Abstract
Caecal volvulus is a rare cause of intestinal obstruction, with the bascule subtype accounting for <10% of all cases of caecal volvulus. It is associated with significant morbidity and mortality if left undiagnosed. We present the case of a 58-year-old female who presented to our surgical department with symptoms of intestinal obstruction. She had various radiological investigations, which supported the diagnosis of a caecal volvulus of the bascule subtype. She was subsequently managed surgically and had a right hemicolectomy and ileocolic anastomosis. Her recovery was uneventful and she was discharged within 1 week of having her operation. Fortunately, caecal volvulus of the bascule subtype is rarely encountered; however, clinicians need to be aware of its presentation and subsequent management options so that clinical outcomes are improved.
INTRODUCTION
Worldwide, tumours account for the majority of cases of large bowel obstruction with diverticular disease and volvulus accounting for the remainder. Volvulus commonly affects the sigmoid, caecum and transverse colon in the decreasing order of frequency with caecal volvulus accounting for <1% of causes of large bowel obstruction [1]. Additionally, the bascule subtype accounts for <10% of cases presenting with caecal volvulus. We present the case of a 58-year-old patient who presented with symptoms of intestinal obstruction and had characteristic radiological findings of a caecal volvulus—bascule subtype.
CASE REPORT
A 58-year-old female with a past medical history of a large intrathoracic hiatus hernia presented to her general practitioner and was subsequently referred to our surgical department with symptoms of sudden onset severe epigastric pain associated with vomiting and abdominal distension. Her abdomen was generally tender, maximally in the epigastric region, although she was not peritonitic. The admission erect chest radiograph showed a large hiatus hernia and an elevated right hemidiaphragm with a large loop of distended bowel (Fig. 1). Subsequent computed tomography (CT) scan demonstrated an almost completely intrathoracic stomach with a degree of volvulus, and the liver medially displaced by a loop of large bowel felt to be caecum (Fig. 2). Since the patient remained otherwise well, bidirectional endoscopy was performed, and given that a volvulus point could not be identified and the ileocaecal junction was not identified, contrast studies were requested (Figs 3–5) which demonstrated an incomplete obstruction caused by a volved caecum rotated anteriorly and cephalad.
Figure 1:
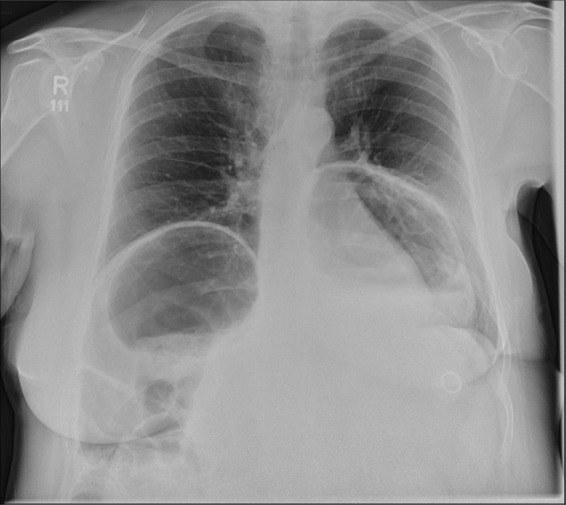
Erect chest radiograph, showing a large hiatus hernia and large loop of bowel elevating the right hemidiaphragm.
Figure 2:

CT coronal section demonstrating caecum medially displacing the liver and causing an upward pressure on the right hemidiaphragm.
Figure 3:

A large bowel contrast study showing the flow of contrast from the collapsed transverse colon into the dilated, upwardly displaced caecum.
Figure 4:

Coronal section of contrast-enhanced CT demonstrating contrast filling upwardly displaced caecum.
Figure 5:

Axial section of contrast-enhanced CT demonstrating ‘whirl sign’ at the point of volvulus.
After the contrast study partial resolution of symptoms occurred but given the development of free fluid in her contrast CT scan, the decision was taken to manage her surgically. A midline laparotomy was performed, with the finding of a freely mobile, grossly distended caecum flipped anteriorly over the ascending colon as demonstrated on her CT scan (Fig. 6). This was therefore removed with a right hemicolectomy and primary ileo-colic anastomosis. Additionally, there was no evidence of a gastric volvulus (suggesting partial twisting) and since her stomach was completely intra-abdominal, there was no need to address her hiatus hernia at that point in time. The patient was admitted to the high dependency unit post-operatively, made a good recovery and was discharged home within a week of surgery.
Figure 6:

Freely mobile, distended caecum found on opening.
DISCUSSION
Caecal volvulus accounts for 1% of all causes of large bowel obstruction [1, 2]. The mechanism of caecal volvulus has been well documented and can be explained by the presence of an excessively mobile caecum or incomplete fixation of the ascending colon to the retroperitoneum during embryogenesis. Additionally, caecal volvulus can be described as organoaxial (true caecal or caecocolic volvulus) or mesenteroaxial (caecal bascule) [3]. The latter describes the folding of the caecum anteriorly over the ascending colon and accounts for 10% of all caecal volvulus [4], while the former describes the twisting of the terminal ileum, caecum and ascending colon. Interestingly, our patient had an incidental finding of a gastric volvulus on imaging, the aetiology most likely related to her large hiatus hernia, a known risk factor for gastric volvulus. The embryological theory as highlighted above for volvuli affecting the large bowel may also be applicable to the stomach.
A review of 561 patients with caecal volvulus found that they commonly presented with symptoms of bowel obstruction—abdominal pain, abdominal distension, constipation, nausea and vomiting. Physical findings included abdominal distension, hyperperistalsis, peritoneal signs, abdominal mass and absent bowel sounds [3]. It is reasonable to assume that patients with the bascule subtype may have intermittent subacute obstruction due to the flopping of the caecum back into its anatomical position. Additionally, this subtype is less likely to strangulate as the mesentery is not frequently twisted when compared with the organoaxial subtype. Risk factors commonly described for caecal volvulus include previous abdominal surgery, high fibre intake, chronic constipation and distal obstruction [5–7].
Radiological imaging is useful in diagnosing caecal volvulus. Rosenblat et al. [8] found that CT findings of whirl, ileocaecal twist, transition points, X marks the spot and split wall have high specificity for caecal volvulus. Additionally, they found that the absence of distal colonic decompression made the diagnosis of caecal volvulus unlikely. Diagnostic confusion may exist between sigmoid and caecal volvulus; however, the location of the mesenteric twist (CT whirl sign) is highly accurate in distinguishing the two [9]. This whirl sign, as first published by Fisher [10], describes ‘swirling strands of soft tissue attenuation within a background of fat attenuation and gives the appearance of a hurricane on a map’. Barium enema has been historically used to confirm the presence of a volvulus, assess the distal colon and may also have a therapeutic effect [3].
Factors such as patient co-morbidities and the viability of the bowel should be taken into account when managing caecal volvulus. The authors agree that right hemicolectomy is associated with the lowest recurrence and complication rates compared with detorsion alone, detorsion and caecopexy and caecostomy [4]. Additional options when faced with non-viable bowel and where primary anastomosis is not suitable include ileostomy and mucus fistula. Minimally invasive procedures may play a role in the management of patients without perforation or gangrenous bowel and provides a reasonable treatment option for this condition.
REFERENCES
- 1.Habre J, Sautot-Vial N, Marcotte C, Benchimol D. Caecal volvulus. Am J Surg. 2008;196:e48–9. doi: 10.1016/j.amjsurg.2007.11.029. [DOI] [PubMed] [Google Scholar]
- 2.Ballantyne GH, Brandner MD, Beart RW, Ilstrup DM. Volvulus of the colon: incidence and mortality. Ann Surg. 1985;202:83–92. doi: 10.1097/00000658-198507000-00014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rabinovici R, Simansky DA, Kaplan O, Mavor E, Manny J. Cecal volvulus. Dis Colon Rectum. 1990;33:765–9. doi: 10.1007/BF02052323. [DOI] [PubMed] [Google Scholar]
- 4.Madiba TE, Thomson SR. The management of cecal volvulus. Dis Colon Rectum. 2002;45:264–7. doi: 10.1007/s10350-004-6158-4. [DOI] [PubMed] [Google Scholar]
- 5.Tejler G, Jiborn H. Volvulus of the cecum. Report of 26 cases and review of the literature. Dis Colon Rectum. 1988;31:445–9. doi: 10.1007/BF02552614. [DOI] [PubMed] [Google Scholar]
- 6.Theuer C, Cheadle WG. Volvulus of the colon. Am Surg. 1991;57:145–50. [PubMed] [Google Scholar]
- 7.O'Mara CS, Wilson TH, Stonesifer GL, Cameron JL. Cecal volvulus: analysis of 50 patients with long-term follow-up. Ann Surg. 1979;189:724–31. doi: 10.1097/00000658-197906000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rosenblat JM, Rozenblit AM, Wolf EL, DuBrow RA, Den EI, Levsky JM. Findings of caecal volvulus at CT. Radiology. 2010;256:169–75. doi: 10.1148/radiol.10092112. [DOI] [PubMed] [Google Scholar]
- 9.Macari M, Spieler B, Babb J, Pachter HL. Can the location of the CT whirl sign assist in differentiating sigmoid from caecal volvulus? Clin Radiol. 2011;66:112–7. doi: 10.1016/j.crad.2010.09.010. [DOI] [PubMed] [Google Scholar]
- 10.Fisher JK. Computed tomographic diagnosis of volvulus in intestinal malrotation. Radiology. 1981;140:145–6. doi: 10.1148/radiology.140.1.7244217. [DOI] [PubMed] [Google Scholar]


