Abstract
Aim:
To examine the effects of all-trans retinoic acid (atRA) on renal morphology and function as well as on renal plasminogen activator inhibitor-1 (PAI-1) expression and plasmin activity in rats with 5/6 nephrectomy.
Methods:
Adult male Sprague Dawley rats were given 5/6 nephrectomy or sham operation. Renal function was measured 2 weeks later. The nephrectomized rats were assigned to groups matched for proteinuria and treated with vehicle or atRA (5 or 10 mg/kg by gastric gavage once daily) for the next 12 weeks. Rats with sham operation were treated with vehicle. At the end of the treatments, kidneys were collected for histological examination, Western blot analysis, and enzymatic activity measurements.
Results:
The 5/6 nephrectomy promoted hypertension, renal dysfunction, and glomerulosclerosis. These changes were significantly reduced in the atRA-treated group. The expressions of PAI-1 and α-smooth muscle actin (α-SMA) were significantly increased in the vehicle-treated nephrectomized rats. Treatment with atRA significantly reduced the expressions of PAI-1 and α-SMA. However, plasmin activity remained unchanged following atRA treatment.
Conclusion:
Treatment with atRA ameliorates glomerulosclerosis and improves renal function in rats with 5/6 nephrectomy. This is associated with a decrease in PAI-1 and α-SMA, but not with a change in plasmin activity.
Keywords: nephrectomy, plasminogen activator inhibitor 1, plasmin, retinoids, α-smooth muscle actin
Introduction
Glomerulosclerosis is a common phenomenon associated with renal failure that occurs regardless of the primary cause of damage1. It is characterized by the excessive accumulation of extracellular matrix (ECM) in the glomeruli. When ECM synthesis exceeds its degradation, ECM accumulation occurs2. In various types of glomerular injuries, mesangial cells are activated into ECM-producing myofibroblasts that undergo proliferation. These cells are phenotypically defined by their expression of α-smooth muscle actin (α-SMA)3, 4, 5, 6. Recently, plasminogen activator inhibitor-1 (PAI-1) has been widely recognized as a key contributor in fibrosis. Under physiological conditions, PAI-1 expression is low in the kidney but is upregulated in response to renal injury7. Transgenic mice overexpressing PAI-1 develop severe fibrosis in several experimental fibrosis models8, 9, 10. In contrast, PAI-1 deficiency or inhibition results in decreased fibrosis8, 10, 11, 12, 13, 14, 15, 16. These studies demonstrate a role for PAI-1 in fibrogenesis. PAI-1 is a major physiological inhibitor of tissue-type plasminogen activator (t-PA) and urokinase-type plasminogen activator (u-PA), both of which convert plasminogen to plasmin. Plasmin can activate latent matrix metalloproteinases (MMPs). Plasmin and MMPs play key roles in the regulation of ECM degradation17, 18, 19. PAI-1′s profibrotic effect is presumed to be exerted by inhibiting plasmin generation. This explanation, however, has been disputed in some reports11, 12, 14, 16.
The retinoids are derivatives of vitamin A (retinol) and include all-trans retinoic acid (atRA), 9-cis RA, and 13-cis RA. RAs exert strong anti-proliferative and anti-inflammatory effects. They act via the retinoic acid receptor (RAR) and retinoid X receptor (RXR), which serve as transcription factors to regulate target gene expression. Retinoids have been reported to be renoprotective in some models of renal fibrosis20, 21, 22, 23, 24, 25, 26, 27, 28. We have previously shown that exogenous atRA decreases cardiac fibrosis in spontaneously hypertensive rats (SHR)29 and inhibits the increases in PAI-1 and the ECM protein fibronectin, which are induced by the key fibrogenic cytokines transforming growth factor-β1 (TGF-β1) and angiotensin II (Ang II) in cultured rat mesangial cells30. However, the mechanisms mediating the antifibrotic actions of retinoids remain to be further clarified. In the current study, we examined the effects of chronic atRA treatment on renal function and morphology in a rat model of 5/6 nephrectomy. The renal expressions of PAI-1 and α-SMA were examined. The activities of plasmin and MMP-2 were also measured.
Materials and methods
Experimental design and animals
Adult male Sprague Dawley rats that weighed 250–330 g and were obtained from the Department of Experimental Animals, Chinese Academy of Sciences (Shanghai, China) were used in this study. The rats were housed in plastic cages in a room with a controlled humidity of 40% and a temperature of 22 °C. Their exposure to light was controlled on a 12:12-h light-dark cycle. These rats had free access to water and a regular standard diet (0.6% salt). All experiments were performed in accordance with the national animal protection law. After the measurement of baseline blood pressure and renal function, all rats underwent 5/6 nephrectomy (5/6Nx) or sham operation. 5/6Nx was performed after ventral laparotomy under anesthesia with chloral hydrate (300 mg/kg, ip), by removal of the right kidney and ligation of 2 branches of the left renal artery, producing a total of 5/6 renal ablation. Rats that received sham operation underwent anesthesia, ventral laparotomy, and manipulation of the renal pedicles without removal of renal mass. Renal function was measured 2 weeks later, and nephrectomized rats were divided into three groups matched for proteinuria: 5/6Nx+vehicle (5/6Nx treated with soybean oil as placebo, 1 mL/kg, n=12), 5/6Nx+atRA1 (5/6Nx treated with 5 mg atRA/kg suspended in soybean oil at a concentration of 5 g/L, n=10), and 5/6Nx+atRA2 (5/6Nx treated with 10 mg atRA/kg suspended in soybean oil at a concentration of 10 g/L, n=12). Sham+vehicle (sham-operated rats treated with soybean oil, 1 mL/kg, n=7) served as a normal control. The dosages of atRA were chosen according to previous experiments from our laboratory that demonstrated an effective reduction of cardiac fibrosis in SHR with little toxic effects29. Fresh suspensions of atRA were prepared under reduced lighting conditions each day to limit its spontaneous isomerization to 9-cis RA and 13-cis RA. Oral treatment was performed by gavage once a day for the next 12 weeks. The rats were weighed once a week to adjust the amount of orally administered atRA.
Blood pressure recordings
Prior to operation, blood pressure (BP) was measured by the tail-cuff method in rats. At the end of the study period, the rats were anesthetized with chloral hydrate. A polypropylene tube (Portex, London, UK) was inserted into the left carotid artery and exteriorized behind the neck. The catheters were filled with a heparinized (10 U/mL) saline solution and plugged with a stainless steel pin. After catheterization, the rats were housed individually and had free access to water and rat chow. On the following day, the arterial catheters were attached to a pressure transducer. BP was measured 2-3 h after gavage. After an equilibrium period of 30 min, systolic BP (SBP), diastolic BP (DBP), mean arterial pressure (MAP), and heart rate (HR) were recorded in the conscious, freely moving animals for 30 min. After the hemodynamic parameters were recorded, terminal blood samples were collected for blood chemical analysis.
Assessment of renal function
Renal function was determined every 2 weeks. Rats were housed individually in metabolic cages to collect urine over 24 h. During this time, they were supplied with food and water ad libitum. Urine was stored at -20 °C until measurement. Tail vein blood samples were collected. Urine albumin and urine and serum creatinine concentrations were measured on an autoanalyzer, and the creatinine clearance was calculated accordingly.
Tissue preparation
After hemodynamic measurements at the end of the study period, rats were anesthetized and kidneys were removed immediately. After being washed in cold 0.9% saline, each kidney was blotted dry and cut into two parts. One part was fixed in 10% neutral buffered formalin, and the other part of the renal cortex was rapidly frozen in liquid nitrogen and stored at -80 °C until required for Western blotting and enzymatic activity analysis.
Light microscopy studies
Fixed kidney tissues were embedded in paraffin and cut into 4 μm-thick sections. Sections were stained with periodic acid-Schiff (PAS) reagent and counterstained with hematoxylin. PAS staining is used as a marker for the glomerular basement membrane. Sections were examined by two investigators without previous knowledge of the experimental group of the animal from which the tissue was taken. The semiquantitative glomerulosclerosis index was used to evaluate the degree of glomerular deposition of PAS-positive ECM according to the method of Raij L et al31. The severity of the lesions for each kidney was examined in the 100 glomeruli selected at random, graded from 0-4 points according to the percentage of morphological changes in each glomerulus (0=0%, 1+=1%–25%, 2+=26%–50%, 3+=51%–75%, 4+=76%–100%). The number of glomeruli with lesions of grades 0, 1+, 2+, 3+, and 4+ was n0, n1, n2, n3, and n4, respectively. The glomerular sclerosis index was obtained from the following formula: (0×n0+1× n1+2×n2+3×n3+4×n4)/100.
Western blot analysis
Renal cortical tissue samples were homogenized in lysis buffer containing 20 mmol/L Tris (pH 7.5), 150 mmol/L NaCl, 1% Triton X-100, and a 1:50 dilution of a protease inhibitor cocktail (Roche Applied Science, Penzberg, Germany) on ice followed by centrifugation (12 000× g, 10 min, 4 °C). The supernatant was collected and the protein concentration was measured. Thirty μg of total protein from samples were loaded and separated under reducing conditions with 10% SDS-PAGE and transferred onto PVDF membranes. Membranes were blocked in 5% milk in Tris-buffered saline with 0.1% Tween 20 (TBST) and incubated with the primary antibody against PAI-1 (BD Biosciences/Pharmingen, San Diego, CA, USA), α-SMA (Sigma-Aldrich, Saint Louis, MO, USA) or β-actin (Santa Cruz Biotechnology, CA, USA) followed by incubation with the corresponding peroxidase-conjugated secondary antibody. Peroxidase activity was detected using an enhanced chemiluminescence detection system.
Assay of plasmin activity
The plasmin activity in total renal cortical tissue homogenates was measured using the plasmin-specific chromogenic substrate Chromozym PL (Roche Diagnostics, Indianapolis, IN, USA), as described by Krag S et al14. This substance is specifically cleaved by plasmin into a residual peptide and 4-nitraniline, which can be detected spectrophotometrically at 405 nm. A standard linear curve was generated with serial dilutions of human plasmin (Roche Applied Science, Penzberg, Germany). Plasmin activity was determined from the standard curve. Results were expressed as μU/mg total protein.
Assay of MMP-2 activity
The renal cortex was homogenized, quantitated, and analyzed for MMP-2 activity by a commercial assay kit (Amersham Biosciences, Buckinghamshire, UK). As described in the protocol supplied, any active MMP-2 present in the sample is captured by the anti-MMP-2 antibody, and bound MMP-2 is detected using a specific chromogenic peptide substrate. Standard MMP-2 (0-16 ng/mL) and experimental samples were placed in 96-well plates for the detection of endogenous and active MMP-2. Plates were read at 405 nm at time zero and after 6 h. Active MMP-2 activity was determined from the standard curve. Results were expressed as pg/mg total protein.
Blood chemical analysis
To test for potential side effects of atRA, such as liver and kidney damage, serum parameters were measured using an autoanalyzer methodology.
Statistical analysis
Data were expressed as the mean±SEM. Statistical analysis was performed using SigmaStat 2.0 software. The differences in mean values between groups were analyzed with a one-way ANOVA followed by a Student-Newman-Keuls test or by a Kruskal-Wallis nonparametric ANOVA followed by a Dunn multiple comparison test, as appropriate. Correlation coefficient was tested for statistical significance using the Spearman's rank test and Pearson's rank coefficients. A P value of <0.05 was considered statistically significant.
Results
Effects of atRA treatment on blood pressure and renal function
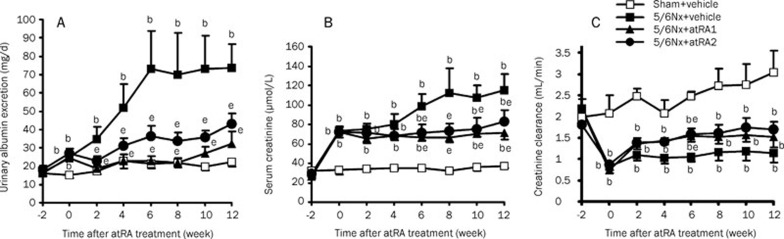
Before the operation, BP measured by the tail-cuff method was similar in all of the groups used in the current study (Table 1). At week 14 after the operation, the systolic, diastolic, and mean BPs directly detected in cannulated, conscious rats were markedly elevated in the 5/6Nx+vehicle group compared with Sham+vehicle rats (P<0.05). Treatment with either dose of atRA decreased systolic BP in 5/6 nephrectomized rats (P<0.05 vs 5/6Nx+vehicle). At the end of the experiment, the average heart rates were similar for each group. Twenty four-hour urinary protein excretion was progressively increased in the 5/6Nx+vehicle group (P<0.05 vs Sham+vehicle) (Figure 1A). Proteinuria was markedly decreased as early as week 2 after atRA administration, and this antiproteinuric effect of atRA was so effective that urinary albumin was almost normalized to control levels (P<0.05 vs 5/6Nx+vehicle). In the 5/6Nx+vehicle group, the serum creatinine concentration remained elevated throughout the entire experimental period (P<0.05 vs Sham+vehicle) (Figure 1B). Treatment with either dose of atRA decreased the elevated serum creatinine levels in 5/6 nephrectomized rats (P<0.05 vs 5/6Nx+vehicle). Following 5/6Nx, rats developed renal failure with a marked decrease in glomerular filtration rate, as estimated by creatinine clearance (P<0.05 vs Sham+vehicle) (Figure 1C). The creatinine clearance in 5/6 nephrectomized rats was slightly increased by atRA. However, this increase only reached statistical significance at the time point of week 6 after atRA administration.
Table 1. Effects of atRA on hemodynamic parameters.
| Group | Initial |
Final (14 week) |
|||
|---|---|---|---|---|---|
| Tail-cuff pressure (mmHg) | SBP (mmHg) | DBP (mmHg) | MAP (mmHg) | HR (beats/min) | |
| Sham+vehicle (n=7) | 125±5 | 144±3 | 101±4 | 120±4 | 348±6 |
| 5/6Nx+vehicle (n=8) | 121±4 | 189±4b | 132±7b | 160±5b | 339±18 |
| 5/6Nx+atRA1 (n=9) | 124±3 | 166±7be | 113±7 | 138±7 | 363±13 |
| 5/6Nx+atRA2 (n=10) | 125±3 | 167±8be | 116±8 | 144±8b | 340±10 |
Values are mean±SEM. n, number of rats. SBP, systolic blood pressure; DBP, diastolic blood pressure; MAP, mean arterial pressure; HR, heart rate. bP<0.05 vs Sham+vehicle; eP<0.05 vs 5/6Nx+vehicle.
Figure 1.
Effects of atRA on urinary albumin excretion (A), serum creatinine level (B), and creatinine clearance (C). The 5/6 nephrectomy provoked the increases in proteinuria and serum creatinine as well as the reduction in the glomerular filtration rate, as estimated by creatinine clearance. Treatment with atRA (5 or 10 mg/kg) at week 2 after the 5/6 nephrectomy for 12 weeks reduced the increases in proteinuria and serum creatinine. This treatment had no effect on the fall in creatinine clearance except at week 6 after atRA treatment. Values are mean±SEM. n=7–10 rats/group. bP<0.05 vs Sham+vehicle, eP<0.05 vs 5/6Nx+vehicle.
Effect of atRA treatment on glomerulosclerosis
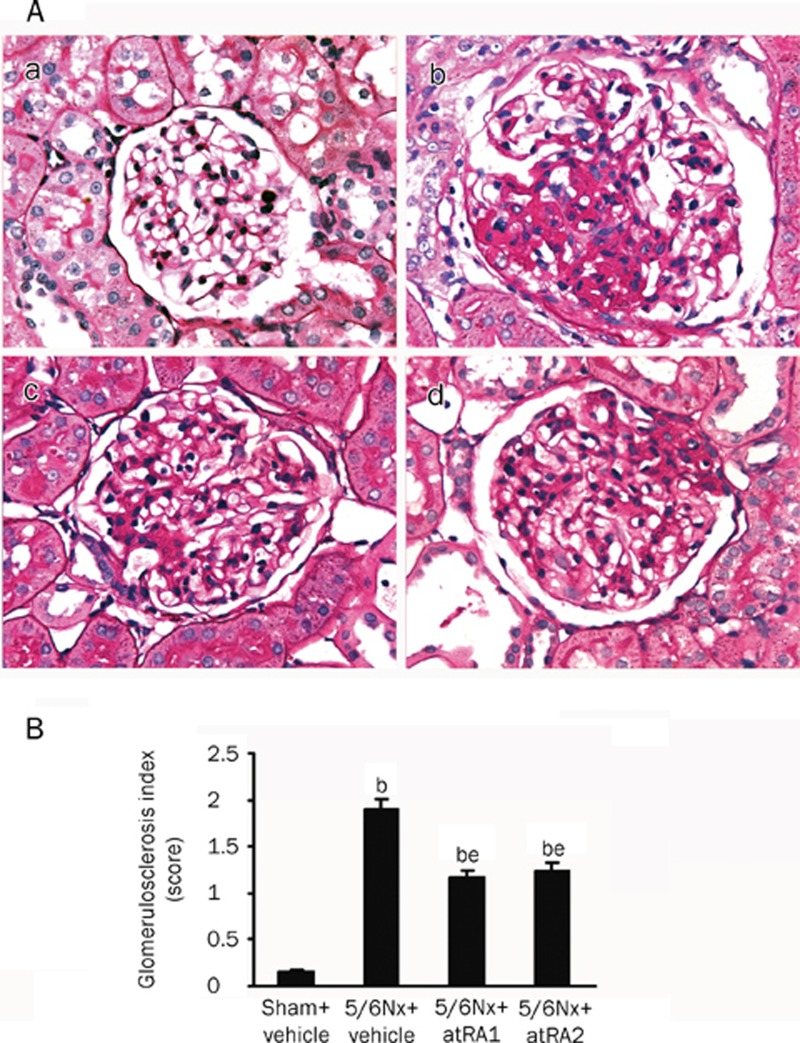
Figure 2A shows representative PAS stains of glomeruli from sham-operated (Figure 2Aa) and 5/6 nephrectomized rats that were treated with vehicle alone (Figure 2Ab), or with low- (Figure 2Ac) or high-dose atRA (Figure 2Ad). The glomerular sclerosis index was markedly higher in the 5/6Nx+vehicle group compared to the Sham+vehicle group (P<0.05) (Figure 2B). Treatment with the two doses of atRA lowered the glomerulosclerosis index in 5/6 nephrectomized rats (P<0.05 vs 5/6Nx+vehicle).
Figure 2.
Degree of glomerulosclerosis. (A) Representative images of PAS stains of glomeruli from sham-operated rats treated with vehicle (a) and 5/6 nephrectomized rats that were treated with vehicle (b) or 5 mg/kg atRA (c) or 10 mg/kg atRA (d) once daily. Magnification, ×400. (B) Glomerulosclerosis index (GSI) (0 to 4 score). The GSI was increased in vehicle-treated rats with 5/6 nephrectomy. This increase in GSI was decreased with atRA treatment. Values are mean±SEM. n=7−10 rats/group. bP<0.05 vs Sham+vehicle. eP<0.05 vs 5/6Nx+vehicle.
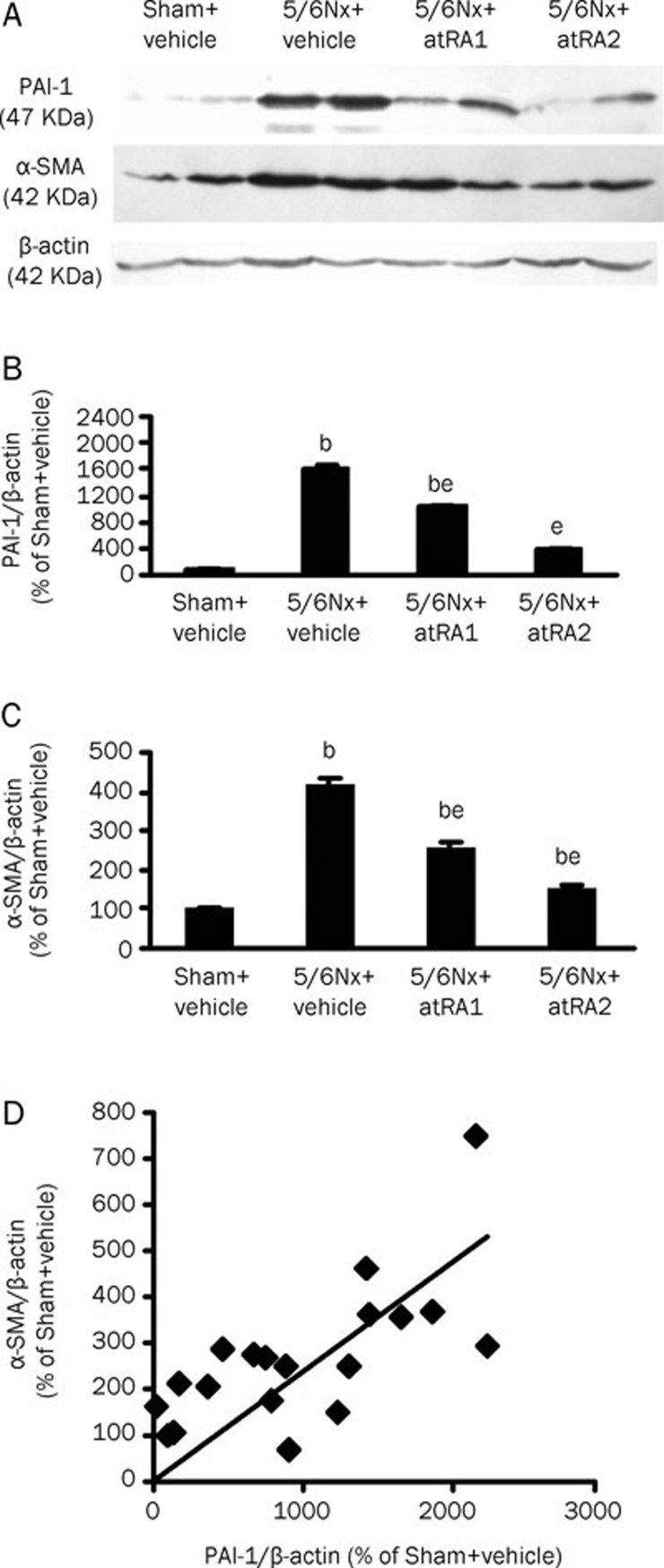
Effect of atRA treatment on protein expressions of PAI-1 and α-SMA
Figure 3A shows the protein expression levels of PAI-1 and α-SMA in renal cortex extract from Western blot analyses. PAI-1 expression was increased approximately 16-fold in the 5/6Nx+vehicle group compared with the Sham+vehicle group (P<0.05) (Figure 3B). PAI-1 expression induced by 5/6Nx was markedly downregulated by atRA treatment in a concentration-dependent fashion (P<0.05 vs 5/6Nx+vehicle). α-SMA expression was increased more than 4-fold in 5/6Nx+vehicle rats compared with Sham+vehicle rats (P<0.05) (Figure 3C). Treatment with atRA markedly suppressed the elevation of α-SMA expression in 5/6 nephrectomized rats in a dose-dependent manner (P<0.05 vs 5/6Nx+vehicle). The expression of α-SMA correlated well with that of PAI-1 (r= 0.759, P<0.0001) (Figure 3D).
Figure 3.
Western blot analysis of protein expressions for plasminogen activator inhibitor-1 (PAI-1) and α-smooth muscle actin (α-SMA) in the renal cortex. (A) Representative protein bands of PAI-1, α-SMA, and β-actin. (B) PAI-1/β-actin protein ratio according to band density. (C) α-SMA/β-actin protein ratio. The protein ratios of PAI-1/β-actin and α-SMA/β-actin were markedly increased in vehicle-treated rats with 5/6 nephrectomy. These increases were attenuated by atRA treatment in a dose-dependent manner. Values are mean±SEM. n=6. bP<0.05 vs Sham+vehicle; eP<0.05 vs 5/6Nx+vehicle. (D) Correlation between α-SMA and PAI-1 expression (r=0.759, P<0.0001).
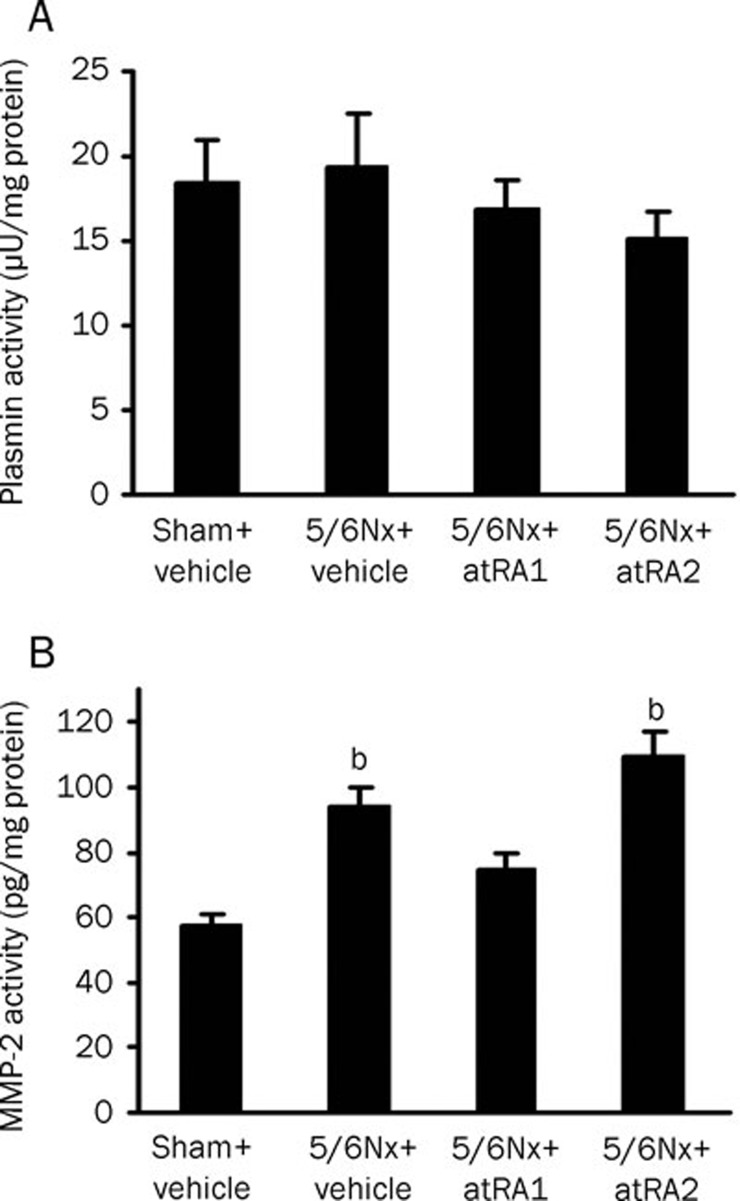
Effect of atRA on the activities of plasmin and MMP-2
Figure 4 shows the activities of plasmin and MMP-2 in kidney cortical homogenates. Somewhat surprisingly, plasmin activity remained unchanged in 5/6 nephrectomized rats (Figure 4A). Moreover, plasmin activity was not altered by either dose of atRA, although PAI-1 expression was downregulated. Also unexpectedly, MMP-2 activity was increased in the 5/6Nx+vehicle group (P<0.05 vs Sham+vehicle) (Figure 4B). The low dose of atRA moderately decreased the elevation of MMP-2 activity in 5/6 nephrectomized rats, but did not reach statistical significance. The high dose of atRA had no effect on MMP-2 activity.
Figure 4.
Chromogenic assay for activities of plasmin (A) and MMP-2 (B) in the renal cortex. Plasmin activity was unchanged and MMP-2 activity was increased in vehicle-treated rats with 5/6 nephrectomy. Treatment with atRA had no effect on the activity of either plasmin or MMP-2. Values are mean±SEM. n=7−10 rats/group. bP<0.05 vs Sham+vehicle.
Effect of atRA on body weight and serum parameters
Table 2 shows that there was no statistical difference in the initial or final body weights of the four groups. There was also no statistical difference in serum parameters such as alanine aminotransferase (ALT), glucose (GLU), triglyceride (TG), and cholesterol (CHO) levels, although at the higher dose of atRA, a slight increase in serum TG level was observed. It is therefore unlikely that either of the two doses of atRA caused any obvious side effects.
Table 2. Effects of atRA on body weight and blood chemistry.
| Group | Initial |
Final (14 week) |
||||
|---|---|---|---|---|---|---|
| Body weight (g) | Body weight (g) | ALT (U/L) | GLU (mmol/L) | TG (mmol/L) | CHO (mmol/L) | |
| Sham+vehicle (n=7) | 283±12 | 546±14 | 80.7±10.6 | 8.53±0.63 | 0.83±0.15 | 1.91±0.14 |
| 5/6Nx+vehicle (n=8) | 289±16 | 538±23 | 75.0±13.9 | 7.46±0.94 | 1.29±0.41 | 1.87±0.09 |
| 5/6Nx+atRA1 (n=9) | 284±11 | 529±20 | 74.8±6.9 | 8.08±0.51 | 1.13±0.11 | 1.84±0.10 |
| 5/6Nx+atRA2 (n=10) | 269±8 | 539±13 | 68.4±9.0 | 7.82±0.56 | 1.75±0.29 | 1.88±0.08 |
Values are mean±SEM. n, number of rats. ALT, alanine aminotransferase; GLU, glucose; TG, triglyceride; CHO, cholesterol. There was no statistical difference in body weight or the blood chemical profile in any group.
Discussion
The major finding of this study is that the amelioration of glomerulosclerosis with atRA is associated with a decrease in PAI-1 and α-SMA, but is not associated with changes in the activities of plasmin and MMP-2. This study expands our understanding of the mechanisms of atRA-mediated renoprotection and provides further evidence that both a pathogenic role for PAI-1 induction and a protective role for PAI-1 inhibition in renal fibrosis might be independent of the effects on the regulation of plasmin and MMP-2 activity.
It has been reported that renin-dependent and renin- independent mechanisms are responsible for hypertension in rats with 5/6Nx32, 33. In the present study, hypertension in 5/6 nephrectomized rats was decreased by treatment with two doses of atRA. This decrease is, at the very least, attributed to the known inhibitory effects of retinoids on the activity of the renin-angiotensin system, particularly on the expression of the Ang II type 1 receptor26, 27. However, previous work from our laboratory has shown that identical doses of atRA tended to lower blood pressure in SHR but failed to reach statistical significance29. Some possible explanations for this may be the different model and the different starting time of atRA administration. Because hypertension is a risk factor for the progression of renal diseases34, a decrease in hypertension underlies the renoprotective effects of atRA.
Twenty four-hour urinary protein excretion was measured every 2 weeks to serve as a surrogate marker for glomerular damage. The time course of proteinuria showed that proteinuria in 5/6 nephrectomized rats was so effectively decreased with atRA treatment that it was almost normalized. This antiproteinuric effect occurred as early as week 2 after treatment. Treatment with atRA has also been reported to decrease proteinuria in other models of kidney disease23, 24, 25. It is well known that defects in the glomerular filtration barrier lead to proteinuria35, and that podocytes play a pivotal role in glomerular barrier function36, 37. The upregulation of nephrin and podocin in podocytes by atRA, in vivo and in vitro, was proposed as a possible mechanism for its antiproteinuric effect23, 24. Because proteinuria is also a risk factor for the progression of renal diseases38, a decrease in proteinuria at least partly mediates the renoprotective effects of atRA.
The glomerular filtration rate, as reflected by creatinine clearance, was markedly decreased by 5/6Nx. This decrease is mainly due to a reduction in functional nephron number. Additionally, with the development of glomerular injury, mesangial cell proliferation and mesangial matrix deposition lead to narrowness or obliteration of glomerular capillary loops39, which eventually results in the loss of originally functional nephrons and a further decrease in glomerular filtration rate. A slightly increased creatinine clearance was observed in atRA-treated 5/6 nephrectomized rats over the period observed. Although this increase appeared to be insignificant, it occurred despite severe nephron loss. Obviously, the increased creatinine clearance in atRA-treated nephrectomized rats is due to less glomerulosclerosis and less destruction of renal structure. Accordingly, the increase in creatinine clearance leads to a decrease in serum creatinine level in the atRA-treated nephrectomized group.
Treatment with atRA decreased glomerulosclerosis in 5/6 nephrectomized rats, as evidenced by the decreased glomerular deposition of PAS positive ECM. It is well known that the cell type responsible for most ECM synthesis is the myofibroblast, distinguished by the acquisition of a α-SMA phenotype. In normal kidney, α-SMA is expressed exclusively in the intrarenal arteries; however, in a number of glomerulonephritis models, mesangial cells are activated into α-SMA positive myofibroblasts and proliferate, producing excessive ECM in glomeruli3, 4, 5, 6. In the present study, Western blot analysis showed that α-SMA expression was increased in the renal cortex of nephrectomized rats and that it was decreased with atRA treatment. Since atRA is a well-known powerful anti-proliferative drug that can inhibit the proliferation of many cell types, including mesangial cells40, 41, 42, 43, 44, we speculate that atRA can inhibit the proliferation of glomerular α-SMA positive myofibroblasts, thus limiting ECM production. Additionally, atRA may inhibit α-SMA expression per cell. Wen X et al45 showed that 9-cis RA, an isomer of atRA, inhibited the TGF-β1-induced α-SMA expression in cultured mesangial cells without influencing cell number.
Recently, attention has focused on the role of PAI-1 in the pathogenesis of fibrosis based on its increased expression in a variety of fibrotic diseases and on the beneficial effects of its inhibition or depletion in some fibrosis models9, 10, 11, 12, 13, 14, 15; however, the mechanism of its action remains controversial. In vitro studies document that ECM degradation by cultured mesangial cells is inhibited by plasmin inhibitors and increased by the addition of a PAI-1 monoclonal antibody19. In experimental anti-thy-1 nephritis, glomerulosclerosis is developed and accompanied by a decrease in plasmin activity in isolated glomeruli; these changes can be reversed by a mutant noninhibitory PAI-1 that competes with endogenous PAI-1 or by recombinant t-PA15, 46. It seems likely that PAI-1 exerts profibrotic effect through inhibiting plasmin generation. However, this explanation is not supported by our study. In the present study, Western blot analysis of renal cortex homogenates showed a greater than 16-fold increase in PAI-1 expression in disease controls compared with sham-operated rats. We expected the activities of plasmin and MMP-2 to decrease. However, plasmin activity was unchanged and MMP-2 activity was increased. Moreover, PAI-1 expression was suppressed by atRA administration. We expected the activities of plasmin and MMP-2 to increase. However, we observed that they were unchanged. This is conceivable based on the fact that PAI-1 is just one of regulators of plasmin activity. For example, α2-antiplasmin is also an inhibitor of plasmin. Indeed, α2-antiplasmin, the most abundant form in normal kidneys, was suppressed following ureteral obstruction11. Consistent with our results, some reports have shown that the increase in PAI-1 and fibrosis is not always accompanied by a decrease in plasmin and MMP-2 activities11, 12, 14, 16. Further, PAI-1 deficiency and decreased fibrosis are not always accompanied by an augmentation of plasmin and MMP-2 activities. These data and our results suggest that PAI-1, at least, has a plasmin/MMP-2-independent fibrogenic function. However, the mechanism by which it controls fibrosis remains largely unknown7. Oda T et al reported that PAI-1 promoted macrophage chemotaxis in vitro11. Our results showed an excellent correlation between α-SMA and PAI-1 expression, but the causal relation between them is not known.
It must be emphasized that PA, plasmin, and MMP are not always protective and have both beneficial and injurious effects on fibrogenesis, depending on the model of fibrosis. Injections with t-PA restored declined glomerular plasmin activity and ameliorated fibrosis in experimental glomerulonephritis46. The deficiency of either plasminogen or t-PA in mice increased the severity of crescentic glomerulonephritis47, but decreased the degree of renal interstitial fibrosis after unilateral ureteral obstruction48, 49. Active MMP-2 has been reported to directly lead to a transition of cultured mesangial cells from the quiescent phenotype to the activated phenotype, characterized by an augmentation in the proliferation and synthesis of ECM proteins50. Active MMP-2 or plasmin can promote the transdifferentiation of murine tubular epithelial cells to myofibroblasts51, 52. Plasmin has also been shown to play a role in leukocyte recruitment53. These data suggest that PA, plasmin, and MMP-2 have other actions in addition to degrading the ECM. Together, all these actions determine whether the net effect is profibrotic or antifibrogenic.
Ang II and TGF-β1 have been established as crucial contributors to ECM expansion and fibrosis in a number of renal diseases54, 55, 56. PAI-1 is strongly induced by these two cytokines. PAI-1 reduction by atRA treatment in the present study is likely to be associated with the retinoids' inhibitory effects on the activities of Ang II/Ang II type 1 receptor and TGF-β1/TGF-β receptor26, 27, 28. We have recently shown that atRA directly inhibits PAI-1 production induced by TGF-β1 and Ang II in cultured mesangial cells in vitro30.
The reduction in PAI-1 and α-SMA by atRA was dose dependent, suggesting that atRA may have direct inhibitory effects on PAI-1 and α-SMA expressions. In contrast, the beneficial effects of atRA on renal function, including decreasing proteinuria and serum creatinine concentration, were inversely dose dependent. This finding may reflect a toxic effect of the higher dose of atRA, as indicated by a slight increase in serum triglyceride levels in rats that received the high dose of atRA (10 mg/kg). Morath C et al showed that higher doses of retinoids may evoke some side effects27. The reduction in the glomerular deposition of ECM by atRA showed no dose-dependent difference. This phenomenon can be explained because high doses of atRA had a tendency to reduce the specific beneficial effects of atRA administration due to its concomitant unspecific toxicity.
Taken altogether, our findings suggest that the beneficial effects of atRA on glomerular damage in a rat model of 5/6 nephrectomy are, in part, due to the reduction of PAI-1 and α-SMA expressions, independent of plasmin activity. Treatment with atRA could be a promising intervention for kidney disease. Further studies are required to determine the atRA dose that is the most effective without causing harm.
Author contribution
Xia LIU, Lei LÜ, and Yi-chun ZHU designed research; Xia LIU and Lei LÜ performed research; Xia LIU, Lei LÜ, Bei-bei TAO, and Ai-ling ZHOU analyzed data; Xia LIU and Yi-chun ZHU wrote the paper.
Acknowledgments
This work was supported by grants from the Ministry of Science and Technology of China (No 2010CB912601, 2006CB503804, 2009ZX09303-006, 2009ZX09301-011), the National Natural Science Foundation of China (No 30825016, 30971064), the Science and Technology Commission of Shanghai Municipality (No 09XD1400400, 08JC1401400) and College Natural Science Research Foundation of Jiangsu Province (No 07KJD310171).
We would like to thank Dr Peter ROSE for critical comments regarding this manuscript.
References
- Remuzzi G, Bertani T. Pathophysiology of progressive nephropathies. N Engl J Med. 1998;339:1448–56. doi: 10.1056/NEJM199811123392007. [DOI] [PubMed] [Google Scholar]
- Birkedal-Hansen H. Proteolytic remodeling of extracellular matrix. Curr Opin Cell Biol. 1995;7:728–35. doi: 10.1016/0955-0674(95)80116-2. [DOI] [PubMed] [Google Scholar]
- Johnson RJ, Floege J, Yoshimura A, Iida H, Couser WG, Alpers CE. The activated mesangial cell: a glomerular “myofibroblast”. J Am Soc Nephrol. 1992;2:S190–7. doi: 10.1681/ASN.V210s190. [DOI] [PubMed] [Google Scholar]
- Zhang G, Moorhead PJ, el Nahas AM. Myofibroblasts and the progression of experimental glomerulonephritis. Exp Nephrol. 1995;3:308–18. [PubMed] [Google Scholar]
- Johnson RJ, Iida H, Alpers CE, Majesky MW, Schwartz SM, Pritzi P, et al. Expression of smooth muscle cell phenotype by rat mesangial cells in immune complex nephritis. Alpha-smooth muscle actin is a marker of mesangial cell proliferation. J Clin Invest. 1991;87:847–58. doi: 10.1172/JCI115089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muchaneta-Kubara EC, el Nahas AM. Myofibroblast phenotypes expression in experimental renal scarring. Nephrol Dial Transplant. 1997;12:904–15. doi: 10.1093/ndt/12.5.904. [DOI] [PubMed] [Google Scholar]
- Eddy AA. Plasminogen activator inhibitor-1 and the kidney. Am J Physiol Renal Physiol. 2002;283:F209–20. doi: 10.1152/ajprenal.00032.2002. [DOI] [PubMed] [Google Scholar]
- Eitzman DT, McCoy RD, Zheng X, Fay WP, Shen T, Ginsburg D, et al. Bleomycin-induced pulmonary fibrosis in transgenic mice that either lack or overexpress the murine plasminogen activator inhibitor-1 gene. J Clin Invest. 1996;97:232–7. doi: 10.1172/JCI118396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matsuo S, López-Guisa JM, Cai X, Okamura DM, Alpers CE, Bumgarner RE, et al. Multifunctionality of PAI-1 in fibrogenesis: evidence from obstructive nephropathy in PAI-1-overexpressing mice. Kidney Int. 2005;67:2221–38. doi: 10.1111/j.1523-1755.2005.00327.x. [DOI] [PubMed] [Google Scholar]
- Kitching AR, Kong YZ, Huang XR, Davenport P, Edgtton KL, Carmeliet P, et al. Plasminogen activator inhibitor-1 is a significant determinant of renal injury in experimental crescentic glomerulonephritis. J Am Soc Nephrol. 2003;14:1487–95. doi: 10.1097/01.asn.0000065550.13931.00. [DOI] [PubMed] [Google Scholar]
- Oda T, Jung YO, Kim HS, Cai X, López-Guisa JM, Ikeda Y, et al. PAI-1 deficiency attenuates the fibrogenic response to ureteral obstruction. Kidney Int. 2001;60:587–96. doi: 10.1046/j.1523-1755.2001.030002587.x. [DOI] [PubMed] [Google Scholar]
- Nicholas SB, Aguiniga E, Ren Y, Kim J, Wong J, Govindarajan N, et al. Plasminogen activator inhibitor-1 deficiency retards diabetic nephropathy. Kidney Int. 2005;67:1297–307. doi: 10.1111/j.1523-1755.2005.00207.x. [DOI] [PubMed] [Google Scholar]
- Ma J, Weisberg A, Griffin JP, Vaughan DE, Fogo AB, Brown NJ. Plasminogen activator inhibitor-1 deficiency protects against aldosterone-induced glomerular injury. Kidney Int. 2006;69:1064–72. doi: 10.1038/sj.ki.5000201. [DOI] [PubMed] [Google Scholar]
- Krag S, Danielsen CC, Carmeliet P, Nyengaard J, Wogensen L. Plasminogen activator inhibitor-1 gene deficiency attenuates TGF-beta1-induced kidney disease. Kidney Int. 2005;68:2651–66. doi: 10.1111/j.1523-1755.2005.00737.x. [DOI] [PubMed] [Google Scholar]
- Huang Y, Haraguchi M, Lawrence DA, Border WA, Yu L, Noble NA. A mutant, noninhibitory plasminogen activator inhibitor type 1 decreases matrix accumulation in experimental glomerulonephritis. J Clin Invest. 2003;112:379–88. doi: 10.1172/JCI18038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Omasu F, Oda T, Yamada M, Yoshizawa N, Yamakami K, Sakurai Y, et al. Effects of pioglitazone and candesartan on renal fibrosis and the intrarenal plasmin cascade in spontaneously hypercholesterolemic rats. Am J Physiol Renal Physiol. 2007;293:F1292–8. doi: 10.1152/ajprenal.00232.2007. [DOI] [PubMed] [Google Scholar]
- Heidland A, Sebekova K, Paczek L, Teschner M, Dämmrich J, Gaciong Z. Renal fibrosis: role of impaired proteolysis and potential therapeutic strategies. Kidney Int Suppl. 1997;62:S32, 5. [PubMed] [Google Scholar]
- Visse R, Nagase H. Matrix metalloproteinases and tissue inhibitors of metalloproteinases: structure, function, and biochemistry. Circ Res. 2003;92:827–39. doi: 10.1161/01.RES.0000070112.80711.3D. [DOI] [PubMed] [Google Scholar]
- Baricos WH, Cortez SL, el-Dahr SS, Schnaper HW. ECM degradation by cultured human mesangial cells is mediated by a PA/plasmin/MMP-2 cascade. Kidney Int. 1995;47:1039–47. doi: 10.1038/ki.1995.150. [DOI] [PubMed] [Google Scholar]
- Adams J, Kiss E, Arroyo AB, Bonrouhi M, Sun Q, Li Z, et al. 13-cis retinoic acid inhibits development and progression of chronic allograft nephropathy. Am J Pathol. 2005;167:285–98. doi: 10.1016/S0002-9440(10)62973-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han SY, So GA, Jee YH, Han KH, Kang YS, Kim HK, et al. Effect of retinoic acid in experimental diabetic nephropathy. Immunol Cell Biol. 2004;82:568–76. doi: 10.1111/j.1440-1711.2004.01287.x. [DOI] [PubMed] [Google Scholar]
- Schaier M, Jocks T, Grone HJ, Ritz E, Wagner J. Retinoid agonist isotretinoin ameliorates obstructive renal injury. J Urol. 2003;170:1398–402. doi: 10.1097/01.ju.0000084620.64255.b3. [DOI] [PubMed] [Google Scholar]
- Suzuki A, Ito T, Imai E, Yamato M, Iwatani H, Kawachi H, et al. Retinoids regulate the repairing process of the podocytes in puromycin aminonucleoside-induced nephrotic rats. J Am Soc Nephrol. 2003;14:981–91. doi: 10.1097/01.asn.0000057857.66268.8f. [DOI] [PubMed] [Google Scholar]
- Vaughan MR, Pippin JW, Griffin SV, Krofft R, Fleet M, Haseley L, et al. ATRA induces podocyte differentiation and alters nephrin and podocin expression in vitro and in vivo. Kidney Int. 2005;68:133–44. doi: 10.1111/j.1523-1755.2005.00387.x. [DOI] [PubMed] [Google Scholar]
- Wagner J, Dechow C, Morath C, Lehrke I, Amann K, Waldherr R, et al. Retinoic acid reduces glomerular injury in a rat model of glomerular damage. J Am Soc Nephrol. 2000;11:1479–87. doi: 10.1681/ASN.V1181479. [DOI] [PubMed] [Google Scholar]
- Dechow C, Morath C, Peters J, Lehrke I, Waldherr R, Haxsen V, et al. Effects of all-trans retinoic acid on renin-angiotensin system in rats with experimental nephritis. Am J Physiol Renal Physiol. 2001;281:F909–19. doi: 10.1152/ajprenal.2001.281.5.F909. [DOI] [PubMed] [Google Scholar]
- Morath C, Ratzlaff K, Dechow C, Schwenger V, Schaier M, Zeier B, et al. Chronic low-dose isotretinoin treatment limits renal damage in subtotally nephrectomized rats. J Mol Med. 2009;87:53–64. doi: 10.1007/s00109-008-0404-5. [DOI] [PubMed] [Google Scholar]
- Morath C, Dechow C, Lehrke I, Haxsen V, Waldherr R, Floege J, et al. Effects of retinoids on the TGF-beta system and extracellular matrix in experimental glomerulonephritis. J Am Soc Nephrol. 2001;12:2300–9. doi: 10.1681/ASN.V12112300. [DOI] [PubMed] [Google Scholar]
- Lü L, Yao T, Zhu YZ, Huang GY, Cao YX, Zhu YC. Chronic all-trans retinoic acid treatment prevents medial thickening of intramyocardial and intrarenal arteries in spontaneously hypertensive rats. Am J Physiol Heart Circ Physiol. 2003;285:H1370–7. doi: 10.1152/ajpheart.00260.2003. [DOI] [PubMed] [Google Scholar]
- Liu X, Lü L, Tao BB, Zhu YC. All-trans retinoic acid inhibits the increases in fibronectin and PAI-1 induced by TGF-beta1 and Ang II in rat mesangial cells. Acta Pharmacol Sin. 2008;29:1035–41. doi: 10.1111/j.1745-7254.2008.00849.x. [DOI] [PubMed] [Google Scholar]
- Raij L, Azar S, Keane W. Mesangial immune injury, hypertension, and progressive glomerular damage in Dahl rats. Kidney Int. 1984;26:137–43. doi: 10.1038/ki.1984.147. [DOI] [PubMed] [Google Scholar]
- Griffin KA, Picken MM, Churchill M, Churchill P, Bidani AK. Functional and structural correlates of glomerulosclerosis after renal mass reduction in the rat. J Am Soc Nephrol. 2000;11:497–506. doi: 10.1681/ASN.V113497. [DOI] [PubMed] [Google Scholar]
- Gonçalves AR, Fujihara CK, Mattar AL, Malheiros DM, Noronha Ide L, de Nucci G, et al. Renal expression of COX-2, ANG II, and AT1 receptor in remnant kidney: strong renoprotection by therapy with losartan and a nonsteroidal anti-inflammatory. Am J Physiol Renal Physiol. 2004;286:F945–54. doi: 10.1152/ajprenal.00238.2003. [DOI] [PubMed] [Google Scholar]
- Ljutić D, Kes P. The role of arterial hypertension in the progression of non-diabetic glomerular diseases. Nephrol Dial Transplant. 2003;18:v28–30. doi: 10.1093/ndt/gfg1040. [DOI] [PubMed] [Google Scholar]
- Mayer G, Lafayette RA, Oliver J, Deen WM, Myers BD, Meyer TW. Effects of angiotensin II receptor blockade on remnant glomerular permselectivity. Kidney Int. 1993;43:346–53. doi: 10.1038/ki.1993.52. [DOI] [PubMed] [Google Scholar]
- Pavenstädt H, Kriz W, Kretzler M. Cell biology of the glomerular podocyte. Physiol Rev. 2003;83:253–307. doi: 10.1152/physrev.00020.2002. [DOI] [PubMed] [Google Scholar]
- Shankland SJ. The podocyte's response to injury: role in proteinuria and glomerulosclerosis. Kidney Int. 2006;69:2131–47. doi: 10.1038/sj.ki.5000410. [DOI] [PubMed] [Google Scholar]
- Zoja C, Benigni A, Remuzzi G. Cellular responses to protein overload: key event in renal disease progression. Curr Opin Nephrol Hypertens. 2004;13:31–7. doi: 10.1097/00041552-200401000-00005. [DOI] [PubMed] [Google Scholar]
- Lee LK, Meyer TW, Pollock AS, Lovett DH. Endothelial cell injury initiates glomerular sclerosis in the rat remnant kidney. J Clin Invest. 1995;96:953–64. doi: 10.1172/JCI118143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raffo P, Emionite L, Colucci L, Belmondo F, Moro MG, Bollag W, et al. Retinoid receptors: pathways of proliferation inhibition and apoptosis induction in breast cancer cell lines. Anticancer Res. 2000;20:1535–43. [PubMed] [Google Scholar]
- Hansen LA, Sigman CC, Andreola F, Ross SA, Kelloff GJ, De Luca LM. Retinoids in chemoprevention and differentiation therapy. Carcinogenesis. 2000;21:1271–9. [PubMed] [Google Scholar]
- Simonson MS. Anti-AP-1 activity of all-trans retinoic acid in glomerular mesangial cells. Am J Physiol. 1994;267:F805–15. doi: 10.1152/ajprenal.1994.267.5.F805. [DOI] [PubMed] [Google Scholar]
- Haxsen V, Adam-Stitah S, Ritz E, Wagner J. Retinoids inhibit the actions of angiotensin II on vascular smooth muscle cells. Circ Res. 2001;88:637–44. doi: 10.1161/01.res.88.6.637. [DOI] [PubMed] [Google Scholar]
- Miano JM, Kelly LA, Artacho CA, Nuckolls TA, Piantedosi R, Blaner WS. All-trans-retinoic acid reduces neointimal formation and promotes favorable geometric remodeling of the rat carotid artery after balloon withdrawal injury. Circulation. 1998;98:1219–27. doi: 10.1161/01.cir.98.12.1219. [DOI] [PubMed] [Google Scholar]
- Wen X, Li Y, Hu K, Dai C, Liu Y. Hepatocyte growth factor receptor signaling mediates the anti-fibrotic action of 9-cis-retinoic acid in glomerular mesangial cells. Am J Pathol. 2005;167:947–57. doi: 10.1016/S0002-9440(10)61185-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haraguchi M, Border WA, Huang Y, Noble NA. t-PA promotes glomerular plasmin generation and matrix degradation in experimental glomerulonephritis. Kidney Int. 2001;59:2146–55. doi: 10.1046/j.1523-1755.2001.00729.x. [DOI] [PubMed] [Google Scholar]
- Kitching AR, Holdsworth SR, Ploplis VA, Plow EF, Collen D, Carmeliet P, et al. Plasminogen and plasminogen activators protect against renal injury in crescentic glomerulonephritis. J Exp Med. 1997;185:963–8. doi: 10.1084/jem.185.5.963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang J, Shultz RW, Mars WM, Wegner RE, Li Y, Dai C, et al. Disruption of tissue-type plasminogen activator gene in mice reduces renal interstitial fibrosis in obstructive nephropathy. J Clin Invest. 2002;110:1525–38. doi: 10.1172/JCI16219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edgtton KL, Gow RM, Kelly DJ, Carmeliet P, Kitching AR. Plasmin is not protective in experimental renal interstitial fibrosis. Kidney Int. 2004;66:68–76. doi: 10.1111/j.1523-1755.2004.00707.x. [DOI] [PubMed] [Google Scholar]
- Turck J, Pollock AS, Lee LK, Marti HP, Lovett DH. Matrix metalloproteinase 2 (gelatinase A) regulates glomerular mesangial cell proliferation and differentiation. J Biol Chem. 1996;271:15074–83. doi: 10.1074/jbc.271.25.15074. [DOI] [PubMed] [Google Scholar]
- Cheng S, Lovett DH. Gelatinase A (MMP-2) is necessary and sufficient for renal tubular cell epithelial-mesenchymal transformation. Am J Pathol. 2003;162:1937–49. doi: 10.1016/S0002-9440(10)64327-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang G, Kernan KA, Collins SJ, Cai X, López-Guisa JM, Degen JL, et al. Plasmin(ogen) promotes renal interstitial fibrosis by promoting epithelial-to-mesenchymal transition: role of plasmin-activated signals. J Am Soc Nephrol. 2007;18:846–59. doi: 10.1681/ASN.2006080886. [DOI] [PubMed] [Google Scholar]
- Ploplis VA, French EL, Carmeliet P, Collen D, Plow EF. Plasminogen deficiency differentially affects recruitment of inflammatory cell populations in mice. Blood. 1998;91:2005–9. [PubMed] [Google Scholar]
- Border WA, Noble N. Maximizing hemodynamic-independent effects of angiotensin II antagonists in fibrotic diseases. Semin Nephrol. 2001;21:563–72. doi: 10.1053/snep.2001.26795. [DOI] [PubMed] [Google Scholar]
- Gagliardini E, Benigni A. Therapeutic potential of TGF-beta inhibition in chronic renal failure. Expert Opin Biol Ther. 2007;7:293–304. doi: 10.1517/14712598.7.3.293. [DOI] [PubMed] [Google Scholar]
- Wolf G. Link between angiotensin II and TGF-beta in the kidney. Miner Electrolyte Metab. 1998;24:174–80. doi: 10.1159/000057367. [DOI] [PubMed] [Google Scholar]