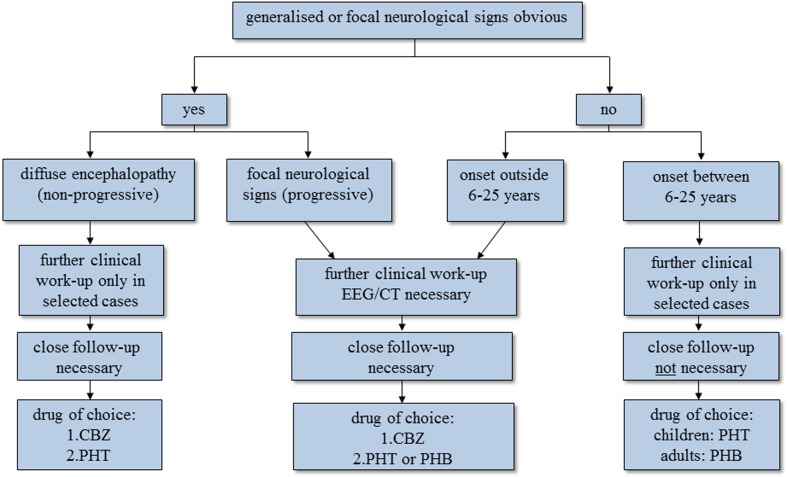
Figure 2.
Algorithm on how to classify people with epilepsy/epileptic seizures in resource-poor countries with diagnostic and therapeutic implications. The first question one has to ask is whether there is any evidence of focal neurological signs or even more widespread encephalopathy. If there is, the approach in the two groups is different. In most people, mainly children, with epilepsy with diffuse encephalopathy, diagnostic tests are rarely needed as the extent of the cerebral sequelae is known and the condition is not progressive. In contrast, in people with epilepsy who show focal signs without diffuse encephalopathy further diagnostic steps are essential in order to identify the underlying, potentially treatable cause. If neurological examination is unremarkable, the so-called primary generalised seizures are split according to the age of onset (see text); the two groups have a different diagnostic and therapeutic approach. Patients with primary generalised seizures that start outside 6–25 years are more likely to have cerebral lesions compared to those with seizures that start within the range of 6–25 years, where genetically determined epilepsy prevails. The former therefore need further investigation. In all four groups, treatment depends mainly on the age of the patient, seizure activity, seizure frequency, the presence of mental handicap and the presence of focal neurological signs, bearing in mind that the choice of antiepileptic medication is limited. People with epilepsy/epileptic seizures due to NCC can potentially be found in all four groups, but are mainly seen in patients with generalised late-onset seizures or in patients with generalised seizures and focal neurological signs without major encephalopathy. For further explanations refer to the main text. CBZ = carbamazepine, PHT = phenytoin, PHB = phenobarbitone.