Abstract
Although hyperthermic intraperitoneal chemotherapy (HIPEC) has been extensively used to treat patients with peritoneal metastases (PM) from colorectal cancer (CRC), a standard protocol has not yet been established. The aim of this preliminary clinical study was to confirm in vitro the efficacy of mitomycin C combined with 5-fluorouracil (MMC-5FU) under hyperthermic conditions in CRC and investigate the pharmacokinetics and feasibility of HIPEC with MMC-5FU for patients at high risk of PM from CRC. To simulate HIPEC in vitro, we used the collagen gel droplet-embedded culture drug sensitivity test with the HCT166 colorectal cell line to assess the antitumor efficacy of MMC and 5FU as single-agent and combination treatments following incubation with HCT116 cells for 30 min at either 37 or 42°C. In addition, five patients at high risk of PM from CRC underwent surgical tumor resection followed by HIPEC with MMC-5FU. Our results demonstrated that the combined administration of MMC-5FU suppressed tumor cell proliferation more efficiently compared to either agent used alone. In addition, hyperthermia at 42°C significantly enhanced drug sensitivity. During the clinical application of HIPEC with MMC-5FU, no grade 4 hematological toxicities or surgical adverse events were recorded. In addition, there was no evidence of peritoneal recurrence during a median observational period of 38 months. Of note, two patients with positive intraoperative peritoneal cytology at the first surgery developed no peritoneal recurrence and exhibited negative peritoneal cytology at the second surgery. In conclusion, HIPEC using MMC-5FU was shown to be a feasible therapeutic option, with an acceptable toxicity profile, for patients at high risk of PM from CRC. Therefore, HIPEC with MMC-5FU may be a promising novel therapeutic option for such patients, which merits further verification of its safety and efficacy in large-scale clinical trials.
Keywords: hyperthermic intraperitoneal chemotherapy, mitomycin C, 5-fluorouracil, combination, adjuvant
Introduction
Despite the recent advances in adjuvant therapy for colorectal cancer (CRC), the peritoneal surface remains an important failure site for patients with disease recurrence. Peritoneal carcinomatosis (PC) is commonly associated with a poor prognosis and a median survival of ∼6 months (1). However, the use of cytoreductive surgery with hyperthermic intraperitoneal chemotherapy (HIPEC) was reported to be a novel approach to treating peritoneal surface malignancies (2–6). Furthermore, as a positive peritoneal lavage following macroscopic curative surgery has been associated with decreased survival, increased recurrence and peritoneal metastases (PM) (7–9), HIPEC is considered to be a viable option for the treatment of patients at high risk of developing PM.
Mitomycin C (MMC) is the most frequently used agent for HIPEC and was shown to be efficient and safe for the treatment of PM of colorectal origin (10). In addition, 5-fluorouracil (5FU) was also shown to be effective as intraperitoneal chemotherapy and was used as early postoperative intraperitoneal chemotherapy (EPIC) following HIPEC in recent trials (11,12). However, the efficacy of 5FU in the HIPEC setting for patients with PM from CRC has not been determined. We recently evaluated the clinical potential of HIPEC with the combination of MMC and 5FU (MMC-5FU) in patients with PC due to gastric cancer (unpublished data). In the present study, we aimed to confirm the efficacy of HIPEC with MMC-5FU for CRC using in vitro simulation. Furthermore, we conducted a clinical study to investigate the feasibility and safety of HIPEC combining these two agents in patients at high risk of developing colorectal PM following cytoreductive surgery.
Materials and methods
In vitro simulation of HIPEC
HIPEC was simulated using a chemosensitivity test for antitumor agents, the collagen gel droplet-embedded culture drug sensitivity test, according to a modification of the manufacturer’s instructions (Kurabo Industries Ltd., Osaka, Japan) as previously described (13–15). Briefly, a suspension of the HCT116 CRC cell line (ATCC, Manassas, VA, USA) was added to a collagen solution to a final density of 1×105 cells/ml. Three drops (30 μl per drop) of the collagen-cell mixture were placed in each well of a 6-well plate on ice and allowed to gel at 37°C in a CO2 incubator. Each well was overlaid with PCM-2 medium (Kurabo Industries Ltd.) after 1 h and incubated overnight. The plates were then incubated with 5FU (final concentration, 200 μg/ml; 1,000 mg/5 l) and MMC (2 μg/ml; 10 mg/5 l) (Kyowa Hakko Kogyo Co., Tokyo, Japan), as single agents or in combination, in 4 ml of saline solution for 30 min at 37 or 42°C. Following removal of the saline solution containing the antitumor agents, each well was rinsed twice with 3 ml of Hank’s balanced salt solution (Nacalai Tesque, Inc., Kyoto, Japan), overlaid with 4 ml of PCM-2 medium and incubated for an additional 7 days. At the end of the incubation period, neutral red was added to each well to a final concentration of 50 μg/ml and the cancer cell colonies in the collagen gel droplets were stained for 2 h. Each collagen droplet was fixed with 10% neutral-buffered formalin, washed in water, air-dried and quantified by image analysis. The cytotoxicity (tumor reduction rate) was expressed as the T/C ratio percentage, in which T was the image optical density of the treated group and C was that of the control group.
Clinical evaluation
Subjects
This clinical study was performed at the Department of Surgery, Shiga University of Medical Science (Shiga, Japan). Patients who had received surgical intervention due to CRC between August, 2009 and December, 2012 were evaluated and five patients were found to be eligible and were enrolled in the study. The toxicities were graded in accordance with the Common Terminology Criteria for Adverse Events, version 4.0 (National Cancer Institute; http://evs.nci.nih.gov/ftp1/CTCAE/CTCAE_4.03_2010-06-14_QuickReference_8.5x11.pdf). The toxicities observed during the first 30 days after surgery, including hematological toxicity (anemia, neutropenia and thrombocytopenia), organ dysfunction (renal and hepatic dysfunction) and surgical complications, were recorded.
The inclusion criteria were as follows: i) patients at high risk of developing PM, defined as either the presence of PM from CRC, positive intraoperative peritoneal cytology, or stage cT4b CRC according to the 7th edition of the American Joint Committee on Cancer TNM staging system for CRC, or both; and ii) patients with PM considered to be resectable. The exclusion criteria were as follows: i) age <18 or >75 years; ii) World Health Organization performance status of >2; iii) cardiac dysfunction (New York Heart Association classification class >II or left ventricular ejection fraction <60%); iv) renal dysfunction (serum creatinine levels >1.5 mg/dl); v) hepatic dysfunction (total bilirubin levels >1.5 mg/dl); vi) leukopenia (white blood cell count <4,000/μl); vii) thrombocytopenia (platelet count <100,000/μl); viii) anemia (hemoglobin concentration <9.5 mg/dl); ix) history of severe disease, such as central nervous system disease, arrhythmia, myocardial infarction within 6 months or uncontrolled diabetes); x) unresectable distant metastases; and xi) pregnancy.
This study was conducted in accordance with the Helsinki Declaration and was approved by the Ethics Committee of the Shiga University of Medical Science. Informed consent was obtained from all the patients or their family members prior to HIPEC.
Surgical procedure
All the patients underwent resection of the primary lesions, recurrent lesions and PM (as appropriate) with open-abdomen HIPEC under general anesthesia. Following complete adhesiolysis, the diagnosis of PM was confirmed by frozen section biopsy when possible and the extent of PM was scored according to the Sugarbaker peritoneal cancer index (16). Macroscopically detectable disease was completely resected prior to HIPEC.
The HIPEC protocol was performed according to our experience using an open sterile circuit. Briefly, the laparotomy incision was closed, maintaining an 18-cm opening. An Arexis Wound Retractor (Applied Medical Resource, Rancho Santa Margarita, CA, USA) and plastic cylinder were used to create a water bath space for HIPEC (Fig. 1A). Outflow and inflow drain tubes were inserted in the rectouterine or rectovesical pouch and in the plastic cylinder bath space, respectively. Temperature probes were inserted into the abdominal cavity behind the mesentery. A perfusate of 5 l saline solution (Otsuka Pharmaceutical Factory, Inc., Tokushima, Japan) was circulated at a flow rate of 500–750 ml/min using a CP-3000 system (Tonokura Ika Kogyo Co. Ltd., Tokyo, Japan) (Fig. 1B). Once the temperature of the perfusate reached 42–43°C, 10 mg MMC and 1,000 mg 5FU were added. HIPEC was performed for 30 min after the addition of the antitumor agents. The intra-abdominal perfusate and blood samples were obtained to measure the concentrations of MMC and 5FU during and after HIPEC.
Figure 1.
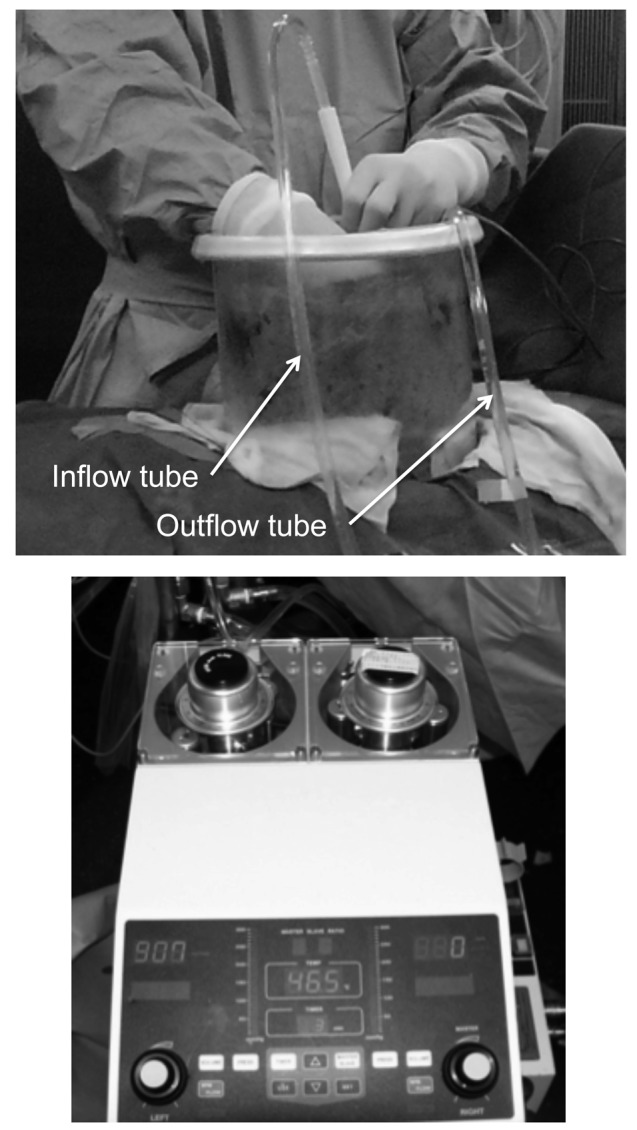
Overview of the set-up and the CP-3000 artificial heart-lung machine used for hyperthermic intraperitoneal chemotherapy.
Measurement of agent concentrations in the perfusate and plasma
The concentrations of MMC and 5FU in the plasma and peritoneal perfusate were determined using high-performance liquid chromatography on an LC-6A system (Shimadzu Corp., Kyoto, Japan) as previously described (17).
Follow-up after surgery and HIPEC
Following surgery, all the patients were transferred to a general surgical ward for postoperative management. The patients underwent blood sampling (complete blood count, renal function tests, electrolyte levels and liver function tests) following surgery. Radiological imaging was performed on the basis of clinical and biochemical parameters when postoperative complications were suspected. All the toxicities and postoperative complications that occurred during the first 30 days after surgery and HIPEC were recorded. The patients were monitored every 3 months in an outpatient clinic, where a physical examination was performed and tumor markers were assessed. Chest and abdominopelvic computed tomographic scans were performed every 6 months. The patients received systemic chemotherapy according to their recurrent conditions.
Statistical analysis
The values were compared using the Wilcoxon and Kruskal-Wallis rank order tests. P<0.05 was considered to indicate a statistically significant difference.
Results
In vitro simulation of HIPEC
The combination treatment with 5FU and MMC at 37°C exerted a significant suppressive effect on HCT116 cell proliferation compared to the untreated control cells (P<0.0001). Additionally, the combined use of MMC-5FU at 37 and 42°C suppressed tumor cell proliferation more effectively compared to either agent used alone at 37 and 42°C. Compared to normothermia (37°C), hyperthermia at 42°C significantly enhanced the sensitivity of the tumor cells to these antitumor agents, regardless of whether the drugs were used as single agents or in combination (P<0.0001). Overall, MMC-5FU at 42°C exhibited the highest cytotoxic activity (91.0% cytotoxity) against HCT116 cells in vitro (Fig. 2).
Figure 2.
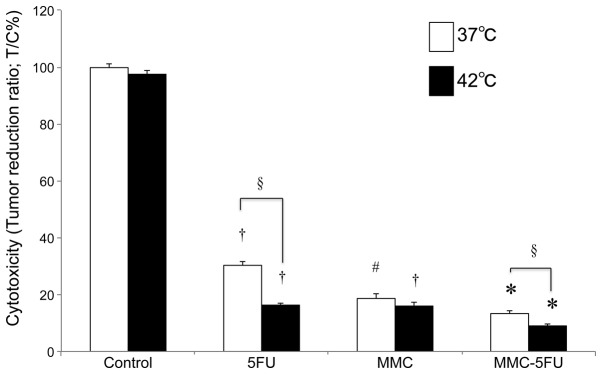
Cytotoxicity and hyperthermia-induced enhancement of antitumor drug toxicity on HCT116 cells. Cytotoxicity was expressed as the tumor reduction ratio (T/C ratio; %), in which T is the total volume of surviving cancer cells in the treated group and C is the total volume of surviving cancer cells in the control group. The P-values (<0.05 calculated by the Wilcoxon and Kruskal-Wallis rank order tests) indicated significant differences: †, compared to that of the control at the same temperature; #, compared to that of the control and 5FU at the same temperature; *, compared to those of all other groups at the same temperature; and §, compared to the corresponding group at 37°C. 5FU, 5-fluorouracil; MMC, mitomycin C.
Clinical evaluation
Patient characteristics
The characteristics of the five patients at a high risk of developing colorectal PM who underwent surgical intervention at our institution are shown in Table I. The study sample comprised three men and two women (median age, 61 years; range, 47–72 years). Patients 1 and 2 had developed peritoneal recurrence of CRC at 12 and 19 months following resection of their primary tumors, respectively. Three patients had primary CRC. In patient 3, the primary tumor had invaded the uterus and urinary bladder; PM was suspected during surgery but could not be pathologically confirmed. Patient 4 had positive intraoperative peritoneal cytology and in the patient 5 PMs were detected in the Douglas pouch during surgery (Table I).
Table I.
Patient characteristics and observations during and after surgery and hyperthermic intraperitoneal chemotherapy (HIPEC).
| Variables | Patients | ||||
|---|---|---|---|---|---|
|
| |||||
| 1 | 2 | 3 | 4 | 5 | |
| Age (years) | 69 | 60 | 73 | 60 | 47 |
| Gender | Male | Male | Female | Male | Female |
| Performance statusa | 0 | 1 | 0 | 0 | 0 |
| Clinical stageb | Peritoneal recurrence (12 months after 1st surgery) | Peritoneal recurrence (19 months after 1st surgery) | T4aN1aM0 Stage IIIB |
T4aN0M0 Stage IIB |
T3N2bM1b Stage IVB |
| Histology (adenocarcinoma) | Moderately differentiated | Moderately differentiated | Moderately differentiated | Well-differentiated | Moderately differentiated |
| Invasion of other organs | Rectum | Duodenum, right kidney, small intestine | Uterus, bladder | None | None |
| PM | Present | Present | Suspected | Absent | Present |
| Peritoneal cancer index | 2 | 2 | 0 | 0 | 1 |
| Intraoperative cytology | Positive | Negative | Negative | Positive | Positive |
| Complications | Ileus (grade 3), parotitis | Superficial surgical site infection (grade 3) | None | None | None |
| Toxicity | Increased alanine aminotransferase (grade 1) | Increased total bilirubin and creatinine, decreased hemoglobin (grade 1) | Decreased hemoglobin (grade 1) | None | None |
| Hospital stay (days) | 22 | 11 | 15 | 17 | 9 |
| Observation (months) | 44 | 40 | 38 | 35 | 16 |
| Recurrence after HIPEC | Lung, liver (13 months) | Lung (7 months) | None | Liver (14 months) | Liver (3 months) Ovary (12 months) |
| Treatment after HIPEC | Chemotherapy | Chemotherapy | None | Hepatectomy | Chemotherapy; surgery for ovarian metastasis |
| Second observation after HIPEC | None | None | None | No evidence of PM; cytology (−) | No evidence of PM; cytology (−) |
ECOG, Eastern Cooperative Oncology Group. PM, peritoneal metastases.
Classified according to the UICC TNM classification, version 7.
Toxicity following HIPEC
One patient developed grade 3 post-surgical ileus (Table I) and received conservative treatment with long-tube drainage for 3 days; this patient also developed parotitis. A single case of superficial grade 3 surgical site infection was recorded in patient 2. Two patients experienced a grade 1 decrease in the levels of hemoglobin and three patients experienced a grade 1 increase in alanine aminotransferase, total bilirubin and creatinine levels (Table I).
MMC and 5FU concentrations in the perfusate and plasma
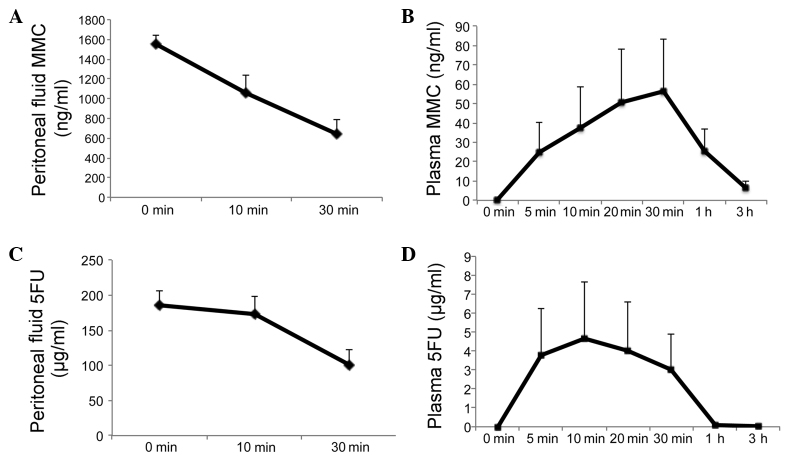
The area under the concentration-time curve (AUC) of MMC was 563±78.2 ng•h/ml in the perfusate (Fig. 3A) and 71.9±35.2 ng•h/ml in the plasma (Fig. 3B). The peak concentration of plasma MMC was 56.2±27.4 ng/ml 30 min after the initiation of HIPEC.
Figure 3.
Pharmacokinetics of MMC and 5FU in the peritoneal perfusate and plasma. Concentrations of (A) MMC and (C) 5FU in the 42°C peritoneal perfusate. MMC dose, 10 mg/5 l saline solution; 5FU dose, 1,000 mg/5 l saline solution. Pharmacokinetics of (B) MMC and (D) 5FU in the plasma during and after HIPEC. MMC, mitomycin C; 5FU, 5-fluorouracil; HIPEC, hyperthermic intraperitoneal chemotherapy.
The AUC of 5FU was 82.4±9.9 μg•h/ml in the perfusate (Fig. 3C) and 2.8±1.6 μg•h/ml in the plasma (Fig. 3D). The peak concentration of plasma 5FU was 4.7±2.9 μg/ml 10 min after the initiation of HIPEC.
Regarding the pharmacokinetics of intraperitoneal MMC-5FU, the peritoneal exposure to MMC was 7.8-fold higher and to 5FU 29.4-fold higher compared to that measured in the plasma. The plasma MMC and 5FU levels were ∼0 at 3 and 1 h after the initiation of HIPEC, respectively (Fig. 3).
Patient outcomes
No patients were lost during the median observational period of 38 months (range, 16–44 months). Three of the five patients developed pulmonary and/or hepatic metastases. Two patients (patients 1 and 2) received systemic chemotherapy alone. Patient 4 underwent hepatectomy for hepatic metastasis 14 months after HIPEC and patient 5 received systemic chemotherapy for hepatic metastasis and underwent surgical resection for ovarian metastasis 12 months after HIPEC. The two patients who underwent a second surgery exhibited no evidence of positive cytology or recurrent masses suggestive of PM. In addition, none of the five patients exhibited clinical signs of PM during the follow-up period (Table I).
Discussion
In our in vitro simulation of HIPEC, MMC-5FU exhibited at least 91.0% cytotoxicity against HCT116 cells. The combination of MMC-5FU was found to be superior to treatment with either agent alone regarding antitumor efficacy. In addition, although the follow-up period was brief, our results suggested that HIPEC with MMC-5FU is a safe and feasible therapeutic option for patients at high risk of PM from CRC.
MMC is the most frequent component of chemotherapeutic regimens administered during HIPEC for patients with PC of colorectal origin in single-center phase II studies, where MMC was administered as a single agent or in combination with other drugs, at doses ranging from 2.5 to 120 mg/m2 (12). In this study, we set the maximal dose of MMC at 10 mg/5 l in the perfusate, according to the maximal intraperitoneal dose (10 mg overall) permitted by the National Health Insurance guidelines in Japan.
5FU has been extensively used in perioperative cancer chemotherapy for colorectal PC. Its marked activity in the prevention of adhesion formation following major surgery (18) merits further investigation. In an initial study by Sugarbaker and Jablonski (19), 5FU was administered as intraperitoneal chemotherapy during surgery; however, chemotherapeutic agents that are enhanced by heat and are non-cell cycle-specific are pharmacologically preferable for HIPEC (20). 5FU, a thymidylate synthase inhibitor, binds covalently to this enzyme and prevents the formation of the DNA nucleoside precursor thymidine monophosphate (21). Therefore, 5FU is currently used in EPIC. Furthermore, 5-fluorouridine diphosphate and 5-fluorouridine triphosphate, which are metabolites of 5FU, exert cytotoxic effects via their incorporation into the RNA. In the present study, a tumor-suppressive effect was observed after a brief incubation of a large dose of 5FU with the HCT116 cells, which may reflect its cytotoxic effects due to incorporation into the RNA.
5FU has been considered to be chemically incompatible with other drugs in solutions for infusion or instillation. Our study demonstrated that the combination of MMC and 5FU exerted a 91.0% cytotoxic effect on HCT116 cells at 42°C in an in vitro simulation of HIPEC, and this effect was more prominent compared to that of 5FU as a single agent at 42°C. Therefore, 5FU also retains its antitumor activity in the MMC-5FU mixture. We set the maximal dose of 5FU to 1,000 mg/5 l in the perfusate, according to the maximal intravenous bolus dose (10–20 mg/kg) permitted by the National Health Insurance guidelines in Japan.
Various researchers reported the efficacy of adjuvant HIPEC in the clinical setting in patients at high risk of developing PC. Although the size of the patient sample was limited, several randomized studies suggested that adjuvant HIPEC may significantly improve survival and reduce the incidence rate of PC in patients with gastric cancer and CRC (22–25). A positive peritoneal lavage following macroscopic curative surgery in patients with CRC appears to be associated with decreased survival and increased recurrence of PM (7–9) and HIPEC appears to be a suitable treatment for patients at high risk of PM. Thus, in our preliminary clinical study, we enrolled patients in whom complete resection of macroscopic disease was achieved prior to HIPEC.
We acknowledge that there were several limitations to the present study. Our results demonstrated that the combination treatment with MMC-5FU was effective in an in vitro simulation of HIPEC; however, the suppressive effects of this combination in vivo have yet to be fully determined. In addition, the dosage of antitumor agents, the perfusion technique and the duration of the perfusion differ among different centers that perform HIPEC. Additional studies are required to establish the efficacy of HIPEC with MMC-5FU.
In conclusion, this study demonstrated that HIPEC with MMC-5FU is feasible, safe and may prevent PM from CRC in patients at high risk of this complication. These findings suggest that HIPEC with MMC-5FU following cytoreductive surgery may be a promising novel therapeutic option for such patients, which merits further verification of its safety and efficacy in large-scale clinical trials.
Acknowledgments
This study was supported by a Grant-in-Aid for Scientific Research from the Japan Society for the Promotion of Science (grant number 24591973).
References
- 1.Stewart JH, IV, Shen P, Levine EA. Intraperitoneal hyperthermic chemotherapy for peritoneal surface malignancy: current status and future directions. Ann Surg Oncol. 2005;12:765–777. doi: 10.1245/ASO.2005.12.001. [DOI] [PubMed] [Google Scholar]
- 2.Chua TC, Esquivel J, Pelz JO, Morris DL. Summary of current therapeutic options for peritoneal metastases from colorectal cancer. J Surg Oncol. 2013;107:566–573. doi: 10.1002/jso.23189. [DOI] [PubMed] [Google Scholar]
- 3.Mohr Z, Hirche C, Liebeskind U, Rau B, Hunerbein M. Feasibility of delayed hyperthermic intraperitoneal chemotherapy in case of unforeseen complications. Eur Surg Res. 2011;47:19–25. doi: 10.1159/000327397. [DOI] [PubMed] [Google Scholar]
- 4.Yonemura Y, Elnemr A, Endou Y, et al. Multidisciplinary therapy for treatment of patients with peritoneal carcinomatosis from gastric cancer. World J Gastrointest Oncol. 2010;2:85–97. doi: 10.4251/wjgo.v2.i2.85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Imano M, Imamoto H, Itoh T, et al. Impact of intraperitoneal chemotherapy after gastrectomy with positive cytological findings in peritoneal washings. Eur Surg Res. 2011;47:254–259. doi: 10.1159/000333803. [DOI] [PubMed] [Google Scholar]
- 6.Fujishima Y, Goi T, Kimura Y, Hirono Y, Katayama K, Yamaguchi A. MUC2 protein expression status is useful in assessing the effects of hyperthermic intraperitoneal chemotherapy for peritoneal dissemination of colon cancer. Int J Oncol. 2012;40:960–964. doi: 10.3892/ijo.2012.1334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bosanquet DC, Harris DA, Evans MD, Beynon J. Systematic review and meta-analysis of intraoperative peritoneal lavage for colorectal cancer staging. Br J Surg. 2013;100:853–862. doi: 10.1002/bjs.9118. [DOI] [PubMed] [Google Scholar]
- 8.Mohan HM, O’Connor DB, O’Riordan JM, Winter DC. Prognostic significance of detection of microscopic peritoneal disease in colorectal cancer: a systematic review. Surg Oncol. 2013;22:e1–e6. doi: 10.1016/j.suronc.2013.01.001. [DOI] [PubMed] [Google Scholar]
- 9.Glockzin G, Rochon J, Arnold D, et al. A prospective multicenter phase II study evaluating multimodality treatment of patients with peritoneal carcinomatosis arising from appendiceal and colorectal cancer: the COMBATAC trial. BMC Cancer. 2013;13:67. doi: 10.1186/1471-2407-13-67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Koppe MJ, Boerman OC, Oyen WJ, Bleichrodt RP. Peritoneal carcinomatosis of colorectal origin: incidence and current treatment strategies. Ann Surg. 2006;243:212–222. doi: 10.1097/01.sla.0000197702.46394.16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Klaver YL, Hendriks T, Lomme RM, Rutten HJ, Bleichrodt RP, de Hingh IH. Intraoperative versus early postoperative intraperitoneal chemotherapy after cytoreduction for colorectal peritoneal carcinomatosis: an experimental study. Ann Surg Oncol. 2012;19(Suppl 3):S475–S482. doi: 10.1245/s10434-011-1984-9. [DOI] [PubMed] [Google Scholar]
- 12.Weber T, Roitman M, Link KH. Current status of cytoreductive surgery with hyperthermic intraperitoneal chemotherapy in patients with peritoneal carcinomatosis from colorectal cancer. Clin Colorectal Cancer. 2012;11:167–176. doi: 10.1016/j.clcc.2012.01.001. [DOI] [PubMed] [Google Scholar]
- 13.Kobayashi H, Tanisaka K, Doi O, et al. An in vitro chemosensitivity test for solid human tumors using collagen gel droplet embedded cultures. Int J Oncol. 1997;11:449–455. doi: 10.3892/ijo.11.3.449. [DOI] [PubMed] [Google Scholar]
- 14.Okumura K, Shiomi H, Mekata E, et al. Correlation between chemosensitivity and mRNA expression level of 5-fluorouracil-related metabolic enzymes during liver metastasis of colorectal cancer. Oncol Rep. 2006;15:875–882. [PubMed] [Google Scholar]
- 15.Muller M, Cherel M, Dupre PF, Gouard S, Collet M, Classe JM. The cytotoxic effect of combined hyperthermia and taxane chemotherapy on ovarian cancer cells: results of an in vitro study. Eur Surg Res. 2012;48:55–63. doi: 10.1159/000333393. [DOI] [PubMed] [Google Scholar]
- 16.Sugarbaker PH. Intraperitoneal chemotherapy and cytoreductive surgery for the prevention and treatment of peritoneal carcinomatosis and sarcomatosis. Semin Surg Oncol. 1998;14:254–261. doi: 10.1002/(sici)1098-2388(199804/05)14:3<254::aid-ssu10>3.0.co;2-u. [DOI] [PubMed] [Google Scholar]
- 17.Kuzuya T, Yamauchi M, Ito A, Hasegawa M, Hasegawa T, Nabeshima T. Pharmacokinetic characteristics of 5-fluorouracil and mitomycin C in intraperitoneal chemotherapy. J Pharm Pharmacol. 1994;46:685–689. doi: 10.1111/j.2042-7158.1994.tb03883.x. [DOI] [PubMed] [Google Scholar]
- 18.Pestieau SR, Marchettini P, Stuart OA, Chang D, Sugarbaker PH. Prevention of intraperitoneal adhesions by intraperitoneal lavage and intraperitoneal 5-fluorouracil: experimental studies. Int Surg. 2002;87:195–200. [PubMed] [Google Scholar]
- 19.Sugarbaker PH, Jablonski KA. Prognostic features of 51 colorectal and 130 appendiceal cancer patients with peritoneal carcinomatosis treated by cytoreductive surgery and intraperitoneal chemotherapy. Ann Surg. 1995;221:124–132. doi: 10.1097/00000658-199502000-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sugarbaker PH. Cytoreductive surgery plus hyperthermic perioperative chemotherapy for selected patients with peritoneal metastases from colorectal cancer: a new standard of care or an experimental approach? Gastroenterol Res Pract. 2012;2012:309417. doi: 10.1155/2012/309417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wyatt MD, Wilson DM., III Participation of DNA repair in the response to 5-fluorouracil. Cell Mol Life Sci. 2009;66:788–799. doi: 10.1007/s00018-008-8557-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.De Roover A, Detroz B, Detry O, et al. Adjuvant hyperthermic intraperitoneal peroperative chemotherapy (HIPEC) associated with curative surgery for locally advanced gastric carcinoma. An initial experience. Acta Chir Belg. 2006;106:297–301. doi: 10.1080/00015458.2006.11679896. [DOI] [PubMed] [Google Scholar]
- 23.Tentes AA, Spiliotis ID, Korakianitis OS, Vaxevanidou A, Kyziridis D. Adjuvant perioperative intraperitoneal chemotherapy in locally advanced colorectal carcinoma: preliminary results. ISRN Surg. 2011;2011:529876. doi: 10.5402/2011/529876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Raue W, Tsilimparis N, Bloch A, Menenakos C, Hartmann J. Volume therapy and cardiocircular function during hyperthermic intraperitoneal chemotherapy. Eur Surg Res. 2009;43:365–372. doi: 10.1159/000248164. [DOI] [PubMed] [Google Scholar]
- 25.Mizumoto A, Canbay E, Hirano M, et al. Morbidity and mortality outcomes of cytoreductive surgery and hyperthermic intraperitoneal chemotherapy at a single institution in Japan. Gastroenterol Res Pract. 2012;2012:836425. doi: 10.1155/2012/836425. [DOI] [PMC free article] [PubMed] [Google Scholar]