Abstract
The quality of life (QoL) of short children is an important issue that has been studied in Western countries, but not fully in Japan. We assessed the psychosocial profiles of Japanese children with short stature using the Japanese version of the Child Behavior Checklist (CBCL). A higher score in the CBCL means a lower QoL. A total of 116 children with idiopathic short stature (ISS) and 127 children with GH deficiency (GHD), aged 4 to 15 yr, were enrolled in the study. The total CBCL scores of the children in the GHD/ISS group were found to be higher than those of the normal children group. The QoL subscales for social problems and attention problems of the young (4–11 yr) children in the GHD/ISS group were significantly higher than those of the group of children of normal height. The proportion of children with GHD/ISS classified into the borderline/abnormal range was significantly higher than that of normal children. Children with ISS tended to have higher total scores and more subscale problems, and a greater proportion of these children was classified in the borderline/abnormal range than the children with GHD, although the difference was not significant. These results suggest that QoL is impaired in Japanese children due to short stature.
Keywords: GH deficiency, idiopathic short stature, quality of life
Introduction
It has been suggested that many short children suffer from psychosocial problems. The short-term goals of GH therapy in short children with GH deficiency (GHD) are to increase their heights into the normal range and to attenuate psychosocial problems caused by short stature. The long-term goals are achievement of normal adult height and adaptation into normal social life. Therefore, assessment of psychosocial problems is important to evaluate the effect of GH therapy in children.
Several studies have pointed out behavioral problems, social immaturity, lower self-esteem and infantilization of children with short stature (1,2,3,4). On the other hand, some studies have reported that children with GHD had no psychosocial problems despite the stress caused by short stature (2, 5, 6). Due to the different methodologies used to evaluate psychosocial problems, evaluation of psychological problems and quality of life (QoL) in short children is still controversial.
Stabler et al. (7) estimated the QoL of children with idiopathic short stature (ISS) and GHD using the Child Behavior Checklist (CBCL) and followed the scores of children with GHD during GH therapy. QoL was impaired in both children with ISS and GHD, and it was improved by GH therapy in children with GHD. In the present study, we assessed QoL in Japanese children with short stature using the Japanese version of the CBCL (8) and compared the results with those of children of normal height.
Subjects and Methods
Subjects
The Genetics and Neuroendocrinology of Short Stature International Study (GeNeSIS) is an open-label, multicenter, multinational, observational study established as a post-marketing research program to evaluate the long-term efficacy and safety of Humatrope GH products (Eli Lilly and Company, Indianapolis, IN, USA). GeNeSIS complies with the requirements of post-marketing surveillance studies as stated in the guidelines provided by various national and international bodies (9, 10). AS GeNeSIS is a post-marketing research program, data is collected only as provided by attending physicians. Because no worldwide consensus guidelines for post-marketing surveillance studies exist, it is the responsibility of the local affiliates of Eli Lilly And Company to ensure that data collection and handling comply with national and regional regulatory requirements. Informed consent is required for QOL study, and permission is required for anonymous use of the data in compliance with rigorous privacy guidelines.
One hundred and twenty-seven Japanese children with GHD (73 boys and 54 girls), naive to GH treatment, were selected from the GeNeSIS Eli Lilly & Co. post-marketing safety observational study. One hundred and sixteen children with ISS (63 boys and 53 girls) were recruited from 17 hospitals participating in GeNeSIS. The inclusion criteria for study participation were 1) age 4–15 yr, 2) height SDS below –2.0, 3) diagnosis of GHD or ISS and 4) use of Japanese as their primary language. Subjects were classified as having GHD when the peak GH responses to two or more provocation tests were <10 ng/mL and were classified as having ISS when the peak GH exceeded 10 ng/mL and when no cause for their short stature (e.g., GHD, Turner syndrome, achondroplasia or chronic renal failure) could be determined. ISS includes short children who did not undergo complete evaluation for GH stimulation tests.
Psychosocial test procedures
The Japanese version of the CBCL/4-18 was used to assess the children’s behavior. The CBCL is a widely used parent-report measure of psychosocial profile in children with somatic and psychiatric diseases, as well as in healthy children of normal height. The checklist consists of 118 questions with multiple choices and yields a total score and two broad-band scores representing externalizing and internalizing dimensions of behavior and emotional problems. In addition, the questions are classified into eight narrow-band subscales (withdrawn/depressed behavior, somatic complaints, social problems, anxiety/depression, thought problems, attention problems, rule-breaking behavior, and aggressive behavior).
The primary caregivers(s) of GHD children completed the CBCL after diagnosis as baseline data. The baseline scores for children with GHD or ISS obtained in the present survey were compared with those of children of normal height (by age-group), as reported by Kambayashi et al. (8).
The results of the CBCL are reported as T-scores. A T-score is a standardized value based on the percentile scores obtained from investigation of normal reference Japanese children. The scoring range is from 0 to 100, and lower scores indicate superior functioning. A T-score of 59 (84th percentile) or lower is classified into the normal range, a T-score between 60-63 (85th-90th percentile) is classified into the borderline range and a T-score of 64 (91st percentile) or higher is classified into the abnormal range.
Statistical analysis
The baseline characteristics of children with GHD and ISS were summarized for each group. For continuous variables, mean and standard deviation were calculated, and group differences were tested by the two-sided t-test. For categorical variables, count and percentage were tabulated for each category, and group differences were tested by the chi-square test. Pair-wise comparison of the CBCL scores at baseline between children with GHD or ISS and children of normal height was performed using the two-sided t-test. The proportional differences between children with GHD/ISS and children of normal height classified in the borderline/abnormal range were assessed using the chi-square test. All statistical analysis tests were evaluated at a two-sided significance level of 0.05. Adjustments for multiple comparisons were not performed. Statistical Analysis System (SAS) version 8.02 was used as the statistical software to conduct the analyses.
Results
Background characteristics
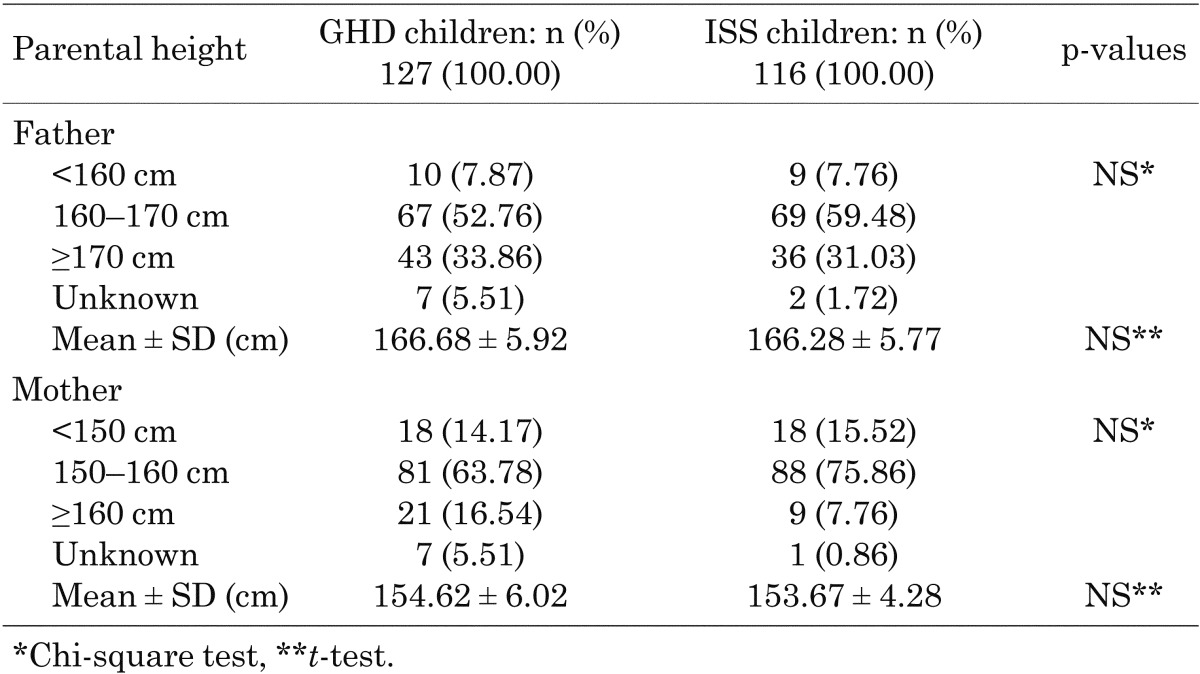
The baseline characteristics of children with GHD and ISS are summarized in Table 1. The two groups did not significantly differ in sex, weight or height. The means of the GHD group were not significantly higher than those of the ISS group. However, the percentage of 12–15 yr old in the GHD group was significantly higher than in the ISS group (p<0.01) and the mean height SD score of the GHD group was significantly lower (p<0.0001). Detailed paarental height data are provided in Table 2. The ISS and GHD groups did not significantly differ in terms of parental height.
Table 1. The baseline characteristics of the GHD and ISS children.
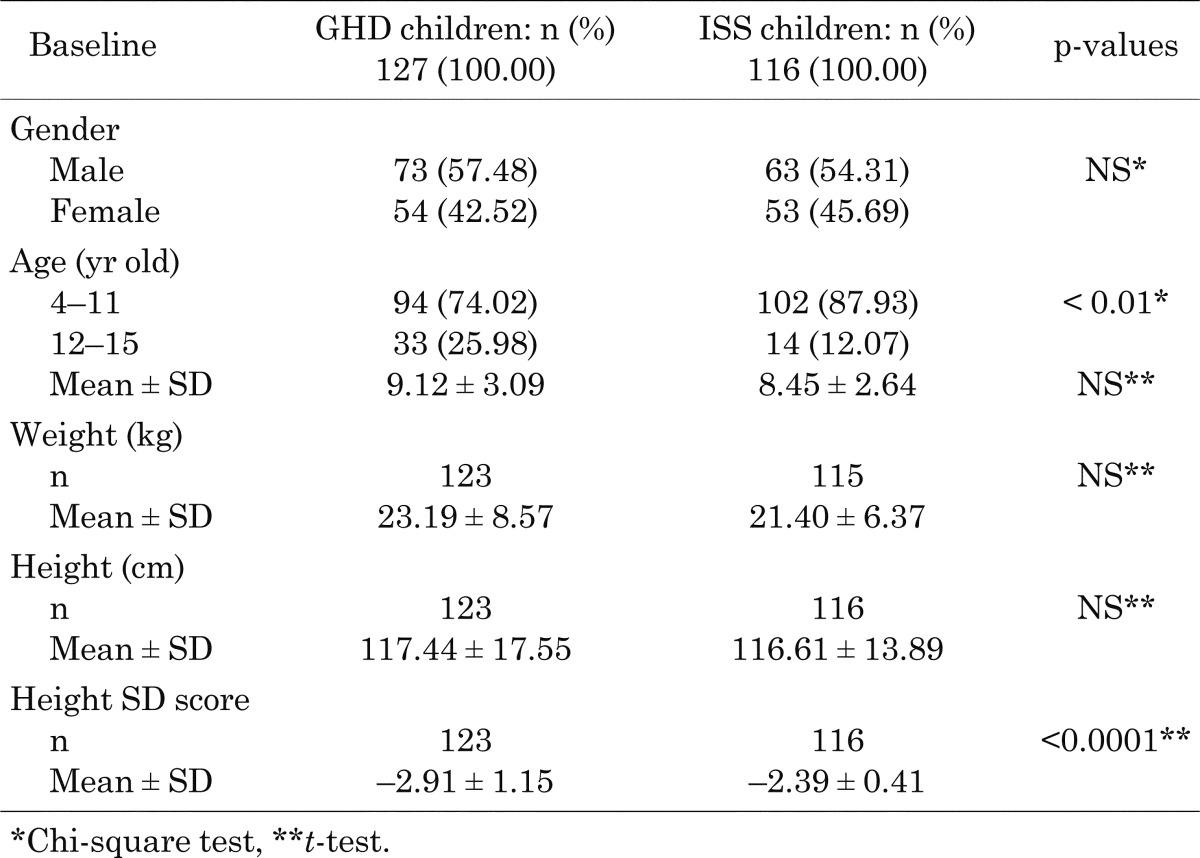
Table 2. Parental height data of the GHD and ISS children.
The CBCL score
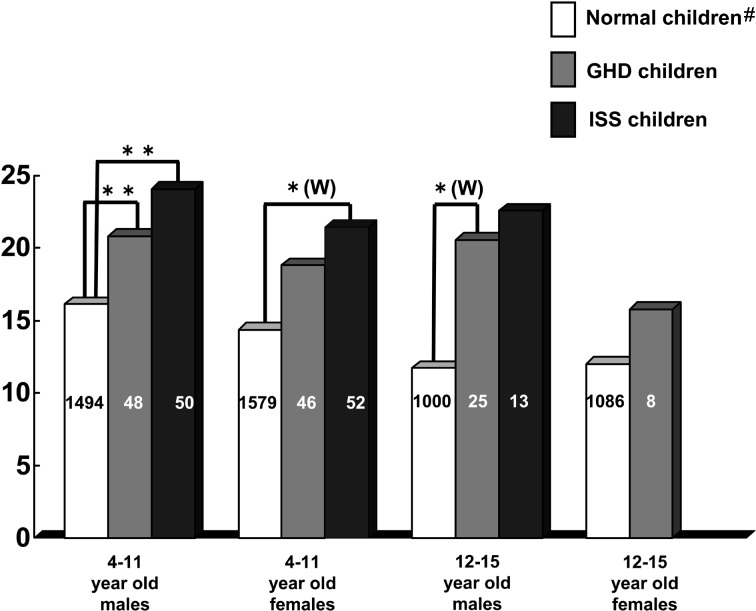
Table 3 shows the CBCL sub-scale scores for normal children and GHD/ISS children at baseline. As shown in Fig. 1, the total CBCL scores at baseline of the children in the GHD group were higher than those of the children in the normal height group. Those differences were significant in boys with GHD aged 4 to 11 yr (p<0.001) and 12 to 15 yr (p<0.05). In girls with GHD, the difference did not reach significance.
Table 3. CBCL subscale scores for normal children and the GHD/ISS children at baseline.
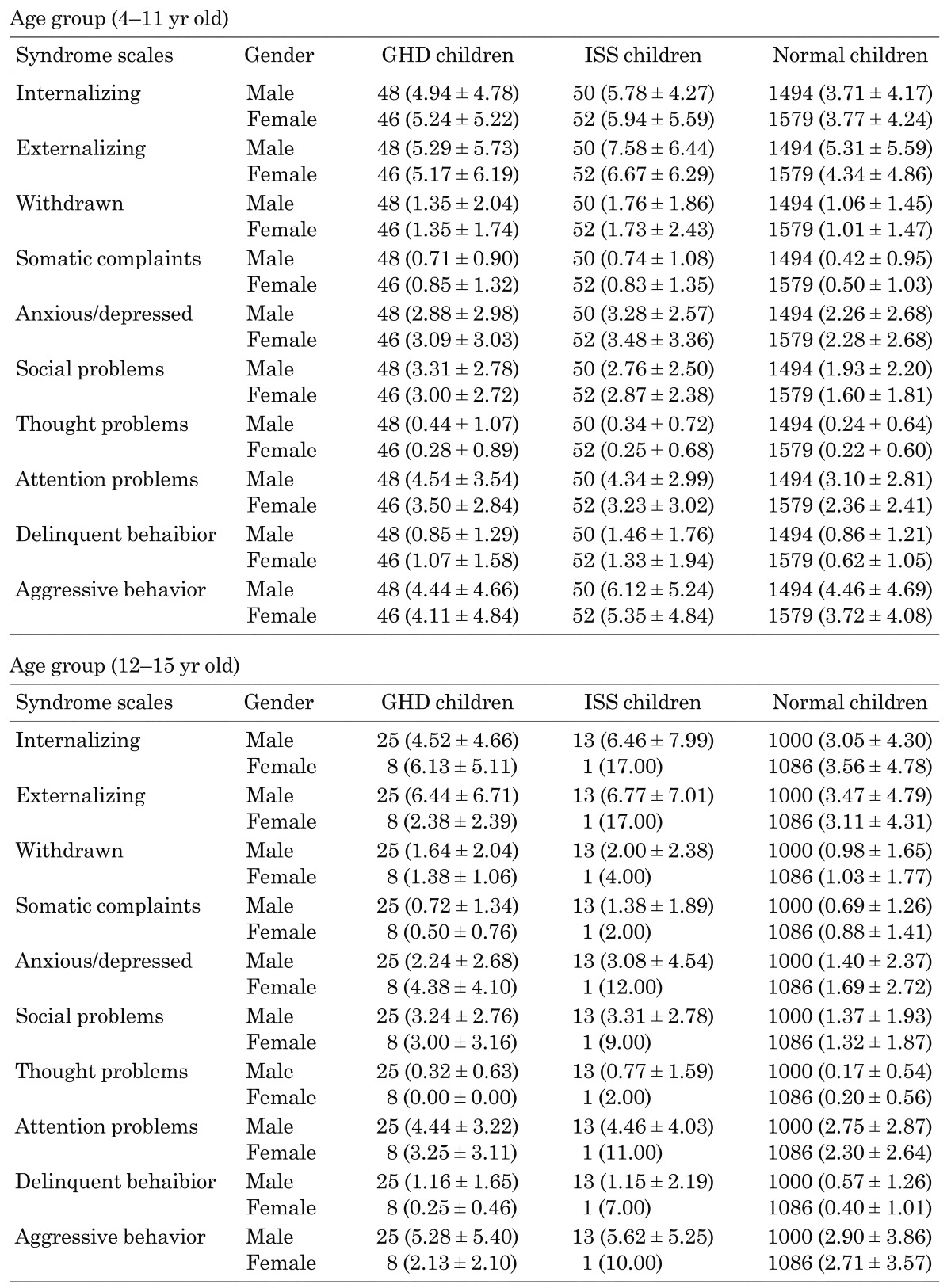
Fig. 1.
Total score of CBCL at baseline. *p<0.05, **p<0.001. (W): Welch, Other: t-test. #Kanbayashi, Standardization of the Japanese version of the Child Behavior Checklist/4-18, Japanese Society Pediatric Psychiatry and Neurology, 2001, 41,1,243-52.
In the subscales, parental ratings of behavioral problems on the CBCL were significantly higher for children with GHD aged 4 to 11 yr (as compared with normal children) in relation to anxious/depressed behavior, social problems and attention problems scales both in both boys and girls (Table 4). In boys with GHD, the somatic complaints scale difference was also significant.
Table 4. Behavioral problems on the CBCL that showed significant differences between normal and GHD/ISS children.
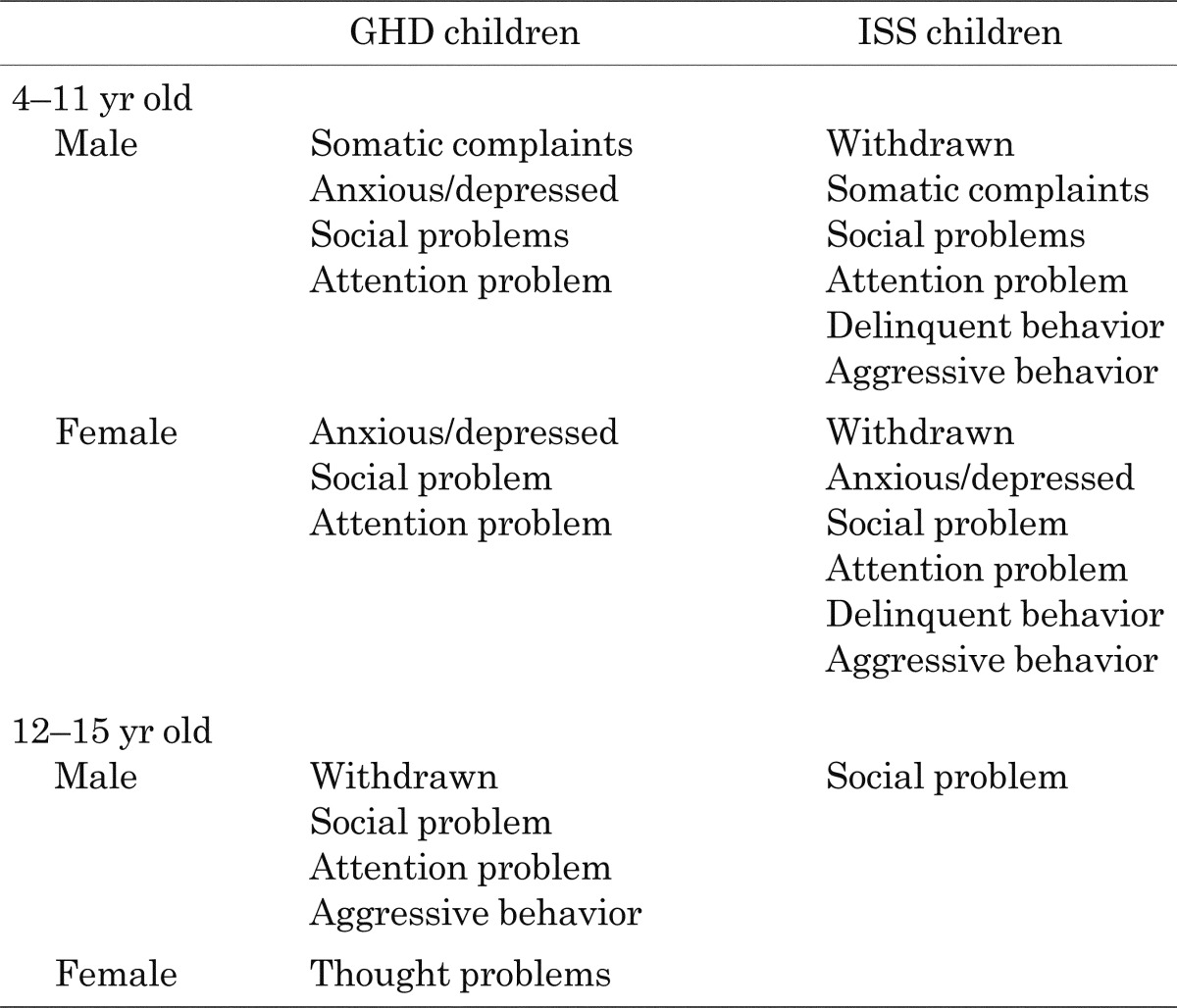
The total CBCL score in children with ISS was also higher than in normal children. Those differences were significantly higher in both male and female children with ISS aged 4 to 11 yr than in the normal children group (boys p<0.001, girls p<0.05; Fig. 1); the total score of the 12 to 15 yr-old group was also higher than that of the normal children group, although this difference was not statistically significant.
The subscale scores of children with ISS aged 4 to 11 yr for withdrawn behavior, social problems, attention problems, delinquent behavior and aggressive behavior were significantly higher than those of the normal children group. The scores for the somatic complaints scale of boys and the anxious/depressed behavior scale of girls were also significantly higher (Table 4).
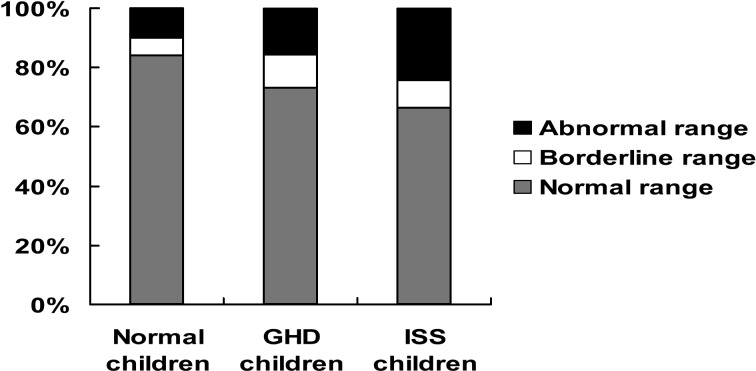
The proportions of children in the borderline/abnormal ranges
Children with T-scores between 60 and 63 (equivalent to the 85th to 90th percentile) were classified into the ‘borderline’ group; children with T-scores over 64 (>91st percentile) were classified into the ‘abnormal’ group.
The baseline scores showed that 26.1% of the children with GHD and 33.6% of the children with ISS were classified in the borderline or abnormal ranges, and it was shown that in both groups these proportions were significantly higher compared with children of normal height (p<0.01; Fig. 2). No significant difference in proportion was found between the children with GHD and the children with ISS.
Fig. 2.
The proportions of children in the borderline/abnormal ranges in GHD/ISS children. Significant difference between normal children and GHD/ISS children in their borderline/abnormal ranges (p<0.01).
Discussion
In Japan, no appropriate method exists for evaluation of the psychosocial problems or QoL of short children. The CBCL has been widely used to assess the psychosocial profiles of children with somatic and psychiatric diseases (11). Because the CBCL was evaluated for normal Japanese children, and therefore standardized for Japanese children with diseases (8), we used it to assess the QoL of short children.
Our study demonstrated that the total score on the CBCL was higher in children with ISS and GHD than in normal children. Although the difference was not statistically significant in some age and sex groups, it may become significant by increasing the number of subjects. These results demonstrate that the QoL of children with ISS and GHD is impaired compared with children of normal height. Our data are comparable with that of Stabler et al. (7), who showed an impaired QoL as estimated by the CBCL in short children with GHD and ISS. The mean total score tended to be higher in the ISS groups than in the GHD groups for all age groups except the oldest (12–15 yr) female group, although the difference between them was not significant.
The present study has several limitations. First, the subjects of this study were only short children who visited GeNeSIS-enrolled medical institutions. Furthermore, the QoL of the GHD children was assessed by the parent(s) after diagnosis in the present study. Therefore, the results might be slightly different from the results of short children who do not visit hospitals and GHD children who have not been diagnosed yet.
In the study by Stabler et al. (7), all the behavioral adjustment subscale raw scores were significantly higher in the GHD and ISS groups than in children of normal height, indicating more problems in short children. Similarly, many of the subscale raw scores were also significantly higher for short children in the present study. Specifically, the raw scores for the young (4–11 yr) ISS group in six subscales were significantly higher than those in children of normal height, whereas the raw scores in three or four subscales were significantly higher in the young GHD group than in children of normal height. These results also suggest that children with ISS have more problems than children with GHD.
Among subscales with higher raw scores, the subscales of social and attention problems were the most common problems in both the young GHD and young ISS groups compared with children of normal height. Withdrawn and externalizing subscales of aggressive behavior and delinquent behavior were characteristic of only the young ISS group. In older short children, children with GHD showed more problems in subscales than children with ISS, but the numbers of the older patients were insufficient to draw conclusions. It is of interest that children with ISS seemed to have more problems than children with GHD, as estimated by parents. The reasons for this tendency are unclear. The parents of children with GHD and children with ISS might feel differently regarding height outcome expectations because children with GHD will receive GH treatment; differing height outcome expectations might influence the CBCL estimation.
When the proportions of the borderline/abnormal range classifications were compared after T-score transformation, the ranges were significantly greater in children with GHD and ISS than in children of normal height. This result also demonstrates that more short children suffer from impaired QoL than children of normal height. A greater percentage of children with ISS classified in the normal range suggests that more children with ISS suffer from impaired QoL than children with GHD.
The present study demonstrated that children with GHD and ISS, at least those who visited hospitals complaining of short stature, had an impaired QoL. To confirm that short stature influences the CBCL score, it is necessary to analyze the relation between CBCL scores and height SDS; this analysis is currently being conducted. Furthermore, it would be interesting to determine whether GH treatment for GHD or ISS improves QoL in Japanese children. A trial is now being conducted in children with GHD to investigate the effect of GH treatment on CBCL scores.
References
- 1.Pollitt E, Money J. Studies in the psychology of dwarf. I. Intelligence quotient and school achievement. J Pediatr 1964;64: 415–21 doi: 10.1016/S0022-3476(64)80194-3 [DOI] [PubMed] [Google Scholar]
- 2.Steinhausen HC, Stahnke N. Psycholoendocrinological studies in dwarfed children and adolescents. Arch Dis Child 1976;51: 778–83 doi: 10.1136/adc.51.10.778 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Frisch H, Hausler G, Lindenbauer S, Singer S. Psychological aspects in children and adolescents with hypopituitarism. Acta Paediatr Scand 1990;79: 644–51 doi: 10.1111/j.1651-2227.1990.tb11529.x [DOI] [PubMed] [Google Scholar]
- 4.Stabler B, Clopper RR, Siegel PT, Stoppani C, Compton PG, Underwood LE. Academic achievement and psychological adjustment in short children. The National Cooperative Growth Study. J Dev Behav Pediatr 1994;15: 1–6 doi: 10.1097/00004703-199402000-00001 [DOI] [PubMed] [Google Scholar]
- 5.Steinhausen HC, Stahnke N. Negative impact of growth-hormone deficiency on psychological functioning in dwarfed children and adolescents. Eur J Pediatr 1977;126: 263–70 doi: 10.1007/BF00477052 [DOI] [PubMed] [Google Scholar]
- 6.Steinhausen HC, Dorr HG, Kannenberg R, Malin Z. The behavior profile of children and adolescents with short stature. J Dev Behav Pediatr 2000;21: 423–8 doi: 10.1097/00004703-200012000-00004 [DOI] [PubMed] [Google Scholar]
- 7.Stabler B, Siegel PT, Clopper RR, Stoppani CE, Compton PG, Underwood LE. Behavior change after growth hormone treatment of children with short stature. J Pediatr 1998;133: 366–73 doi: 10.1016/S0022-3476(98)70271-9 [DOI] [PubMed] [Google Scholar]
- 8.Itani T, Kanbayashi Y, Nakata Y, Kita M, Fujii H, Kuramoto H, et al. Standardization of the Japanese version of the Child Behavior Checklist/4-18. Psychiatr Neurol Pediatr Jpn 2001;41: 243–52 [Google Scholar]
- 9.Linden M, Baier D, Beitinger H, Kohnen R, Osterheider M, Philipp M, et al. Guidelines for the implementation of drug utilization observation (DUO) studies in psychopharmacological therapy. Pharmacopsychiat (Suppl) 1996;29: 1–6 [DOI] [PubMed] [Google Scholar]
- 10.Herbold M. International guidelines on post-authorization research and surveillance. Pharmacopsychiat (Suppl) 1997;30: 62–4. doi: 10.1055/s-2007-979519 [DOI] [PubMed] [Google Scholar]
- 11.Achenbach TM, Ruffle TM. The child behavior checklist and related form for assessing behavioral/emotional problems and competencies. Pediatr Rev 2000;21: 265–71 doi: 10.1542/pir.21-8-265 [DOI] [PubMed] [Google Scholar]