and use of health records were not commonly framed in terms of structuring and/or coding even though this represents a significant change in documentation practices arising from, and underpinning, the increased use of EHRs. While structure was a major factor in the practice of collection and interpretation of information, it was not routinely discussed. Indeed, we spent time during research data generation to reflect upon how we might frame our investigation using language and ideas familiar to participants given the complexity of the subject. We sought to reflect the full spectrum of stakeholders likely to be interested in and impacted by this issue, but it is possible that this may not have been adequately achieved. Given the relatively small-scale nature of this study, care therefore needs to be taken in assessing the likely transferability of this work to other populations, contexts, and settings. For example, we were unable to explore international dimensions, or conduct in-depth investigation within particular specialties within the time and resources available, so these should be seen as areas for further potential enquiry that can build on this initial work.
Considering our findings in the light of the existing literature
The exchange of information during clinical care is a highly interpretative process that draws on personal relationships, tacit knowledge, and intuitive understanding within clinical decision-making.9 10 This highlights the importance of the clinical narrative as a source of information to support decision-making.44 45 The proliferation of local systems indicates known advantages of flexible paper-based systems and small scale EHRs and the use of tools and techniques to structure information within specific clinics or specialties.6 46–49 However, inconsistencies in practice may be exacerbated by the negotiated nature of local systems development. Informal local practices and limited sharing of best practice present the potential for significant duplication of effort (eg, entering information in more than one system) and increased potential for human error (eg, when retrospectively transferring patient information from paper to computer), particularly where locum staff or those undergoing rotational training are asked to adapt to local styles of documentation.
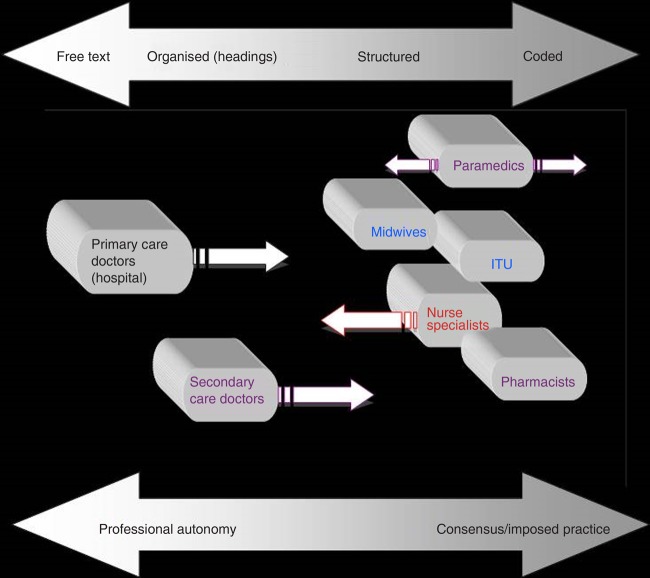
Assumptions regarding a common approach to the collation, comprehension, and understanding of computable information underpin the anticipated benefits of shared EHRs.5 50 However, we identified important nuances of interpretation of structured information that may only be clarified within the context of associated free text. Variations in the use of structuring and/or coding in EHRs (figure 3) may, for example, be due to local custom and practice, an absence of professional guidelines, the use of locally determined protocols, organization-specific requirements, commissioning and audit requirements, or medico-legal considerations. This indicates that some of the issues attributed to the use of paper-based records, such as inconsistent content and difficulties in sharing and comparing records,51–53 may not be fully addressed by the introduction of EHRs. Given the contingent nature of clinical processes, any increased use of structuring and/or coding should respect patient and clinician individuality and non-standard clinical outcomes while at the same time facilitating best practice in clinical care. We suggest, therefore, that the standardization of data collection and storage required within EHRs should, wherever possible, be subject to empirical assessment of the benefits and risks associated with changes to documentation practices and the organization of related tasks.
Figure 3.
Healthcare professionals’ use of structuring and coding in the health record. ITU, intensive therapy unit.
Conceptually, the increased use of structuring and/or coded information within medical records may standardize how information is stored and exchanged.54 55 In practice, we identified important differences of understanding and perceived utility across the diverse range of healthcare providers, secondary use services, commissioners, and patients consulted.56 Our findings showed low awareness of the potential value of information exchange among those providing care, and healthcare professionals were concerned that they were being asked to populate treasure troves of information for the benefit of others. This is a potential barrier to change, particularly as only limited work has been done to consider the impact of this additional workload for individuals.11 12 57 58 A further barrier is the limited evidence of immediate benefits in support of clinical care, such as decision-support to reduce errors, and a failure to provide audit information to support individual clinicians (eg, for professional development and appraisal). In view of the importance of patient data to the optimization of effective and efficient healthcare provision, those engaged in care processes should be directly incentivized to provide complete and consistent data, as has been the case in the USA, for example.5 Indeed, future debate may consider more direct penalties for not doing so.
While acknowledging the importance of patient data for the optimization of effective and efficient healthcare provision, our findings also highlight important considerations regarding the recording of sensitive patient information. Increased patient education and awareness of the ways in which their information is documented and used would help to inform patients in relation to their personal privacy and confidentiality. Furthermore, information gathered during processes of care is recorded in biomedical language within a medical context. Such terminology may be stigmatizing when considered in non-medial contexts, for example, use of the term ‘morbidly obese.’ Levels of literacy, language skills, and cultural norms will influence interpretations of medical information and should be considered when communicating information to avoid judgmental connotations and mitigate potential concerns.
There is significant potential for the trial and introduction of more structured feedback to patients (eg, through charts and diagrams) to improve the accessibility of this information for patients and family carers. That said, we caution against the use of coded information that may falsely imply certainty within diagnostic processes and may adversely impact upon patients and the patient/clinician relationship, for example, by creating undue alarm or causing confusion. This may well present a new challenge to the dominance of biomedical models of recording. We recommend further consideration and development of non-medical information models, for example, the problem-orientated health record59 and the inclusion of patient stories.60 61 Given that the modification of health records was central to major reform of medical care in the 20th century,62 the consequences of patient-focused approaches to documentation may only be evident in the long term.
Conclusions
The design and development of meaningful EHRs requires equal attention to the capture of narrative communication between patients and clinicians, and administrators’ and researchers’ need for accurate, computable data. National reporting requirements for the reimbursement of primary care services have successfully influenced the structuring and coding of clinical information. However, a lack of perceived relevance to direct care has inhibited clinician interest and more immediate benefits must be offered to engage healthcare professionals in often time-consuming data processing. Further alignment between guidelines relating to clinical practice and recommendations for the comprehensive and accurate processing of clinical data would support related national policy developments.
Many of the risks we identified related to the appropriateness of structured and/or coded information for patients. We note the possibility of unanticipated consequences, most particularly unintended impacts upon clinician/patient interactions. These risks highlight the need for new models of documentation if health records are to be read and indeed authored by patients. Given the potential benefits and risks, recommendations relating to different levels of structuring and coding health records should be isolated for empirical investigation to allow evidence-based implementation focusing on outcomes and benefits.
Supplementary Material
Acknowledgments
We gratefully acknowledge the advice on this research which has been provided by members of the Independent Project Steering Committee overseeing our program of work into the structuring and coding of the clinical record. Chaired by Professor Simon de Lusignan, this group also comprises Dr Nick Booth, Dr Stephen Kay, and Lee Priest. We are grateful to Professor Brian McKinstry, Dr Hilary Pinnock, and the reviewers for their constructive suggestions on an earlier draft of this manuscript.
Footnotes
Contributors: BF, DK, ZM, and AS conceived the idea for this study. ZM and BF conducted the interviews and data gathering. BF, DK, ZM, KC, and AS analyzed the data. ZM drafted the manuscript, with AS, DK, BF, and KC commenting on and editing several drafts. AS was the Principal Investigator. All authors approved the final manuscript.
Funding: This work was funded by the NHS CFH Evaluation Programme (NHS CFHEP 009). The views expressed in this publication are those of the authors and not necessarily those of the NHS, the NHS CFH Evaluation Programme or the Department of Health. AS is supported by a Harkness Health Policy and Practice Fellowship from The Commonwealth Fund.
Competing interests: We declare that (1) all authors have support in the form of a grant from the NHS Connecting for Health Evaluation Programme for the submitted work; (2) no author has a relationship with any company that might have an interest in the submitted work in the previous 3 years; (3) no author's spouse, partner or children have financial relationships that may be relevant to the submitted work; and (4) no author has non-financial interests that may be relevant to the submitted work.
Ethics approval: We received ethics approval for this work from the National Research Ethics Service—Brighton West Ethics Committee (MREC Ref: 10/H1111/25). Governance approval was obtained for each participating organization. Where possible, written informed consent was sought from all participants, although in some cases, such as telephone interviews, verbal consent was accepted. All data were anonymized to protect the confidentiality of both participant organizations and individual interviewees.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Blumenthal D. Launching HITECH. N Engl J Med 2010;362:382–5 [DOI] [PubMed] [Google Scholar]
- 2.Black AD, Car J, Pagliari C, et al. The impact of eHealth on the quality and safety of health care: a systematic overview. PLoS Med 2011;8:e1000387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Department of Health. The power of information: putting all of us in control of the health and care information we need. 21 May 2012. http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH_134181 (accessed 24 May 2012).
- 4.Department for Business Innovation and Skills. Strategy for UK Life Sciences, December 2011. https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/32457/11-1429-strategy-for-uk-life-sciences.pdf (accessed 8 Feb 2012).
- 5.Morrison Z, Robertson A, Cresswell K, et al. Understanding contrasting approaches to nationwide implementations of electronic health record systems: England, the USA and Australia. J Healthc Eng 2011;2:25–42 [Google Scholar]
- 6.Fernando B, Kalra D, Morrison Z, et al. Benefits and risks of structuring and coding the presenting patient history in the electronic health record: systematic review. BMJ Qual Saf 2012;21:337–46 [DOI] [PubMed] [Google Scholar]
- 7.Lilford RJ, Thornton JD. Decision logic in medical practice. The Milroy Lecture 1992. J R Coll Physicians 1992;26:400–12 [PMC free article] [PubMed] [Google Scholar]
- 8.De Lusignan S. Codes, classifications, terminologies and nomenclatures: definition, development and application in practice. Inform Prim Care 2005;13:65–9 [DOI] [PubMed] [Google Scholar]
- 9.Butler CC, Evans M, et al. The ‘heartsink’ patient revisited. Br J Gen Pract 1999;49:230–3 [PMC free article] [PubMed] [Google Scholar]
- 10.Goldstein-Jutel A. Putting a name to it: diagnosis in contemporary society. Baltimore: John Hopkins University Press, 2011 [Google Scholar]
- 11.De Lusignan S. The barriers to clinical coding in general practice: a literature review. Med Inform Internet Med 2005;30:89–97 [DOI] [PubMed] [Google Scholar]
- 12.O'Dowd A. Coding errors in NHS cause up to £1bn worth of inaccurate payments. BMJ 2010;341:c4734 [Google Scholar]
- 13.The Scottish Government. The healthcare quality strategy for NHS Scotland. 2010. http://www.scotland.gov.uk/Resource/Doc/311667/0098354.pdf (accessed 27 Oct 2013). [Google Scholar]
- 14.The Scottish Government. Patient Rights (Scotland) Act. 2011. http://www.legislation.gov.uk/asp/2011/5/contents (accessed 27 Oct 2013). [Google Scholar]
- 15.Greist JH, Laughren TP, Gustafson DH. A computer interview for suicide-risk prediction. Am J Psychiatry 1973;130:1327–32 [DOI] [PubMed] [Google Scholar]
- 16.Porter SC, Silvia MT, Fleisher GR, et al. Parents as direct contributors to the medical record: validation of their electronic input. Ann Emerg Med 2000;35:346–52 [DOI] [PubMed] [Google Scholar]
- 17.Porter SC, Kohane IS. Optimal data entry by patients: effects of interface structure and design. Stud Health Technol Inform 2001;84(Pt 1):141–5 [PubMed] [Google Scholar]
- 18.Hershey CO, Grant BJB. Controlled trial of a patient-completed history questionnaire: effects on quality of documentation and patient and physician satisfaction. Am J Med Qual 2002;17:126–35 [DOI] [PubMed] [Google Scholar]
- 19.O'Connell R, Poljak A, Powsner S, et al. Forms that inform. Methods Inf Med 2004;43:247–55 [PubMed] [Google Scholar]
- 20.Porter SC, Forbes P, Manzi S, et al. Patients providing the answers: narrowing the gap in data quality for emergency care. Qual Saf Health Care 2010;19:e34. [DOI] [PubMed] [Google Scholar]
- 21.Engel GL. The need for a new medical model: a challenge for biomedicine. Science 1977;196:129–36 [DOI] [PubMed] [Google Scholar]
- 22.Donnelly WJ. Righting the medical record. JAMA 1988;260:823–5 [PubMed] [Google Scholar]
- 23.Smith RC, Hoppe RB. The patient's story: integrating the patient- and physician-centered approaches to interviewing. Ann Intern Med 1991;115:470–7 [DOI] [PubMed] [Google Scholar]
- 24.Fisher B, Bhavnani V, Winfield M, et al. How patients use access to their full health records: a qualitative study of patients in general practice. J R Soc Med 2009;102:539–44 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Donnelly WJ. Taking suffering seriously: a new role for the medical case history. Acad Med 1996;71:730–7 [DOI] [PubMed] [Google Scholar]
- 26.Berg M. Medical work and the computer-based patient record: a sociological perspective. Methods Inf Med 1998;37:294–301 [PubMed] [Google Scholar]
- 27.Crowe S, Cresswell K, Robertson A, et al. The case study approach. BMC Med Res Methodol 2011;11:100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.George A, Bennett A. Case studies and theory development in the social sciences. Cambridge, MA: MIT Press, 2005 [Google Scholar]
- 29.Stake RE. The art of case study research. London: Sage, 1995 [Google Scholar]
- 30.Yin R. Case study research, design and methods. Sage, 2009 [Google Scholar]
- 31.Aarts J, Doorewaard H, Berg M. Understanding implementation: the case of a computerized physician order entry system in a large Dutch university medical center. J Am Med Inform Assoc 2004;11:207–16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Chiasson MW, Davidson E. Pushing the contextual envelope: developing and diffusing IS theory for health information systems research. Info Organ 2004;14:155–88 [Google Scholar]
- 33.Coiera E. Four rules for the reinvention of health care. BMJ 2004;328:1197–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Doolin B. Sociotechnical networks and information management in health care. Account Manag Info Technol 1999;9:95–114 [Google Scholar]
- 35.Pare G. Implementing clinical information systems: a multiple-case study within a US hospital. Health Serv Manage Res 2002;15:71–92 [DOI] [PubMed] [Google Scholar]
- 36.Prout A. Actor-network theory, technology and medical sociology: an illustrative analysis of the metered dose inhaler. Sociol Health Illn 1996;18:198–219 [Google Scholar]
- 37.Yusof MM, Kuljis J, Papazafeiropoulou A, et al. An evaluation framework for health information systems: human, organization and technology-fit factors (HOT-fit). Int J Med Inform 2008;77:386–98 [DOI] [PubMed] [Google Scholar]
- 38.Silverman D. Doing qualitative research, a practical handbook. London: Sage, 2000 [Google Scholar]
- 39.Britten N. Qualitative research: qualitative interviews in medical research. BMJ 1995;311:251–3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Barbour R. Introducing qualitative research. London: Sage, 2008 [Google Scholar]
- 41.Glaser BG, Strauss AL. The discovery of grounded theory. Chicago: Aldine, 1967 [Google Scholar]
- 42.Alvesson M, Sköldberg K. Reflexive methodology: new vistas for qualitative research. London: Sage, 2000 [Google Scholar]
- 43.Morse J. The significance of saturation. Qual Health Res 1995;5:147–9 [Google Scholar]
- 44.Greenhalgh T. Narrative based medicine in an evidence based world. BMJ 1999;318:323–5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kay S, Purves IN. Medical records and other stories: a narratological framework. Methods Inf Med 1996;35:72–87 [PubMed] [Google Scholar]
- 46.Greenhalgh T, Potts HW, Wong G, et al. Tensions and paradoxes in electronic patient record research: a systematic literature review using the meta-narrative method. Milbank Q 2009;87:729–88 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Lilford RJ, Bingham P, Fawdry R, et al. The development of on-line history-taking systems in antenatal care. Methods Inf Med 1983;22:189–97 [PubMed] [Google Scholar]
- 48.Mcadam WA, Brock BM, Armitage T, et al. Twelve years’ experience of computer-aided diagnosis in a district general hospital. Ann R Coll Surg Engl 1990;72:140–6 [PMC free article] [PubMed] [Google Scholar]
- 49.Slack WV, Bleich HL. The CCC system in two teaching hospitals: a progress report. Int J Med Inform 1999;54:183–96 [DOI] [PubMed] [Google Scholar]
- 50.Coiera E. Building a national health IT system from the middle out. J Am Med Inform Assoc 2009;16:271–3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Weed LL. Medical records that guide and teach. N Engl J Med 1968;278:652–7 [DOI] [PubMed] [Google Scholar]
- 52.Rector AL. Clinical terminology: why is it so hard? Methods Inf Med 1999;38:239–52 [PubMed] [Google Scholar]
- 53.Dick RC, Steen EB, Detmer DE. The computer-based patient record. Washington, DC: National Academies Press, 1997 [PubMed] [Google Scholar]
- 54.Sheikh A, Cornford T, Barber N, et al. Implementation and adoption of nationwide electronic health records in secondary care in England: final qualitative results from a prospective national evaluation. BMJ 2011;343:d6054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Robertson A, Cresswell K, Takian A, et al. Implementation and adoption of nationwide electronic health records in secondary care in England: qualitative analysis of interim results from a prospective national evaluation. BMJ 2010:341:c4564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Almann P, Micael J. Successful delivery of information technology in the NHS. BMJ 2011;343:d6663. [DOI] [PubMed] [Google Scholar]
- 57.Patel VL, Kushniruk AW, Yang S, et al. Impact of a computer-based patient record system on data collection, knowledge organization, and reasoning. J Am Med Inform Assoc 2000;7:569–85 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Karsh B, Beasley JW, Hagenauer ME. Are electronic medical records associated with improved perceptions of the quality of medical records, working conditions, or quality of working life? Behav Inform Technol 2004;23:327–35 [Google Scholar]
- 59.Weed LL. Medical records, medical education, and patient care: the problem-orientated record as a basic tool. Cleveland, OH: Press of Case Western Reserve University, 1969 [Google Scholar]
- 60.Smith RC, Hoppe RB. The patient's story: integrating the patient- and physician-centered approaches to interviewing. Ann Intern Med 1991;115:470–7 [DOI] [PubMed] [Google Scholar]
- 61.Donnelly WJ. Viewpoint: patient-centered medical care requires a patient-centered medical record. Acad Med 2005;80:33–8 [DOI] [PubMed] [Google Scholar]
- 62.Reiser SJ. The clinical record in medicine. Part 2: reforming content and purpose. Ann Intern Med 1991;114:980–5 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.