Abstract
This mixed-methods study examines the primary health care experiences of Hispanic patients with serious mental illness. Forty patients were recruited from an outpatient mental health clinic. Participants reported a combination of perceived discrimination and stigmatization when receiving medical care. They rated the quality of chronic illness care as poor and reported low levels of self-efficacy and patient activation. These indicators were positively associated with how patients viewed their relationships with primary care providers. A grounded model was developed to describe the structural, social, and interpersonal processes that shaped participants’ primary care experiences.
Keywords: Primary care, serious mental illness, mixed methods, Hispanics, patient-centered care
Common medical conditions like heart disease, diabetes mellitus, and cancer disproportionally impact people with serious mental illness (SMI; e.g., schizophrenia, bipolar disorder) and account for a significant portion of the elevated mortality rates observed in this population (Druss, Zhao, Von Esenwein, Morrato, & Marcus, 2011). Hispanics with SMI may face even greater risk for these health disparities compared to non-Hispanic Whites with SMI as studies have shown elevated rates of common medical conditions (e.g., obesity, diabetes, metabolic syndrome) in this growing minority population (Hellerstein et al., 2007; Kato, Currier, Gomez, Hall, & Gonzalez-Blanco, 2004; Lambert, Chou, Chang, Tafesse, & Carson, 2005; McEvoy et al., 2005). For example, a ten-year naturalistic study of patients with schizophrenia treated with clozapine found that Hispanic patients were at higher risk than White patients for developing diabetes and having a CVD-related death (Henderson et al., 2005). These health disparities justify the need to devote special attention to Hispanics with SMI in treatment planning, intervention development, and health services research in order to improve the health of this historically underserved community.
The receipt of suboptimal medical care is one important factor that can exacerbate the health needs of Hispanics with SMI. Yet the few studies that have examined the receipt and quality of medical care in Hispanics with SMI report mixed results with some finding low rates of treatment for chronic conditions associated with CVD (e.g., hypertension) while others report higher odds of receiving guideline-concordant care for CVD conditions (Druss et al., 2012; Nasrallah et al., 2006). To date, limited attention has been paid to examining the factors that shape the primary care experiences of Hispanics with SMI.
A variety of factors can impact the medical care that Hispanics with SMI receive in primary care settings. Structural barriers, such as lack or insufficient health insurance, long waits in clinics, language barriers, and lack of care coordination between mental health and primary care providers, can prevent Hispanic patients from accessing and receiving timely primary care. Provider-level issues, including biases, stigmatization, and lack of training and experience working with people with SMI, have been shown to negatively impact how primary care clinicians deliver medical care to people with SMI (Druss, 2007; Jones, Howard, & Thornicroft, 2008). Moreover, interpersonal aspects of care, such as the nature of the patient- provider relationship, can shape Hispanic patients’ primary care experiences. For example, cultural norms like personalismo (being warm and personable; showing that personal ties outweigh formal, institutional connections), respeto (respect), and dignidad (dignity), valued by Hispanics in interpersonal relationships are critical for engaging Hispanic patients into care (Cabassa, Hansen, Palinkas, & Ell, 2008; Interian, Martinez, Rios, Krejci, & Guarnaccia, 2010). The type of relationship that patients form with their primary care clinicians (e.g., positive vs. negative) can also influence how patients view the quality of the care they receive, their satisfaction with services, and their involvement and participation in health care (Becker & Roblin, 2008).
In this study, we examined the factors that shape the primary care experiences of Hispanics with SMI. We defined these experiences as patients’ perceptions of their primary health care and their views about receiving medical care from primary care providers. These perceptions encompass patients’ experiences while accessing and navigating the primary care system and their relationships with medical providers. Examining patients’ perceptions of their primary care is critical for understanding and developing patient-centered care, a key standard of care stipulated by the Institute of Medicine (2001) that is essential for improving health care quality and reducing health care disparities among racial and ethnic minority groups and people with mental and substance-use conditions (Institute of Medicine, 2003, 2006). Patient-centered care is defined as health care that is “respectful and responsive to individual patient preferences, needs and values and ensuring that patient values guide all clinical decisions” (Institute of Medicine, 2001, p. 40). Studying patients’ personal accounts of their medical care is essential for understanding patient-centered care as it generates valuable insights into what patients’ value and prefer during the medical encounter, identifies facilitating or impeding factors in their navigation of the system, detects how they view their relationships with providers, and how they perceive the quality of health care.
Methods
Study Overview
We used a mix of quantitative and qualitative methods to examine the primary health care experiences of Hispanic outpatients with SMI. Patient focus groups were embedded within a larger quantitative study using structured patient interviews and medical chart abstractions. We merged both sources of data to describe patients’ perceived stigma and discrimination in receiving medical care and to explore how patients’ discussions of their relationships with their primary care providers were associated with quantitative indicators of patient-centered care, including patients’ perceptions of the quality of chronic illness care, levels of self-efficacy, and patient activation. We then used qualitative data to deepen our understanding of these associations by developing a grounded model of participants’ primary health care experiences that captures the structural, social, and interpersonal processes that shape their experiences with medical care. Study procedures were approved by the appropriate institutional review boards at (BLIND INSTITUTION and BLIND INSTITUTION).
Sample
This study was conducted between October 2011 and February 2012 at an outpatient public mental health clinic in New York City that serves a large population of Hispanics with SMI, mostly of Dominican origins. A purposive sampling strategy was used. Eligible participants needed to be active patients at the clinic, 18 years of age or older, and self-identified as Hispanic who spoke English or Spanish. They also needed to have a chart diagnoses of a serious mental illness defined - as a mental disorder that meets DSM-IV diagnostic criteria (e.g., schizophrenia, bipolar disorder) associated with substantial functional impairment that interferes with major life activities (e.g., employment, social relationships) - and at least one CVD risk factor (body mass index [BMI] ≥ 25, diabetes mellitus, current smoker, hypertension, or hyperlipidemia). We excluded patients in need of detoxification and/or at acute risk of suicidal/homicidal behavior at the time of recruitment and those who failed a capacity-to-consent questionnaire (Zayas, Cabassa, & Pérez, 2005) or were cognitively impaired, as detected by the Mini-Cog Examination (Palmer & Meldon, 2003).
Potential participants were referred to the study by their mental health clinician. Fifty-three patients were referred and screened. Eleven refused to participate (e.g., not interested), and two failed the capacity-to-consent questionnaire.
Data Collection
We used two quantitative data sources (structured patient interviews and medical chart abstractions) and one qualitative approach (patient focus groups). All data were collected by trained bilingual study staff.
Structured Interviews
These interviews lasted approximately 90 minutes and were administered in the patient’s preferred language (English or Spanish). We collected information about patients’ demographic characteristics, place of birth, years living in the U.S., language preferences, and self-reported medical conditions.
We also included the following measures. Perceived discrimination and stigma were measured with 3 items adapted from a national telephone survey conducted by the Kaiser Family Foundation (Lillie-Blanton, Brodie, Rowland, Altman, & McIntosh, 2000). The first item asked participants if they “thought racism (defined as being treated unfairly due to a person’s race/ethnicity) was a problem in the U. S. health care system” on a 3-point scale ranging from 0 (not a problem) to 2 (a major problem). The second question asked how often participants “thought that the health care system treated persons unfairly” because of four different characteristics: being Hispanic, not being able to speak English very well, being a person with a mental illness, and being an immigrant. This is a set of global opinion questions that examined participants’ general views of how people with different social characteristics are treated overall in the U. S. health care system. For each characteristic a 4-point scale ranging from 0 (never) to 3 (very often) was used. The last question asked participants if they had “ever felt disrespected by a doctor or health care provider” because of: being Hispanic, being a person with a mental illness, and being a person who spoke Spanish. A dichotomous scale of 0 (no) and 1 (yes) was used for each characteristic.
The Patient Assessment of Chronic Illness Care (PACIC) scale assesses patients’ perspectives on the quality and patient-centeredness of chronic illness care received during the past 6 months (Glasgow, Whitesides, Nelson, & King, 2005). The instrument has 20 items divided into five subscales that correspond to dimensions of the chronic care model: patient activation, delivery system design/decision support, goal setting, problem solving, and care coordination. Each item is scored on a 5-point scale ranging from 1 (almost never) to 5 (almost always). The PACIC has strong psychometric properties and has been validated in English and Spanish and with clinical populations with and without mental disorders (Aragones et al., 2008; Gensichen et al., 2011; Glasgow et al., 2005). We present the mean overall PACIC and subscale scores; higher scores indicate more positive assessments of chronic illness care. The overall PACIC scale in our sample had excellent internal consistency (Cronbach’s α = 0.95) and with subscales coefficient alphas of .76 to .85.
To measure patients’ self-efficacy, we used a 5-item subscale derived from Lorig’s (1996) Chronic Disease Self-Efficacy (CDSE) scale: This subscale tap patients’ confidence regarding genral self-management behaviors on a scale from 0 (not at all confident) to 10 (totally confident). It has established internal consistency and test-retest reliability, has been used in numerous self-management studies, and is available and validated in English and Spanish (K. Lorig et al., 1996). We report mean subscale score, ranging from 0 to 10, with higher scores representing greater self-efficacy. This scale had excellent internal consistency (α = 0.91) in our sample.
Lastly, the patient activation measure (PAM) is a 13-item scale that assesses patients’ knowledge, skills, and confidence related to self-management (Hibbard, Mahoney, Stockard, & Tusler, 2005). It has strong psychometric properties, has been tested across a range of chronic illnesses, and is available in English and Spanish (Hibbard et al., 2005; Hibbard & Tusler, 2007; Skolasky, Mackenzie, Wegener, & Riley, 2008). PAM scores range from 0 (no activation) to 100 (high activation) and had good internal consistency (α= 0.86) in our sample.
Chart Abstractions
These abstractions were conducted by a research assistant supervised by the first author. As part of the informed consent process, all participants provided written permission for research staff to access their medical records at the study site, including medical and psychiatric information. The following clinical data were collected from patients’ records at the outpatient psychiatric clinic: primary mental health diagnosis, physical health conditions, type of psychiatric medications, and smoking status.
Patient Focus Groups
Five focus groups were conducted at the study site in Spanish, each lasting 90 minutes, and each consisting of 3–9 patients. All groups were audiotaped and professionally transcribed verbatim. We used a focus group guide composed of open-ended questions and probes derived from our review of the literature to elicit patients’ views about their primary health care experiences (focus group guide available upon request). Examples of questions and probes included: How do you get along with your primary care doctor? What do you like about your primary care doctor? What do you dislike about your primary care doctor? What difficulties do you face when you go see your primary care doctor or receive medical care for your health problems? Focus groups were chosen over in-depth qualitative interviews because of funding limitations.
We also transformed each patients’ comments during the focus groups into a dichotomous variable composed of two mutually exclusive categories: positive or negative relationship with their primary care provider. The first two authors independently read each transcript and applied this code to the focus group data. We were in agreement on 20 of the 24 participants (83%). For the remaining four participants, we reviewed our differences using examples from the transcripts and came to a consensus.
Data Analysis
Frequencies and measures of central tendencies were used to describe the sample and present quantitative results. We used independent sample t-tests to explore the associations between patients’ relationships with their primary care providers (positive or negative) and their assessment of chronic illness care, self-efficacy, and patient activation. Given our small sample size, we also explored the significance of these associations using the Mann Whitney U-tests, a nonparametric test that is equivalent to a t-test.
Our qualitative analysis helped deepen our understanding of the quantitative findings. We used open-coding procedures and the constant comparative method derived from grounded theory (Strauss & Corbin, 1998) to analyze focus group transcripts. The first two authors independently read all transcripts and drafted analytical memos to develop an initial code list. We then met on a weekly basis for several months to present and discuss our respective codes, interpretation of the data, and analytical questions. Our decisions during these analytical meetings and our meeting notes were used to reach consensus on the codes that were ultimately included in our code book.
All qualitative data were entered into Atlas.ti (Muhr, 2004) which was used to facilitate the management and application of our code book to the transcripts. One coder (BLIND) then coded all qualitative data under the supervision of the primary author (BLIND). We used the constant comparative method to cluster codes into categories, derive themes, and develop our grounded model of health care experiences (Strauss & Corbin, 1998). This process involved generating queries and reports in Atlas.ti on major codes. Through our review and discussions of these reports, we identified discernible patterns in our data, and developed analytical memos describing the emergence of categories and subcategories. We grouped our major categories into overarching themes taking into consideration how salient these themes were across focus groups and the emotional intensity conveyed by participants in their narratives and discussions of these topics (Frosch, May, Rendle, Tietbohl, & Elwyn, 2012). We used the following strategies to ensure the trustworthiness of our analysis: generation of an audit trail to document analytical decisions, triangulation of quantitative and qualitative data, and member-checking presentations to the clinic’s staff, the project’s community advisory board, and professional meetings (Padgett, 1998).
Integration of Quantitative and Qualitative Findings
We triangulated the overarching qualitative themes related to participants’ primary health care experiences and the lessons learned from our quantitative analysis to develop a grounded model that describes the structural, social, and interpersonal characteristics of participants’ experiences with primary care. This model deepens and enriches the understanding of participants’ primary care experiences by illustrating the context and social forces that shaped these experiences. Use of this triangulation strategy during the data analysis and interpretation phase is a common approach in mixed-methods studies for integrating quantitative and qualitative data in order to confirm and enrich findings within a single study (Creswell, 2003).
Results
Sample Characteristics
A total of 40 Hispanic outpatients participated in the study. All were invited to participate in focus group discussions. Twenty-four participated in five focus groups. Characteristics of the total sample and the focus group sub-sample are presented in Table 1. There were no statistically significant differences on key demographic characteristics (e.g., age, gender; results available upon request) between patients who only participated in the structured interviews and those who participated in both the structured interviews and focus groups. Half of our total sample was female. On average, participants were fifty years of age, had less than a high school degree, were Dominican, and had lived in the U. S. for about thirty years. Most were Spanish speakers (55%) or bilingual (32.5%) and rated their physical health as fair or poor. The most common chronic medical conditions were: high cholesterol, hypertension, arthritis, and diabetes mellitus. On average, participants had 4 medical conditions. All but one patient had visited a primary care provider in the past 12 months. The most common psychiatric conditions included: schizophrenia, schizoaffective disorder, and major depression. Over half of participants were taking second-generation antipsychotic medications.
Table 1.
Sample Characteristics
| Sample Characteristics | Total Sample (N = 40) | Focus Group Sub-Sample (N=24) | ||||
|---|---|---|---|---|---|---|
|
| ||||||
| Mean (SD) | N | % | Mean (SD) | N | % | |
| Age | 50.6 (13.7) | 52.9 (13.2) | ||||
| Years of Education | 10.7 (4.3) | 11.9 (3.8) | ||||
| Female | 20 | 50 | 14 | 58.3 | ||
| Marital Status | ||||||
| Married | 6 | 15 | 3 | 12.5 | ||
| Single | 22 | 55 | 12 | 50 | ||
| Widow/Divorced/Separated | 12 | 30 | 9 | 37.5 | ||
| Place of Birth | ||||||
| U. S. Mainland | 6 | 15 | 2 | 8.3 | ||
| Dominican Republic | 28 | 70 | 17 | 70.8 | ||
| Puerto Rico | 4 | 10 | 3 | 12.5 | ||
| Other (i.e., Cuba, Costa Rica) | 2 | 5 | 2 | 8.3 | ||
| Years living in the U.S. | 30.6 (13.2) | 33.8 (14.5)** | ||||
| Language Preference | ||||||
| Spanish Only | 22 | 55 | 13 | 54.2 | ||
| Bilingual | 13 | 32.5 | 11 | 45.8 | ||
| English Only | 5 | 12.5 | 0 | 0 | ||
| Perceived Health Status | ||||||
| Fair/Poor | 26 | 65 | 17 | 73.9** | ||
| Chart-reported Common Medical Conditions | ||||||
| Asthma | 6 | 15 | 3 | 12.5 | ||
| Arthritis | 17 | 42.5 | 10 | 41.7 | ||
| Diabetes | 16 | 40 | 9 | 37.5 | ||
| Hypertension | 24 | 60 | 14 | 58.3 | ||
| High Cholesterol | 27 | 67.5 | 17 | 70.8 | ||
| Average Number of Medical Conditions | 4.2 (2.3) | 4.5 (2.3)** | ||||
| Current Smokers | 16 | 40 | 7 | 30.4** | ||
| Visited Primary Care | 39 | 97.5 | 23 | 95.8 | ||
| Provider in Past 12-months Chart Diagnosis | ||||||
| Schizophrenia | 13 | 32.5 | 5 | 20.8 | ||
| Schizoaffective Disorder | 11 | 27.5 | 9 | 37.5 | ||
| Major Depression | 8 | 20 | 3 | 12.5 | ||
| Bipolar Disorder | 7 | 17.5 | 6 | 25 | ||
| Taking Second Generation Antipsychotics** | 27 | 69.2* | 14 | 63.6*** | ||
Note:
n = 39;
n = 23;
n = 22
Perceived Discrimination and Stigma
We found elevated rates of perceived discrimination and stigma in our sample (see Table 2). Three-quarters of participants reported that racism was a problem or major problem in the U.S. health care system. Participants also reported that people are treated unjustly in the U.S. health care system somewhat to very often because of being: Hispanic (60%), Black (65%), immigrants (83%), people who do not speak English very well (68%), and who have a serious mental illness (66%). Moreover, when asked whether they had ever felt disrespected by a medical provider, 18% attributed this event to being Hispanic, 33% to having a serious mental illness, and 20% to speaking Spanish.
Table 2.
Perceived Discrimination and Stigma (N = 40)
| Discrimination and Stigma Indicators | N | % |
|---|---|---|
| Is racism a problem in the healthcare system?* (Yes) | 30 | 75 |
| How often are people treated unjustly in healthcare systems for being:** | ||
| Hispanic | 24 | 60 |
| Black | 26 | 65 |
| An immigrant | 33 | 82.5 |
| A person who does not speak English well | 27 | 67.5 |
| A person with serious mental illness | 26 | 65 |
| Ever felt a doctor treated you with disrespect because: (Yes) | ||
| You are Hispanic | 7 | 17.5 |
| You have a serious mental illness | 13 | 32.5 |
| You speaks Spanish | 8 | 20 |
Note:
“Problem” and “Major Problem”;
“Somewhat Often” and “Very Often”
Indicators of Patient-Centered Care and Associations with Patients’ Relationships with Primary Care Providers
Descriptive statistics for the indicators of patient-centered care and of participants’ relationship with their primary care providers are presented in Table 3. Participants’ ratings of the quality of chronic illness care were low. All means fell between receiving assistance in these dimensions “a little of the time” to “some of the time” over the past 6 months. A closer examination of the distribution of scales results shows that most participants received little to no assistance with patient activation (57.5%), goal setting (70%), problem solving (65.5%), and care coordination (60%).
Table 3.
Indicators of Patient-Centered Care and their Associations with Patient-Primary Care Clinician Relationship
| Indicators of Patient-Centered Care | Total Sample (N=40) | Patients’ Relationships with Primary Care Clinicians (N = 23a)
|
t-value (df) | Mann-Whitney U Test (Sig) | ||||
|---|---|---|---|---|---|---|---|---|
| Positive Relationship (n = 11) | Negative Relationship (n = 12) | |||||||
| Mean | SD | Mean | SD | Mean | SD | |||
| Total PACIC Scores (α = .95) | 2.50 | 1.04 | 3.27 | 0.65 | 2.11 | 0.97 | −3.34 (21)* | .006 |
| PACIC: Patient Activation (α = .79) | 2.48 | 1.26 | 3.30 | 0.81 | 2.44 | 1.39 | −1.79 (20) | .151 |
| PACIC: Delivery System/Practice Design (α = .76) | 2.88 | 1.41 | 3.72 | 0.70 | 2.36 | 1.24 | −3.29 (17.56) ** | 0.007 |
| PACIC: Goal Setting (α = .84) | 2.24 | 1.10 | 2.92 | 0.97 | 1.77 | 0.96 | −2.88 (21)** | 0.013 |
| PACIC: Problem Solving (α = .85) | 2.54 | 1.23 | 3.32 | 1.00 | 2.02 | 0.98 | −3.13 (21)** | 0.006 |
| PACIC: Care Coordination (α = .84) | 2.55 | 1.04 | 3.27 | 0.93 | 2.17 | 0.98 | −2.78 (21)** | 0.009 |
| Self-Management Indicators | ||||||||
| Self-efficacy: Managing Chronic Disease (α = .91) | 5.90 | 2.29 | 6.87 | 2.02 | 4.58 | 1.77 | −2.89 (21)** | 0.009 |
| Patient Activation Measure (α =.86) | 55.28 | 18.03 | 59.8 | 13.08 | 46.48 | 11.44 | −2.60 (21)* | 0.023 |
p ≤ 0.05,
p ≤ 0.01
Note:
One participant in the focus group had missing data on these patient-centered care indicators and was excluded from these analyses. α = Cronbach’s coefficient alpha. PACIC: Patient Assessment of Chronic Illness Care. PACIC total and subscale ranges from 1 (never) to 5 (always), higher scores indicate greater assessment of chronic illness care. Self-efficacy scales range from 0 to 10, higher scores greater levels of self-efficacy. Patient Activation measure range from 0 to 100, higher score greater patient activation.
Participants’ also reported low self-efficacy and patient activation scores. On average, their self-efficacy for managing chronic disease was in the moderate range (m = 5.90, sd = 2.29). Within the four patient activation levels captured by the PAM, ranging from being passive to adopting self-managing behaviors, participants reported a mean level of 3. That is, participants were beginning to take self-management actions but lacked confidence about their attempts. A closer examination of the distribution of PAM scores indicates that over three quarters of participants (77.5%) scored between level 1 (passive and not confident) and level 3.
We also found several associations between indicators of patient-centered care and patients’ relationships with their primary care providers (See Table 3). Based on our coding of patients’ focus groups, positive relationships (N = 11) were characterized as warm, friendly, and trustworthy, while negative relationships (N = 12) were characterized as impersonal, detached, rushed, and disrespectful. Compared to patients who had negative relationships with their primary care providers, patients with positive relationships reported significantly better overall assessment of their chronic illness care; in particular, better ratings about the delivery system/practice design and more assistance with goal setting, problem solving, and care coordination. Patients with positive relationships also reported significantly higher activation and self-efficacy for managing their chronic disease.
Grounded Model of Primary Health Care Experiences
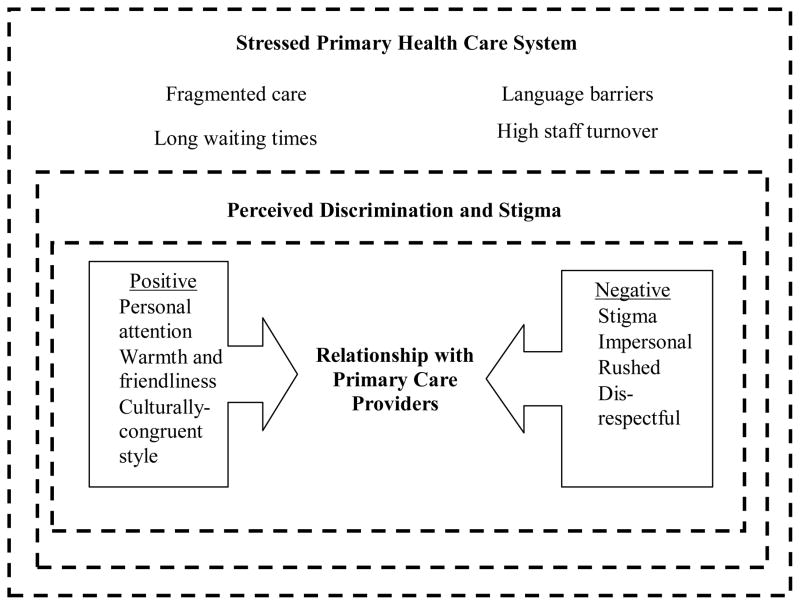
A grounded model of primary health care experiences emerged from the triangulation of our data (see Figure 1). The model expands upon our quantitative results and depicts how participants’ primary health care experiences are embedded within a stressed health care system characterized by numerous structural barriers and high levels of perceived discrimination and stigma associated with being Hispanic and having a serious mental illness. We also found that these characteristics of the health care system seem to be buffered by the nature of participants’ relationships with their primary care providers (positive vs. negative).
Figure 1.
Grounded Model of Primary Health Care Experiences
Stressed Health Care System
In all focus groups, participants consistently talked about having to navigate a stressed health care system in order to access and use primary care services. Participants were seen in 18 different primary care clinics ranging from small private offices to large public primary care centers. Regardless of where participants received medical services, they consistently described these primary care clinics as full, overflowing with patients, and with a staff that seemed overburdened and rushed, as exemplified by Pedro’s comment (all names are pseudonyms and all quotes have been translated from Spanish): “in the clinic that I go to there are too many people. The doctor is full to capacity and you can’t talk much with him.” The most common frustration expressed by participants was their inability to get timely appointments; some had to wait 3–4 months to be seen. Others described how they could not get walk-in appointments and were often turned away. These situations pushed many to rely on the emergency room for care and eroded their confidence and trust in the health care system. For instance, Enrique described how the last time he had the flu he tried to get a walk-in appointment; when he got to the clinic, the receptionist told him:
‘The doctor can’t see you … He has too many patients. You have to call for an appointment.’ “That made me feel bad. I went home and I took some home remedies until the flu went away. After that experience, I did not want to go back to that doctor.”
Other common structural barriers included: facing language barriers when scheduling appointments, spending hours waiting to be seen by the doctor, and not being able to form lasting relationships with primary care providers because of the high turnover of doctors and the reliance of many clinics on rotating medical residents.
Perceived Discrimination and Stigma
Focus group discussions corroborated the elevated rates of perceived discrimination and stigma reported in the structured interviews and illustrated how the interactions of participants’ multiple identities as Hispanic with SMI impacted their medical care. A common experience reported by participants was how their medical complaints were often dismissed by medical providers because they were identified as having a mental disorder, as illustrated by the examples from Marta and Marcos, respectively:
And the amazing thing about this is that once you wait 3 months to be seen if you are a psychiatric patient they tell you there is nothing wrong with you.
One time it happened in the hospital. My stomach hurt and I kept telling them, but they just gave me a Tylenol. I ended up passing out. It was my appendix … They just did not believe me.
Participants also described experiencing discrimination from medical staff, as illustrated by the following vignette developed from one of our focus groups:
Isabel recounted how she experienced discrimination seeking medical attention for respiratory problems and chest pains. Isabel arrived at her clinic accompanied by her brother and asked to see her doctor even though she did not have an appointment. The receptionist wrote down her name, and she waited to be seen. After two hours of worsening symptoms, Isabel approached a staff nurse to find out how much longer it would be and stressed that she was having trouble breathing. The nurse informed her that she could not be seen that day as she did not have an appointment. At that point, Isabel recounts that she became irate, explained that her name had already been taken down by the receptionist two hours ago. She stated she wanted to be seen by a doctor as it was an emergency, and she had been a patient at the clinic for 15 years. According to Isabel, the staff member replied, ‘You Hispanics are always sick. You never get well.’ At this point, Isabel began arguing with the nurse and, in response to her racist remark told the nurse, “it is because of us Hispanics that you eat in your home … that you pay your rent … And let me tell you something, you’re not a professional, because a professional would not speak to a patient the way you are speaking to me.” After another nurse at the clinic got involved, Isabel and her brother were finally taken to an examination room. They remained in the examination room for another hour while her symptoms continued, until her brother lost his patience and pleaded with the staff to provide medical attention to his sister. When the doctor finally came into the room, he told Isabel that he had forgotten that she was in there, which only upset and offended her further. Isabel recounted that she ended her appointment crying out of anger, frustration, and physical discomfort. When asked during the focus group about this experience, she replied, “A person becomes depressed. I started to cry. I wanted to die from crying. I asked myself, ‘What is this?’
This vignette illustrates how some participants often felt dehumanized and disrespected by the very system that is supposed to help them during times of need and vulnerability.
Relationship with Primary Care Providers
Twelve of the patients who participated in the focus groups talked about having negative relationships with their primary care providers. These negative experiences were commonly described as interactions where participants perceived their medical providers as rude, impersonal, and displaying a detached interpersonal style. This style was often described by participants as being rushed through their medical visits, and not paid attention to by their doctors, as captured by the comments from Sandra:
Doctors don’t pay attention to us is because now the doctor is only on the computer. They don’t face you to talk, instead you simply keep talking and he goes on asking, “How are you feeling?” They don’t give you their attention.
Participants felt angry, frustrated and even disrespected by the lack of personal attention during the medical encounter with their primary care doctors, as captured by this exchange:
Moderator: For those of you whose doctors don’t spend much time with you, how does that make you feel?
Carla: Bad.
Sandra: Furious.
Moderator: Furious, bad. Why?
Sandra: Because he doesn’t even look at your face. He starts writing on the computer.
Maria: Mine tells me to shut up when I speak …
As a reaction to these situations, some participants talked about not feeling comfortable asking questions and taking on a passive role during the medical visit. These negative experiences also reinforced the sense of stigma and mistrust patients often felt within the medical system, resulting in doctors ignoring participants’ physical complaints and providing poor quality of care. For example, Cristina described an incident where a serious medical condition was completely overlooked because providers focused solely on her psychiatric issues:
I go to the clinic over there … They tell me everything is fine, and they stick me in psychiatry. They don’t pay attention. I can go with a pain, and they commit me – instead of admitting me to the hospital to check me, as has happened many times … The last time I went it was for an infection, and I had pain in my kidneys and they hospitalized me [in psychiatry]. I was hospitalized for three weeks, and it looked like a plume of blood coming through my pee. That’s when they discovered that I had cancer. They hospitalized me and operated.
Similarly, Angela talked about how her primary care doctor dismissed her physical symptoms because of Angela’s mental health issues and failed to diagnose and properly treat a painful physical injury that lasted more than a year. These lapses in appropriate medical care not only impacted the participants’ physical health, but had serious implications for her livelihood:
I had a White doctor for about 5–7 years and I came to understand that she made grave mistakes. For example, I fell and ripped two tendons, a bone came out of place, and I had a lot of arthritis here … And I waited one year for her to pay attention to me because I went to her immediately when I fell. I told her I had a lot of pain and she told me, “Go to [physical] therapy and take an anti-anxiety pill” … Exactly one year passed. And I couldn’t handle the pain any more. I would go to the [physical] therapies. That did nothing for me. And I changed therapists. And when I changed therapists, changed clinics … I said to my new Dominican doctor, “Since I take pills for depression, tell me if it’s that I’m going crazy or if it’s that I have something, because I have a pain here that I can’t take and my [previous] doctor doesn’t pay attention to me.” So that’s when she took action, but it took a year. They did tests and it came out that I had a problem. They did an MRI and it showed that I had two ripped tendons. All of that could have been avoided. I lost my job. I lost my apartment. I lost everything because they had to operate on me.
Lastly, negative relationships with primary care doctors were characterized by situations where clinicians ignored patients’ psychosocial circumstances in formulating treatment recommendations. These situations reinforced patients’ perceptions that doctors do not listen to them and do not provide care that addresses their main concerns, as exemplified by Sandra’s comments:
I have an example which took place the first time I was supposed to take blood pressure medication. I went to a doctor. I was dealing with a lot of stress at that time. I was taking medication for depression. I had a huge stress because they were going to send me to court. I was going to lose my apartment … This was about eight years ago. The doctor immediately wrote me a prescription. I told him, “Doctor, I don’t have high blood pressure. What I have is a lot of stress because I need to pay my rent.” I told him, “I’m not going to take the medication.” So he told me to come back in one month, without me taking them. When I went back a month later, I had paid my rent. And when I went, my blood pressure was normal. And he asked me, “What did you do?” I said, “I paid the rent.”
In contrast, positive relationships with primary care providers were characterized by the personal attention, warmth, and genuine interest participants received from their doctors. Participants valued providers who asked personal questions and displayed familiarity not only with their medical histories but also with their personal and psychosocial issues. Participants were impressed by doctors who referenced this knowledge during their visits because it was perceived as a sign of the doctors’ genuine interest in their patients as people, thus engendering trust (confianza). This sentiment was best captured by Rosa’s comments:
When my doctor said to me, “How is your grandmother?” he surprised me because I didn’t know he remembered my grandmother, and I thought it was going to be a routine visit where he was going to say to me: “We’ll draw blood. How is your health? How are you feeling?” These are more or less the normal questions. But when he came out with, “How is your grandmother?,” I said, wow, this doctor is really in it [éste doctor está en la sopa].
Participants appreciated this atmosphere of open communication where questions from patients were welcomed and encouraged. Because of these interactions, participants expressed being motivated and invested in their treatment, which confirms the significant associations we found between positive experiences with primary care providers and their self-efficacy and patient activation scores. Participants expressed strong preferences for doctors who are personable, caring, and show concern for their well-being by providing lifestyle recommendations to cope with their chronic medical issues. This was best captured by Gonzalo, who described his doctor’s treatment approach as follows:
Well, I have a doctor who is a dear (un amor), like my grandmother says. He gives me my medications – they are for blood pressure. But he hasn’t given me any more medications. In other words, instead of him telling me “this medication would be good for you,” he’ll more readily say, “better to eat this soup or drink this.” Now, it’s not that he avoids medication but, instead of prescribing me more medications he tries to tell me, “do more exercise. Eat healthier. Do this.” He talks to me too. He’s a good person … He’s a good person in that first he counsels you before you get an illness… He works on prevention.
When participants were asked what their doctors do to inspire confidence and trust in them, they most often cited examples of doctors who provided individualized attention and made an effort to get to know their patients from both a personal and medical standpoint. Monica’s comment exemplifies the personal interest participants like to see from their providers and the importance of being treated as a person, not just another case:
I am not a patient, but someone in particular, his particular patient and he is caring for me and is taking the time to give me his attention. I’m not merely a record in the files. Instead, he is giving his attention personally to me.
Lastly, participants also discussed how doctors’ personal attention, friendliness, and warmth help counter the stigma patients face because of their mental conditions, as discussed by Gonzalo:
I prefer a doctor who treats me like a friend, like a person who goes there with problems, but who says…you know, not a person who looks at you as having a defect. Because there are people who you tell, “I have this mental or physical problem,” and at once they put up a barrier. I prefer that communication occurs between the two and that he learns about my personal things. For example, “Are you married? Do you have a girlfriend?” All of those personal things my doctor knows about me. And it seems like a good thing to me, because like that he knows about me.
Discussion
To our knowledge, this is one of the first studies to examine how Hispanic adults with SMI view their primary health care experiences. Overall, our participants reported high levels of medical need that mirror the medical needs of most people with SMI receiving outpatient mental health services (Druss & Walker, 2011). Yet in terms of indicators of patient-centered care, our participants reported lower scores than in previous research conducted with clinical samples of people with and without mental disorders. The mean PACIC score in our sample (2.5, sd = 1.04) was lower than that reported among patients with type 2 diabetes (3.2, sd = 0.9) in a large muti-ethnic sample (Glasgow et al., 2005), Hispanic patients with diabetes mellitus (3.17, sd = 0.82) (Aragones et al., 2008) and primary care sample patients with major depression (3.25, sd = 0.79) (Gensichen et al., 2011). The mean self-efficacy score in our sample (5.90, sd, 2.29) was lower than that reported in a large Spanish-speaking Hispanic sample receiving care for chronic diseases (6.17, sd = 2.96) (K. R. Lorig, Ritter, & Jacquez, 2005) and people with SMI and one chronic medical condition (6.5, sd = 1.7) in a self-management study (Goldberg et al., 2012). Our average PAM score (55.28, sd = 18.03) was also lower than the score reported in a national sample of Hispanics (m = 62.6) and non-Hispanic whites (m = 66.2) (Hibbard & Cunningham, 2008).
These findings suggest that Hispanics with SMI are prime candidates for health care interventions that focus on improving care coordination, goal setting, patient activation, and self-management behaviors. More research is needed to examine the best implementation strategies to bring existing health care manager (Druss et al., 2010; Kilbourne et al., 2008) and self-management interventions (Goldberg et al., 2012) to Hispanics with SMI, particularly within public outpatient mental health clinics, and test their effectiveness and cost-effectiveness in these settings.
Consistent with findings from studies of people with SMI (Druss, 2007), we found that our participants experienced an array of structural barriers, such as fragmented care, long wait times, overburdened clinics, and high staff turnover. In addition to these common structural barriers, our participants also contended with language barriers adding an extra layer of obstacles to receiving medical care. These structural barriers can prevent many Hispanics with SMI from seeking and engaging in medical care and from receiving continuous primary care, particularly when faced with a combination of language barriers, low financial resources, and the symptoms of serious mental disorders.
The implementation of patient-centered medical homes supported by the Patient Protection and Affordable Care Act and other quality improvement interventions are viable approaches that can tackle these structural barriers by focusing on care coordination and service integration (Druss & Mauer, 2010). The aim of integrated mental and medical care for people with SMI is to reduce service fragmentation and facilitate continuity of medical care (Alakeson, Frank, & Katz, 2010). Our findings suggest that integrated approaches must also pay attention to language barriers and the provision of linguistically and culturally appropriate services through the use of bilingual providers and/or trained interpreters along the entire continuum of care. More research is needed to test the impact and cost-effectiveness of these interventions in reducing structural barriers to primary care and improving health care quality and outcomes among populations with SMI, particularly those from historically underserved minority communities.
At a social level, the majority of our participants reported that people are treated unjustly because of a combination of social labels associated with having a mental disorder, being a member of an ethnic minority group, and speaking Spanish. Racism and stigma are known barriers to medical care (Institute of Medicine, 2003, 2006). For example, previous studies indicate that people with SMI often feel discriminated because of their mental illness resulting in underutilization and disengagement from medical care (Borba et al., 2012; Thornicroft, 2006). Our findings expand upon previous work by uncovering possible mechanisms that can help explain how the combination of perceived racism and stigma in the medical encounter results in poor quality of care and negative health outcomes for Hispanics with SMI.
We found that, because of participants’ mental health and minority status, their physical complaints were often dismissed and ignored by medical providers, delaying the diagnosis of medical conditions and the receipt of appropriate care. Although we are unable to disentangle the unique contributions stigma and racism in shaping the primary health care experiences of Hispanics with SMI, the intersection of these two social identities in an individual appears at times to activate multiple biases and prejudices that shape how medical providers interpret physical health complaints. Labeling a patient as having a psychiatric condition can result in providers’ questioning and doubting whether the patient’s complaints are due to a medical condition or are part of his or her psychiatric disorder, a phenomenon known as diagnostic overshadowing (Jones et al., 2008). The patient’s Hispanic identity can also activate other clinician biases, such as the unexamined assumption that the patient’s physical complaints are somatized descriptions of psychological symptoms, rather that signs of physical illness, a phenomenon also labeled as unexplained physical symptoms and frequently described among Hispanic patients (Escobar, Burnam, Karno, Forsythe, & Golding, 1987). In the presence of patients with both of these social identities (Hispanics with SMI), these biases can interact resulting in a cognitive barrier for clinicians that may interfere with a full examination of the clinical situation. Additional barriers include those due to linguistic and cultural differences between patients and providers and to a lack of familiarity with the patients’ medical and mental health history, as is often the case in busy public primary care clinics with high staff turnover.
Our findings indicate that the combination of perceived stigma and racism are critical targets for improving the primary health care of Hispanic with SMI. Anti-stigma and cultural competence training programs can help raise providers’ awareness of these issues and help shift maladaptive attitudes and biases. These training programs should stress principles of recovery from SMI, help providers develop better assessment and engagement skills, educate clinicians about mental disorders and evidence-based treatments, and enable medical providers to interact with members of minority groups living with SMI. Past studies have shown that education and positive social contact with people with mental illness and education are effective strategies for reducing stigma toward mental illness (Corrigan, Morris, Michaels, Rafacz, & Rusch, 2012).
Given the negative impact that perceived stigma and racism had in our study in the identification of medical conditions, primary care providers should attend to and explicitly elicit patients’ explanatory models of their health concerns in order to clarify patients’ views about causes, symptoms, course, consequences, help-seeking experiences, and expected outcomes of their health complaints (Kleinman & Benson, 2006). This patient-centered approach has multiple benefits that can reduce providers’ biases and patients’ perceived stigma and discrimination. It conveys to the patient that the provider is interested in understanding patients’ personal narratives of their health concerns (Lewis-Fernandez & Diaz, 2002) and enables the provider to move beyond stereotypes and group-level knowledge and gather individual-level information about the patient’s socio-cultural context involved in their illness experience that can help clarify diagnostic and treatment decisions (Kleinman & Benson, 2006). This approach is also compatible with the cultural value of personalismo which leads Hispanic patients to expect a personalized, informed, and warm relationship with their providers (Organista, 2007). Lastly, the integration of medical and mental health services for people with SMI can help reduce providers’ stigma and biases by creating formal structures and relationships for sharing medical information, thereby clarifying the patient’s clinical picture and helping providers disentangle the contribution of physical and mental symptoms (Druss, 2007).
Participants’ relationships with their primary care providers revealed important insights about what they valued and preferred during the medical encounter. Positive relationships with primary care providers were characterized by clinicians who displayed an interpersonal style that was compatible with core cultural norms, such as personalismo, respeto, and dignidad, valued by Hispanic cultures. That is, patients valued providers who were warm, friendly, trustworthy, and displayed genuine interest in familiarizing themselves with patients’ social context by inquiring about their social lives, personal situations, and family history. The presence of these cultural norms seems to function as “social lubrication needed to build confianza, or trust” (Organista, 2007, p. 143) Our findings indicate that these cultural norms should be operationalized and integrated into health care interventions to guide providers’ in being more responsive to Hispanic patients’ needs and preferences, as they resulted in participants feeling welcomed and respected and contributed to developing open communication and trust during the medical encounter.
Furthermore, positive relationships with primary care providers were significantly associated with higher scores in participants’ assessments of chronic illness care, self-efficacy, and patient activation. These positive associations are consistent with previous findings that patients’ trust in their primary care providers is related to greater patient activation and involvement in health care (Becker & Roblin, 2008). Although our cross-sectional design prevents us from establishing causality between patient-doctor relationships and patient-centered care, our findings suggest that a plausible pathway for improving the quality of medical care and enhancing activation and self-efficacy in managing chronic medical conditions among Hispanic patients with SMI is to cultivate positive, trustworthy, and culturally compatible patient-doctor relationships that are shaped by the core cultural norms of personalismo, respeto, and dignidad. Longitudinal studies are needed to examine the impact that culturally-compatible patient-doctor relationships have on quality of care, patient self-management behaviors, and ultimately quality of life.
Several study limitation must be considered. The cross-sectional nature of our study prevented us from drawing causal inferences. Our small purposive sample of mostly Dominican patients from one public outpatient mental health clinic in New York City prevents us from generalizing our findings to other subgroups of Hispanics with SMI in different urban, suburban, and rural communities. Lastly, the measures used in our structured interviews relied on patients’ self-report which are subject to recall biases. Future research in this area would benefit from larger representative clinical samples using longitudinal designs to better understand the determinants of medical care affecting Hispanic patients and their resulting health care experiences.
In all, our grounded model captured the multiple structural, social, and relational factors involved in the primary health care experiences of Hispanics with SMI. Our findings highlight the saliency that Hispanic patients with SMI place in their relationships with their primary care doctors and how these relationships can help buffer the structural and social barriers faced by these patients when seeking and receiving medical care. Our results show that if patients do not feel valued and understood and do not trust their primary care providers, they will not engage in medical care and self-management behaviors. A culturally compatible, patient-centered relationship with a health care provider is the bedrock of any successful health care intervention, particularly among Hispanic patients with SMI facing multiple structural and social barriers to care.
Acknowledgments
An earlier version of this paper was presented at the 2013 Society for Social Work and Research Annual Conference in San Diego, CA. This work was supported in part by the New York State Office of Mental Health, and NIH grants: K01 MH091108, R01 MH77226, R25 MH080916, and K24 MH075867. The content of this article is solely the responsibility of the authors and does not represent the official views of the National Institutes of Health.
Contributor Information
Leopoldo J. Cabassa, Email: ljc2139@columbia.edu, School of Social Work, Columbia University and the New York State Center of Excellence for Cultural Competence, New York State Psychiatric Institute, New York, NY, USA.
Arminda P. Gomes, Email: apg6@columbia.edu, School of Social Work, Columbia University, New York, NY, USA
Quisqueya Meyreles, Email: Meyrele@nyspi.columbia.edu, New York State Psychiatric Institute, New York, NY, USA.
Lucia Capitelli, Email: capitel@nyspi.columbia.edu, New York State Psychiatric Institute, New York, NY, USA.
Richard Younge, Email: rgy2103@columbia.edu, Columbia Center for Family and Community Medicine, Columbia University, New York, NY, USA.
Dianna Dragatsi, Email: Dragats@nyspi.columbia.edu, Department of Psychiatry, Columbia University and the New York State Psychiatric Institute, New York, NY, USA.
Juana Alvarez, Email: alvarezj@nyspi.columbia.edu, New York State Psychiatric Institute, New York, NY, USA.
Benjamin Druss, Email: bdruss@emory.edu, Emory University, Atlanta, GA, USA.
Roberto Lewis-Fernández, Email: Rlewis@nyspi.columbia.edu, Department of Psychiatry, Columbia University and the New York State Psychiatric Institute, New York, NY, USA.
References
- Alakeson V, Frank RG, Katz RE. Specialty care medical homes for people with severe, persistent mental disorders. Health Affairs. 2010;29(5):867–873. doi: 10.1377/hlthaff.2010.0080. [DOI] [PubMed] [Google Scholar]
- Aragones A, Schaefer EW, Stevens D, Gourevitch MN, Glasgow RE, Shah NR. Validation of the Spanish translation of the Patient Assessment of Chronic Illness Care (PACIC) survey. Preventing Chronic Disease. 2008;5(4):A113. [PMC free article] [PubMed] [Google Scholar]
- Becker ER, Roblin DW. Translating primary care practice climate into patient activation: the role of patient trust in physician. Medical Care. 2008;46(8):795–805. doi: 10.1097/MLR.0b013e31817919c0. [DOI] [PubMed] [Google Scholar]
- Borba CP, Depadilla L, McCarty FA, von Esenwein SA, Druss BG, Sterk CE. A Qualitative Study Examining the Perceived Barriers and Facilitators to Medical Healthcare Services among Women with a Serious Mental Illness. Womens Health Issues. 2012;22(2):e217–224. doi: 10.1016/j.whi.2011.10.001. S1049-3867(11)00243-X [pii] [DOI] [PubMed] [Google Scholar]
- Cabassa LJ, Hansen MC, Palinkas LA, Ell K. Azucar y nervios: explanatory models and treatment experiences of Hispanics with diabetes and depression. Social Science & Medicine. 2008;66(12):2413–2424. doi: 10.1016/j.socscimed.2008.01.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corrigan PW, Morris SB, Michaels PJ, Rafacz JD, Rusch N. Challenging the public stigma of mental illness: a meta-analysis of outcome studies. Psychiatric Services. 2012;63(10):963–973. doi: 10.1176/appi.ps.201100529. [DOI] [PubMed] [Google Scholar]
- Creswell JW. Research design: Qualitative, quantitative and mixed methods approaches. 2. Thousand Oaks: Sage Publications; 2003. [Google Scholar]
- Druss BG. Improving medical care for persons with serious mental illness: challenges and solutions. Journal of Clinical Psychiatry. 2007;68(Suppl 4):40–44. [PubMed] [Google Scholar]
- Druss BG, Mauer BJ. Health care reform and care at the behavioral health--primary care interface. Psychiatric Services. 2010;61(11):1087–1092. doi: 10.1176/appi.ps.61.11.1087. [DOI] [PubMed] [Google Scholar]
- Druss BG, von Esenwein SA, Compton MT, Rask KJ, Zhao L, Parker RM. A randomized trial of medical care management for community mental health settings: the Primary Care Access, Referral, and Evaluation (PCARE) study. American Jounral of Psychiatry. 2010;167(2):151–159. doi: 10.1176/appi.ajp.2009.09050691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Druss BG, Walker ER. Mental disorders and medical comorbidity. Syntheis Project: Research Synthesis Report. 2011;(21):1–26. [PubMed] [Google Scholar]
- Druss BG, Zhao L, Cummings JR, Shim RS, Rust GS, Marcus SC. Mental comorbidity and quality of diabetes care under Medicaid: a 50-state analysis. Medical Care. 2012;50(5):428–433. doi: 10.1097/MLR.0b013e318245a528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Druss BG, Zhao L, Von Esenwein S, Morrato EH, Marcus SC. Understanding excess mortality in persons with mental illness: 17-year follow up of a nationally representative US survey. Medical Care. 2011;49(6):599–604. doi: 10.1097/MLR.0b013e31820bf86e00005650-201106000-00011. [pii] [DOI] [PubMed] [Google Scholar]
- Escobar JI, Burnam MA, Karno M, Forsythe A, Golding JM. Somatization in the community. Archives of General Psychiatry. 1987;44:713–718. doi: 10.1001/archpsyc.1987.01800200039006. [DOI] [PubMed] [Google Scholar]
- Frosch DL, May SG, Rendle KA, Tietbohl C, Elwyn G. Authoritarian physicians and patients’ fear of being labeled ‘difficult’ among key obstacles to shared decision making. Health Affairs. 2012;31(5):1030–1038. doi: 10.1377/hlthaff.2011.0576. [DOI] [PubMed] [Google Scholar]
- Gensichen J, Serras A, Paulitsch MA, Rosemann T, Konig J, Gerlach FM, Petersen JJ. The Patient Assessment of Chronic Illness Care questionnaire: evaluation in patients with mental disorders in primary care. Community Ment Health Journal. 2011;47(4):447–453. doi: 10.1007/s10597-010-9340-2. [DOI] [PubMed] [Google Scholar]
- Glasgow RE, Whitesides H, Nelson CC, King DK. Use of the Patient Assessment of Chronic Illness Care (PACIC) with diabetic patients: relationship to patient characteristics, receipt of care, and self-management. Diabetes Care. 2005;28(11):2655–2661. doi: 10.2337/diacare.28.11.2655. [DOI] [PubMed] [Google Scholar]
- Goldberg RW, Dickerson F, Lucksted A, Brown CH, Weber E, Tenhula WN, Dixon LB. Living Well: An Intervention to Improve Self-Management of Medical Illness for Individuals With Serious Mental Illness. Psychiatric Services. 2012 doi: 10.1176/appi.ps.201200034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hellerstein DJ, Almeida G, Devlin MJ, Mendelsohn N, Helfand S, Dragatsi D, Capitelli L. Assessing obesity and other related health problems of mentally ill Hispanic patients in an urban outpatient setting. Psychiatric Quarterly. 2007;78(3):171–181. doi: 10.1007/s11126-007-9038-y. [DOI] [PubMed] [Google Scholar]
- Henderson DC, Nguyen DD, Copeland PM, Hayden DL, Borba CP, Louie PM, Goff DC. Clozapine, diabetes mellitus, hyperlipidemia, and cardiovascular risks and mortality: results of a 10-year naturalistic study. Journal of Clinical Psychiatry. 2005;66(9):1116–1121. doi: 10.4088/jcp.v66n0905. [DOI] [PubMed] [Google Scholar]
- Hibbard JH, Cunningham PJ. How engaged are consumers in their health and health care, and why does it matter? Research Brief. 2008;(8):1–9. [PubMed] [Google Scholar]
- Hibbard JH, Mahoney ER, Stockard J, Tusler M. Development and testing of a short form of the patient activation measure. Health Services Research. 2005;40(6 Pt 1):1918–1930. doi: 10.1111/j.1475-6773.2005.00438.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hibbard JH, Tusler M. Assessing activation stage and employing a “next steps” approach to supporting patient self-management. Jounral of Ambulatory Care Manage. 2007;30(1):2–8. doi: 10.1097/00004479-200701000-00002. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine. Crossing the quality chasm: a new health system for the 21st century. Washington, D.C: National Academy Press; 2001. [PubMed] [Google Scholar]
- Institute of Medicine. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington DC: National Academy Press; 2003. [PubMed] [Google Scholar]
- Institute of Medicine. Improving Quality of Health Care for Mental and Substance use Conditions: Quality Chasm Series. Washington D.C: National Acadmy Press; 2006. [PubMed] [Google Scholar]
- Interian A, Martinez I, Rios LI, Krejci J, Guarnaccia PJ. Adaptation of a motivational interviewing intervention to improve antidepressant adherence among Latinos. Cultural Diversity and Ethnic Minority Psychology. 2010;16(2):215–225. doi: 10.1037/a0016072. 2010-07475-014 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones S, Howard L, Thornicroft G. ‘Diagnostic overshadowing’: worse physical health care for people with mental illness. Acta Psychiatric Scandinavia. 2008;118(3):169–171. doi: 10.1111/j.1600-0447.2008.01211.x. [DOI] [PubMed] [Google Scholar]
- Kato MM, Currier MB, Gomez CM, Hall L, Gonzalez-Blanco M. Prevalence of Metabolic Syndrome in Hispanic and Non-Hispanic Patients With Schizophrenia. Primary Care Companion: Journal of Clinical Psychiatry. 2004;6(2):74–77. doi: 10.4088/pcc.v06n0205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kilbourne AM, Post EP, Nossek A, Drill L, Cooley S, Bauer MS. Improving medical and psychiatric outcomes among individuals with bipolar disorder: a randomized controlled trial. Psychiatric Services. 2008;59(7):760–768. doi: 10.1176/ps.2008.59.7.760. [DOI] [PubMed] [Google Scholar]
- Kleinman A, Benson P. Anthropology in the clinic: the problem of cultural competency and how to fix it. PLoS Med. 2006;3(10):e294. doi: 10.1371/journal.pmed.0030294. 06-PLME-ES-0159R1 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lambert BL, Chou CH, Chang KY, Tafesse E, Carson W. Antipsychotic exposure and type 2 diabetes among patients with schizophrenia: a matched case-control study of California Medicaid claims. Pharmacoepidemioly Drug Safety. 2005;14(6):417–425. doi: 10.1002/pds.1092. [DOI] [PubMed] [Google Scholar]
- Lewis-Fernandez R, Diaz N. The cultural formulation: a method for assessing cultural factors affecting the clinical encounter. Psychiatric Quarterly. 2002;73(4):271–295. doi: 10.1023/a:1020412000183. [DOI] [PubMed] [Google Scholar]
- Lillie-Blanton M, Brodie M, Rowland D, Altman D, McIntosh M. Race, ethnicity, and the health care system: public perceptions and experiences. Medical Care Research Review. 2000;57(Suppl 1):218–235. doi: 10.1177/1077558700057001S10. [DOI] [PubMed] [Google Scholar]
- Lorig K, Stewart A, Ritter P, González V, Laurent D, Lynch J. Outcome Measures for Health Education and other Health Care Interventions. Thousand Oaks, CA: Sage Publications; 1996. [Google Scholar]
- Lorig KR, Ritter PL, Jacquez A. Outcomes of border health Spanish/English chronic disease self-management programs. Diabetes Educator. 2005;31(3):401–409. doi: 10.1177/0145721705276574. [DOI] [PubMed] [Google Scholar]
- McEvoy JP, Meyer JM, Goff DC, Nasrallah HA, Davis SM, Sullivan L, Lieberman JA. Prevalence of the metabolic syndrome in patients with schizophrenia: baseline results from the Clinical Antipsychotic Trials of Intervention Effectiveness (CATIE) schizophrenia trial and comparison with national estimates from NHANES III. Schizophrenia Research. 2005;80(1):19–32. doi: 10.1016/j.schres.2005.07.014. [DOI] [PubMed] [Google Scholar]
- Muhr T. User’s manual for ATLAS.ti 5.0. 2. Berlin: Scientific Software Development; 2004. [Google Scholar]
- Nasrallah HA, Meyer JM, Goff DC, McEvoy JP, Davis SM, Stroup TS, Lieberman JA. Low rates of treatment for hypertension, dyslipidemia and diabetes in schizophrenia: data from the CATIE schizophrenia trial sample at baseline. Schizophrenia Research. 2006;86(1–3):15–22. doi: 10.1016/j.schres.2006.06.026. [DOI] [PubMed] [Google Scholar]
- Organista KC. Solving Latino psychosocial and health problems: Theory, practice, and population. Hoboken, New Jeresey: John Wiley & Sons; 2007. [Google Scholar]
- Padgett DK. Qualitative methods in social work research: Challenges and rewards. Thousand Oaks, CA: Sage; 1998. [Google Scholar]
- Palmer RM, Meldon SW. Acute Care. In: Hazzard WR, editor. Principles of Geriatric Medicine and Gerontology. Boston, MA: McGraw-Hill; 2003. pp. 157–168. [Google Scholar]
- Skolasky RL, Mackenzie EJ, Wegener ST, Riley LH., 3rd Patient activat ion and adherence to physical therapy in persons undergoing spine surgery. Spine. 2008;33(21):E784–791. doi: 10.1097/BRS.0b013e31818027f1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strauss AL, Corbin J. Basics of qualitative research: Techniques and procedures for developing grounded theory. 2. Thousand Oaks: Sage; 1998. [Google Scholar]
- Thornicroft G. Shunned: Discrimination against people with mental illness. New York, NY: Oxford University Press; 2006. [Google Scholar]
- Zayas LH, Cabassa LJ, Pérez MC. Capacity-to-consent in psychiatric research: Development and preliminary testing of a screening tool. Research on Social Work Practice. 2005;15(16):545–556. [Google Scholar]