Abstract
OBJECTIVES:
To evaluate the effectiveness of an educational intervention to decrease pediatric emergency department (PED) visits and adverse care practices for upper respiratory infections (URI) among predominantly Latino Early Head Start (EHS) families.
METHODS:
Four EHS sites in New York City were randomized. Families at intervention sites received 3 1.5-hour education modules in their EHS parent-child group focusing on URIs, over-the-counter medications, and medication management. Standard curriculum families received the standard EHS curriculum, which did not include URI education. During weekly telephone calls for 5 months, families reported URI in family members, care sought, and medications given. Pre- and post-intervention knowledge-attitude surveys were also conducted. Outcomes were compared between groups.
RESULTS:
There were 154 families who participated (76 intervention, 78 standard curriculum) including 197 children <4 years old. Families were primarily Latino and Spanish-speaking. Intervention families were significantly less likely to visit the PED when their young child (age 6 to <48 months) was ill (8.2% vs 15.7%; P = .025). The difference remained significant on the family level (P = .03). These families were also less likely to use an inappropriate over-the-counter medication for their <2-year-old child (odds ratio, 0.29; 95% confidence interval, 0.09–0.95; 12.2% vs 32.4%, P = .034) and/or incorrect dosing tool for their <4-year-old child (odds ratio, 0.24; 95% confidence interval, 0.08–0.74; 9.8% vs 31.1%; P < .01). The mean difference in Knowledge-Attitude scores for intervention families was higher.
CONCLUSIONS:
A URI health literacy-related educational intervention embedded into EHS decreased PED visits and adverse care practices.
Keywords: health literacy, upper respiratory infections, Early Head Start
What’s Known on This Subject:
Young children have multiple upper respiratory infections (URI) annually. Limited health literacy regarding URI can place families at risk for emergency department (ED) visits, inappropriate use of over-the-counter medications, and medication measurement errors.
What This Study Adds:
Few educational interventions for URI have targeted groups with limited health literacy. Integrating an educational intervention into Early Head Start is a novel approach to increasing parental health literacy regarding URI and decreasing ED visits, with potential for wide dissemination.
Young children, especially in day care and early school settings, have multiple episodes of upper respiratory infections (URI).1–4 Lack of knowledge about causes and medically appropriate treatment of URIs among parents and caregivers5–8 has been linked to increased health service use, including pediatric emergency department (PED) visits8–10 and adverse care practices such as inappropriate use of over-the-counter (OTC) cough and cold medications and/or home remedies in young children,11–15 medication dosing errors,16 and antibiotic seeking.8,9,17
Limited health literacy affects over 90 million Americans18 and is especially prevalent in low-income households and among minorities and people with limited English proficiency.19 Latino parents have been shown to be at high risk for limited health literacy in general19 and regarding URIs specifically.7,20–22 They are also at higher risk for believing antibiotics are needed for URI and for using OTC medications and home remedies for young children.13,15,20,21,23
Previous studies have found mixed impacts of educational efforts directed at care for URIs.24–29 These studies were primarily conducted in practice settings with predominately non-minority populations. The Institute of Medicine recommends embedding health literacy-promoting educational programs into existing curricula of community programs,18 and the Centers for Disease Control and Prevention promotes using such programs for URI-related health literacy interventions.30 Early Head Start (EHS) is a federally supported community-based program for low-income infants, toddlers, and pregnant women; parent health education is an important part.31 Nearly 175 000 children nationally are in EHS, and nearly 40% are Latino. Thus, EHS may be a potentially effective venue for URI educational interventions.31–33 We conducted a randomized study of an educational intervention to increase health literacy regarding URI, with the goals of decreased PED visits and improved care practices among EHS families in a predominately Latino community.
Methods
Setting and Subjects
The study took place in 2009 to 2010 in 4 EHS sites, 2 affiliated with the Children’s Aid Society and 2 with Columbia University. These programs are the principal providers of EHS services in the Washington Heights/Inwood section of northern Manhattan, New York City.
To minimize spillover effects from having intervention and nonintervention families at the same sites, 1 site from each program was randomly chosen as intervention sites, the remaining as “standard curriculum.” Families were identified by EHS staff based on class rosters and were eligible if they were attending an infant or toddler group in September 2009. Families were ineligible if they were part of a small pilot study of this intervention33 or another community URI-related intervention34 (Fig 1). The study was approved by Columbia University’s Institutional Review Board, and families gave written informed consent.
FIGURE 1.
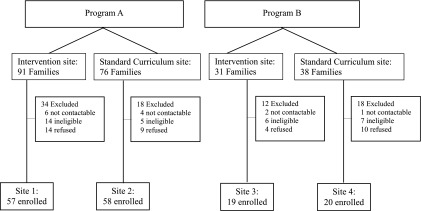
Enrollment flow.
Intervention
In fall 2009 at the intervention sites, three 1.5-hour education modules were provided to whichever parent/caregiver attended EHS as part of their regular curriculum in their EHS parent-child group.35 Classes were taught by trained Latina community health workers hired for the study, and were conducted in English or Spanish, based on class preference. The first module focused on viral versus bacterial infections, URI versus influenza (seasonal and 2009 H1N1), influenza vaccination, antibiotic resistance, and when/where a family should seek care.35,36 Parents were also given and taught how to use a URI care kit, including a URI “prescription,” digital thermometer, nasal saline and bulb suction, oral syringe for medication dosing, tissues, and hand sanitizer. The “prescription” was written suggestions for URI care, such as using a humidifier or elevating the head of the bed. The second module focused on OTC medications and common home remedies for that community (eg, sancochito) with a safety emphasis.37 The third concentrated on how to measure medications, read prescription labels, and prepare for medical visits. The previous session’s material was reviewed at the beginning of the next session. During the same time period, parents at the standard curriculum sites received the usual EHS curriculum, which did not include URI health literacy education. These families received the URI health literacy curriculum in spring 2010, after study completion. All EHS parents, including ineligible and non-enrollees, also received the classes within their EHS group.
Measures
Demographic information was collected by using a standardized form at baseline. Parent participants also completed 2 self-administered health literacy tools at baseline, Short Test of Functional Health Literacy in Adults (S-TOFHLA)38 and Newest Vital Sign (NVS).39 Health literacy was categorized using both the S-TOFHLA (0–16 inadequate, 17–22 marginal, and 23–36 adequate health literacy)38 and NVS scores (0–1 high likelihood of limited, 2–3 possible limited, and 4–6 adequate health literacy).39 General health literacy scores were not calculated for 3 intervention and 4 standard curriculum parents who were illiterate.
To assess care practices related to URIs, parent participants in both groups reported weekly via telephone for 5 months from the end of the classes in mid-December 2009 into mid-May 2010. Parents reported illnesses in the household, symptoms, care sought, and medications/home remedies used for all family members, not just those in EHS. If a medication was used, the name and dosing tool was reported. The research team called parents who failed to report. Research staff conducted home visits on a random sample of telephone reports of medications (n = 95) to determine accuracy (93.7% accurate [95% confidence interval (CI), 86.9%–97.4%]). All but 1 erroneous report took place in the first 6 study-weeks. Families received $25/month to defray costs of required telephone calls.
A Knowledge-Attitudes (KA) instrument was also verbally administered at 2 time points in English or Spanish to the intervention and standard curriculum parent who was the main EHS participant: before initiation of the educational intervention and again in spring 2010. The KA instrument was adapted from instruments used in community studies8,23,29 and was previously piloted in this setting.33
Outcome Variables
The main outcomes of interest were PED visits and adverse care practices, which included inappropriate use of OTC cough/cold medications, incorrect use of dosing measurement tool, and use of unprescribed antibiotics. We also assessed URI knowledge/attitudes and home remedy safety attitudes.
PED use was defined as the number of PED visits and the proportion of all illness episodes that resulted in a PED visit, by self-report. Of the PED visits reported as having occurred at Columbia University Medical Center (57.4% of total), 85.2% were verified in the electronic health record. An inappropriate use of an OTC medication was defined as a family reporting, during any phone report, administering an OTC cough/cold medication to a child <2 years old, based on the Federal Drug Administration’s (FDA) public health advisory against the use of OTC cough/cold medications for such children.40 A family was considered to have incorrectly used a dosing measurement tool if the parent reported administering a liquid medication with either a regular kitchen spoon (not measuring spoon) or giving an unmeasured amount. A family was considered to have used an unprescribed antibiotic if the parent reported giving an antibiotic received from anywhere other than a prescribing clinician, including botánica/bodega, leftover or shared prescription, brought from other country, or from a pharmacy without a prescription. To include all EHS-aged children, the analyses focused on children age <4 years except for the analysis related to OTC medication use, as described above.
A composite KA score (0–10) was adapted from the score validated in our pilot study.33 Parents were given a score of 1 for each correct response at baseline and post-intervention (Supplemental Table 4). Attitude toward home remedies was determined by asking parents at baseline and post-intervention if they agreed, disagreed, or were not sure about the statement: “All home remedies are safe.”
Statistical Analysis
All primary analyses were conducted on an intention-to-treat basis in which intervention families were included regardless of attendance. For PED use, to first identify the absolute number of PED visits as an indication of use, the proportion of all illness episodes that resulted in a PED visit was compared between intervention and standard curriculum groups by using Pearson’s χ2 test. Then, to provide a family-level analysis while accounting for the non-independence of multiple illness episodes in a child or family, a Wilcoxon rank-sum test was used to compare between groups the proportion of times a family had a child who was ill and went to the PED, weighted by number of illness episodes.
Percent of households ever reporting inappropriate use of OTC cough/cold medication for children, incorrect use of measurement tool for child, and use of unprescribed antibiotics were also compared separately between groups using χ2 tests and odds ratios (ORs). Both the overall mean and change in score pre- to post-intervention were compared between groups using t tests, and home remedy attitudes by using Pearson’s χ2 test.
Confirmatory analyses were performed adjusting in regression models for the program that administered the child’s EHS site. All analyses were conducted by using Stata/SE 11 (Stata Corp, College Station, TX), SPSS 18.0 (IBM SPSS Statistics, IBM Corporation), and SAS 9.3 (SAS Institute, Inc, Cary, NC).
Results
A total of 154 families were enrolled (n = 76 intervention; n = 78 standard curriculum), 197 children were <4 years old (n = 99 intervention; n = 98 standard curriculum). A high proportion (94.8%) of families reported data through the entire 5-month period, and 94.2% completed the post-intervention survey. Participant parents were primarily Latino, Spanish-speaking, and low-income, and only 17% had adequate health literacy on the NVS (Table 1). Intervention parents were somewhat more likely to be Latino and Spanish-speaking, although there was no significant difference in English proficiency. Children were somewhat more likely to be Latino (Table 2). Site demographics were similar (Supplemental Table 5).
TABLE 1.
Characteristics of Parent Participants: Demographics and Health Literacy
| Intervention (n = 76) | Standard Curriculum (n = 78) | |
|---|---|---|
| Age, y | ||
| 19 to 29 | 51.3 (39) | 53.8 (42) |
| ≥30 | 48.7 (37) | 46.2 (36) |
| Race/ethnicity | ||
| Latino | 98.7 (74) | 88.2 (67) |
| Black, non-Latino | 0 (0) | 3.9 (3) |
| White, non-Latino | 0 (0) | 3.9 (3) |
| Other, non-Latino | 1.3 (1) | 3.9 (3) |
| Born in the United States | ||
| No | 92.1 (70) | 87.2 (68) |
| Primary language | ||
| Spanish | 93.4 (71) | 80.8 (63) |
| English | 5.3 (4) | 17.9 (14) |
| Other | 1.3 (1) | 1.3 (1) |
| English proficiency | ||
| Excellent–good | 21.1 (16) | 30.8 (24) |
| Fair | 26.3 (20) | 14.1 (11) |
| Poor–not at all | 52.6 (40) | 55.1 (43) |
| Education | ||
| <High school | 48.7 (37) | 44.9 (35) |
| High school | 22.4 (17) | 26.9 (21) |
| Some college | 28.9 (22) | 28.2 (22) |
| Health literacya | ||
| S-TOFHLA | ||
| Adequate | 71.2 (52) | 64.9 (48) |
| Marginal | 11.0 (8) | 18.9 (14) |
| Inadequate | 17.8 (13) | 16.2 (12) |
| NVS | ||
| Adequate | 17.8 (13) | 16.2 (12) |
| Possible limited | 47.9 (35) | 37.8 (28) |
| High likelihood limited | 34.2 (25) | 45.9 (34) |
All data are presented as % (n). NVS. Newest Vital Sign; S-TOFHLA, Short Test of Functional Health Literacy in Adults.
N = 73 intervention, 74 standard curriculum; 3 intervention and 4 standard curriculum illiterate.
TABLE 2.
Characteristics of Pediatric Participants Younger Than Age 4 Years
| Intervention (n = 99) | Standard Curriculum (n = 98) | |
|---|---|---|
| Age, mo | 20.8 ± 12.1 | 22.7 ± 10.9 |
| Gender | ||
| Male | 45.5 (45) | 45.9 (45) |
| Race/ethnicity | ||
| Latino | 93.8 (90) | 82.1 (78) |
| Black, non-Latino | 0 | 4.2 (4) |
| White, non-Latino | 1.0 (1) | 5.3 (5) |
| Other, non-Latino | 5.2 (5) | 8.4 (8) |
| Born in the United States | ||
| No | 3.0 (3) | 1.0 (1) |
| Insurance | ||
| Private | 10.1 (10) | 5.1 (5) |
| Public insurance | 89.9 (89) | 94.9 (93) |
All data are presented as % (n).
A little less than half of intervention parents (46.1%) attended all 3 sessions, 43.4% attended 2 sessions, 7.9% 1 session, and 2.6% no sessions. Almost all intervention parents reported that the education sessions (97.3%) and URI kit (93.0%) were very useful; 87.3% used the kit at least a few times over the winter. The most commonly used items were tissues (97.2%), digital thermometer (83.1%), saline drops (83.1%), oral syringe (76.1%), and bulb suction (66.2%).
There were 396 episodes of illness reported for children <4 years old (205 intervention, 191 standard curriculum). Children <4 years old from intervention families had fewer PED visits per illness episode than the standard curriculum group (18 of 205 [8.8%] vs 29 of 191 [15.2%] illness episodes; P = .049). The majority of this difference was for children age 6 to <48 months (intervention families 16 of 194 [8.2%] vs 29 of 185 [15.7%] illness episodes; P = .025). The relationship between intervention status and fewer PED visits was also significant on the family level (P = .03). When analyses were repeated for only Latino families and after adjusting for program, results were not materially different on the family level analyses: on the individual visit level analysis adjusting for program, P = .054 for the whole sample, but for the Latino-only sample, P = .029. Intervention families attending all 3 classes had 6.2% of illness episodes result in a PED visit for a child age 6 to <48 months (5 of 80), whereas those attending 2 classes had 7.8% (8 of 102) and 0 or 1 class had 25% (3 of 12) (P = .087).
For 72.7% of illness reports for children <4 years old, a medication was used (n = 148 intervention, n = 140 standard curriculum). Intervention families had lower odds post-intervention of giving an inappropriate OTC medication to a child <2 years (OR, 0.29; 95% CI 0.089–0.95; 12.2% vs 32.4%; P = .034) (Table 3). Intervention families also had lower odds post-intervention of using an incorrect dosing tool for a child age <4 years (OR, 0.24; 95% CI 0.079–0.74; 9.8% vs 31.1%; P = .009). There was no difference between groups in use of unprescribed antibiotics for a child age <4 years (0% vs 1.9%; P = .29). When these analyses were repeated for only parents who were Latino and after adjusting for program, results were not materially different.
TABLE 3.
Impact of Intervention on Household Care Practices During Illness Episodes
| Standard Curriculum | Intervention | P Value | |
|---|---|---|---|
| PED visit, child age <4 y | 15.2 (29) | 8.8 (18) | .049 |
| PED visit, child age 6 mo to <4 y | 15.7 (29) | 8.2 (16) | .025 |
| Household had at least 1 illness episode in which used an inappropriate OTC medication, child age <2 y | 32.4 (11) | 12.2 (5) | .034 |
| Household had at least 1 illness episode in which used an incorrect dosing tool, child age <4 y | 31.3 (14) | 9.8 (5) | .009 |
| Household had at least 1 illness episode in which used an unprescribed antibiotic, child age <4 y | 1.9 (1) | 0 (0) | .29 |
All data are presented as % (n), except P values.
Mean baseline KA scores were similar for intervention and standard curriculum families (4.2 vs 4.6 of 10; P = .27). Mean post-intervention scores increased to 5.5 for intervention families but remained the same (4.7) for standard curriculum ones (P = .011), and the mean difference in baseline-to-post scores for intervention families was significantly different than for standard curriculum families (1.3 vs 0.097; P = .001). Home remedy beliefs at baseline were also similar (28.9% of intervention families believed all home remedies were safe or were unsure vs 37.2% of standard curriculum families; P = .28), but were different post-intervention (17.8% vs 38.9%; P = .005). The percent of intervention families who had incorrect home remedy beliefs post-intervention (52.0%) was also lower, but not significantly lower, than the standard curriculum families (75.7%; P = .053), when those who had both correct baseline and post-intervention beliefs were removed. As a sensitivity analysis, analyses were repeated for only parents who were Latino and results were not materially different, except for the change in post-intervention home remedy beliefs (P = .023). Additionally, after adjusting for program, results were not materially different.
Discussion
By using a site-randomized design, we found that a URI-related health literacy intervention embedded into an EHS program reduced PED use in the setting of more illness episodes. It also decreased adverse care practices related to medication dosing and OTC medication use, and had a positive impact on health knowledge. Parent health education is a standard performance indicator for EHS, and EHS serves nearly 175 000 children nationally; therefore the use of such a curriculum in EHS has the potential for widespread dissemination.31
Our study illustrates the potential strength of using EHS for a health literacy intervention. Integrating the educational intervention into an existing EHS allowed inclusion of parents outside the medical setting. Additionally, providing information in a setting in which parents were comfortable receiving health information may have lent credibility. Although some other educational interventions have been successful in increasing knowledge, attitudes, and care practices regarding URI,25,27–29 they were conducted predominately in non-minority populations, with higher literacy levels, and many took place in primary care offices or pharmacies. One study of Head Start parents did show that providing a training session and a reference book could help reduce PED and clinic visits but used a pre-post design rather than a control group.41
PED use remains high for non-urgent conditions, which impacts both continuity of care in the medical home as well as cost of care.42–44 On a national scale, even small changes in PED visits could have an important impact on costs. Low-income families like those served by EHS are at highest risk for seeking PED care for a URI,8 highlighting the potential impact of an EHS-based intervention strategy. Previous studies have identified greater trust in the medical expertise of the PED compared with their primary care provider as a main motivator for seeking PED care.44–46 Our intervention included information regarding which symptoms could be cared for by their primary care provider, which may have contributed to decreased PED use.
The positive impact of this intervention on OTC use and medication dosing also illustrates the potential use of non-medical settings for distributing information regarding important health issues. Despite the 2008 FDA public health advisory regarding voluntary removal of OTC medications for children <2 years old,40 a 2011 national poll revealed that 61% of those families surveyed had used OTC cough and cold medication for a child age 6 to 24 months in the previous 12 months.15 There has also been national attention regarding medication measurement errors.47 Although we did observe an intervention effect on OTC and medication measurement, we did not see an effect on the use of unprescribed antibiotics. In a previous study in this community, we observed that antibiotics were frequently obtained from bodegas without prescription for adults, but not for children.23 In other parts of the country, use of unprescribed antibiotics remains a concern. For example, the FDA issued a warning about fake pediatric antibiotics targeted for Spanish speakers that led to hospitalization of several children.48
Finally, in addition to improving knowledge regarding URI overall, the intervention also had an impact on attitudes toward home remedy use. Home remedy use even for young children is not uncommon,13,49 and although many home remedies are safe to use, some are not.12,37,50–52 Additionally, many patients do not disclose home remedy use to their health care providers.49
In our intervention we did not discourage the use of home remedies, but rather encouraged that families be informed about their safety and discuss them with their providers. Importantly, our home remedy curriculum was tailored to those remedies used most often in this community.
There were several limitations to this study. First, this study took place in a single community and randomization was site-based as opposed to individual. To limit organization/program-based differences, we selected 1 intervention and 1 standard curriculum site per program. However, because the unit of analysis was the family, in some respects it is a quasi-experimental study. Additionally, we were not able to fully account for potential effects of clustering owing to the small number of clusters; however, we found similar effects when we adjusted for EHS program. Furthermore, the randomized sites did not differ with respect to demographic variables with the exception of Latino ethnicity, which was accounted for in the sensitivity analyses. Secondly, blinding of data collection was not feasible, and most outcomes were self-reported, which could have been affected by social desirability bias. We attempted to mitigate this concern, however, by making home visits to assess the accuracy of reporting of medications administered and conducting chart reviews to verify reported visits to the local medical center. Other URI-related studies also use self-report methodology.8 Additionally, the collection of information over the phone could have reinforced the intervention; this was conducted for the standard curriculum group as well. We also did not a priori indicate what would constitute a clinically significant difference, however, we do believe reduction in the odds of a household having a harmful care practice of 71% to 76% and reduction in ED visits are significant benefits, especially for an intervention that is straightforward to implement and relates to an EHS standard performance indicator. Finally, the 2 general health literacy tools gave differing scores, making it difficult to make an overall assessment on the general health literacy level.53 The study also had several strengths, including its randomized design, low attrition rate, and the use of PED visits as an outcome.
Conclusions
A URI health literacy-related educational intervention embedded into EHS decreased PED visits and adverse care practices.
Supplementary Material
Acknowledgments
We thank our community health workers, including Dulce Barrios, Carmen Acevedo, and Maria Gonzalez, and our data manager Myra Joyce. We thank Rajasekhar Ramakrishnan, EngScD and Stephen Holleran for their statistical assistance, and Steven Shea, MD, MS for his critical review of the manuscript. We thank the Columbia University and Children’s Aid Society P.S. 5 and P.S. 8 EHS staff and the parents in the participating classes. Special thanks to Andrew Seltzer, EdD, Children’s Aid Society Early Childhood Deputy Director For Family Services, and Erica Quezada-Selman, LMSW, MS Ed, CD (DONA), CEIM, Tamara Royal, MA, Marlene Aranda Gillman, LCSW, Esther Olvera, MS Ed, and Carmen Gonzalez, MS Ed from the Children’s Aid Society, and Maria Guzman, MHC and Fatima Beccar-Varella, MS from Columbia University EHS. Design of the educational intervention was supported by grant UL1 RR024156 from the National Center for Research Resources, a component of the National Institutes of Health (NIH) and NIH Roadmap for Medical Research and built on a health literacy module supported by a grant from the Health Resources Services Administration. This manuscript’s contents are solely the responsibility of the authors and do not necessarily represent the official views of the funding agencies. The funding agencies had no role in the design and conduct of the study; collection, management, analysis, or interpretation of the data; or preparation, review, or approval of the manuscript.
Glossary
- CI
confidence interval
- EHS
Early Head Start
- FDA
Food and Drug Administration
- KA
Knowledge-Attitudes
- NVS
Newest Vital Sign
- OR
odds ratio
- OTC
over-the-counter
- PED
pediatric emergency department
- S-TOFHLA
Short Test of Functional Health Literacy in Adults
- URI
upper respiratory infection
Footnotes
Dr Stockwell conceptualized and designed the study, took part in the analysis of the data, and drafted the initial manuscript; Drs Catallozzi, Larson, Rodriguez, Subramony, and Meyer aided in the conceptualization and design of the study and reviewed and revised the manuscript; Dr Andres Martinez carried out the initial analyses and critically reviewed the manuscript; Ms Martinez helped in the design of the educational material, coordinated the teaching aspect of the intervention, and critically reviewed the manuscript; Ms Barrett helped design the data collection instruments, coordinated and supervised data collection at all sites, and critically reviewed the manuscript; and all authors approved the final manuscript as submitted.
This trial has been registered at www.clinicaltrials.gov (identifier NCT01916031).
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: Supported by grant RC1MD004109 from the National Institutes of Health/National Institute on Minority Health and Health Disparities. Funded by the National Institutes of Health (NIH).
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
References
- 1.Chonmaitree T, Revai K, Grady JJ, et al. Viral upper respiratory tract infection and otitis media complication in young children. Clin Infect Dis. 2008;46(6):815–823 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dales RE, Cakmak S, Brand K, Judek S. Respiratory illness in children attending daycare. Pediatr Pulmonol. 2004;38(1):64–69 [DOI] [PubMed] [Google Scholar]
- 3.Carabin H, Gyorkos TW, Soto JC, Penrod J, Joseph L, Collet JP. Estimation of direct and indirect costs because of common infections in toddlers attending day care centers. Pediatrics. 1999;103(3):556–564 [DOI] [PubMed] [Google Scholar]
- 4.Jacobson JS, Goldstein IF, Canfield SM, et al. Early respiratory infections and asthma among New York City Head Start children. J Asthma. 2008;45(4):301–308 [DOI] [PubMed] [Google Scholar]
- 5.Kuzujanakis M, Kleinman K, Rifas-Shiman S, Finkelstein JA. Correlates of parental antibiotic knowledge, demand, and reported use. Ambul Pediatr. 2003;3(4):203–210 [DOI] [PubMed] [Google Scholar]
- 6.Vanden Eng J, Marcus R, Hadler JL, et al. Consumer attitudes and use of antibiotics. Emerg Infect Dis. 2003;9(9):1128–1135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Larson E, Ferng YH, Wong J, et al. Knowledge and misconceptions regarding upper respiratory infections and influenza among urban Hispanic households: need for targeted messaging. J Immigr Minor Health. 2009;11(2):71–82 [DOI] [PubMed] [Google Scholar]
- 8.Lee GM, Friedman JF, Ross-Degnan D, Hibberd PL, Goldmann DA. Misconceptions about colds and predictors of health service utilization. Pediatrics. 2003;111(2):231–236 [DOI] [PubMed] [Google Scholar]
- 9.Friedman JF, Lee GM, Kleinman KP, Finkelstein JA. Acute care and antibiotic seeking for upper respiratory tract infections for children in day care: parental knowledge and day care center policies. Arch Pediatr Adolesc Med. 2003;157(4):369–374 [DOI] [PubMed] [Google Scholar]
- 10.Saunders NR, Tennis O, Jacobson S, Gans M, Dick PT. Parents’ responses to symptoms of respiratory tract infection in their children. CMAJ. 2003;168(1):25–30 [PMC free article] [PubMed] [Google Scholar]
- 11.Dart RC, Paul IM, Bond GR, et al. Pediatric fatalities associated with over the counter (nonprescription) cough and cold medications. Ann Emerg Med. 2009;53(4):411–417 [DOI] [PubMed] [Google Scholar]
- 12.Rodriguez-Fragoso L, Reyes-Esparza J, Burchiel SW, Herrera-Ruiz D, Torres E. Risks and benefits of commonly used herbal medicines in Mexico. Toxicol Appl Pharmacol. 2008;227(1):125–135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zhang Y, Fein EB, Fein SB. Feeding of dietary botanical supplements and teas to infants in the United States. Pediatrics. 2011;127(6):1060–1066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lokker N, Sanders L, Perrin EM, et al. Parental misinterpretations of over-the-counter pediatric cough and cold medication labels. Pediatrics. 2009;123(6):1464–1471 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.CS Mott Children’s Hospital. Despite warnings, parents continue to use cough & cold medicines for young kids. Natl Poll Childr Health. 2011;12(1)
- 16.Yin HS, Mendelsohn AL, Wolf MS, et al. Parents’ medication administration errors: role of dosing instruments and health literacy. Arch Pediatr Adolesc Med. 2010;164(2):181–186 [DOI] [PubMed] [Google Scholar]
- 17.Braun BL, Fowles JB. Characteristics and experiences of parents and adults who want antibiotics for cold symptoms. Arch Fam Med. 2000;9(7):589–595 [DOI] [PubMed] [Google Scholar]
- 18.Nielson-Bohlman L, Panzer A, Hamlin H, Kindig D. Health Literacy: A Prescription to End Confusion. Washington DC: Institution of Medicine; 2004 [PubMed]
- 19.US Department of Education, Institute of Education Sciences. The Health Literacy of America's Adults Results From the 2003 National Assessment of Adult Literacy. Available at: http://nces.ed.gov/pubs2006/2006483.pdf. Accessed February 24, 2014 [Google Scholar]
- 20.Mangione-Smith R, Elliott MN, Stivers T, McDonald L, Heritage J, McGlynn EA. Racial/ethnic variation in parent expectations for antibiotics: implications for public health campaigns. Pediatrics. 2004;113(5). Available at: www.pediatrics.org/cgi/content/full/113/5/e385 [DOI] [PubMed] [Google Scholar]
- 21.Corbett KK, Gonzales R, Leeman-Castillo BA, Flores E, Maselli J, Kafadar K. Appropriate antibiotic use: variation in knowledge and awareness by Hispanic ethnicity and language. Prev Med. 2005;40(2):162–169 [DOI] [PubMed] [Google Scholar]
- 22.Larson E, Lin SX, Gomez-Duarte C. Antibiotic use in Hispanic households, New York city. Emerg Infect Dis. 2003;9(9):1096–1102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Larson EL, Dilone J, Garcia M, Smolowitz J. Factors which influence Latino community members to self-prescribe antibiotics. Nurs Res. 2006;55(2):94–102 [DOI] [PubMed] [Google Scholar]
- 24.Finkelstein JA, Davis RL, Dowell SF, et al. Reducing antibiotic use in children: a randomized trial in 12 practices. Pediatrics. 2001;108(1):1–7 [DOI] [PubMed] [Google Scholar]
- 25.Finkelstein JA, Huang SS, Kleinman K, et al. Impact of a 16-community trial to promote judicious antibiotic use in Massachusetts. Pediatrics. 2008;121(1). Available at: www.pediatrics.org/cgi/content/full/121/1/e15 [DOI] [PubMed] [Google Scholar]
- 26.Taylor JA, Kwan-Gett TS, McMahon EM., Jr Effectiveness of a parental educational intervention in reducing antibiotic use in children: a randomized controlled trial. Pediatr Infect Dis J. 2005;24(6):489–493 [DOI] [PubMed] [Google Scholar]
- 27.Belongia EA, Sullivan BJ, Chyou PH, Madagame E, Reed KD, Schwartz B. A community intervention trial to promote judicious antibiotic use and reduce penicillin-resistant Streptococcus pneumoniae carriage in children. Pediatrics. 2001;108(3):575–583 [DOI] [PubMed] [Google Scholar]
- 28.Huang SS, Rifas-Shiman SL, Kleinman K, et al. Parental knowledge about antibiotic use: results of a cluster-randomized, multicommunity intervention. Pediatrics. 2007;119(4):698–706 [DOI] [PubMed] [Google Scholar]
- 29.Trepka MJ, Belongia EA, Chyou PH, Davis JP, Schwartz B. The effect of a community intervention trial on parental knowledge and awareness of antibiotic resistance and appropriate antibiotic use in children. Pediatrics. 2001;107(1). Available at: www.pediatrics.org/cgi/content/full/107/1/e6 [DOI] [PubMed] [Google Scholar]
- 30.Centers for Disease Control and Prevention. Interagency Task Force on Antimicrobial Resistance: a public health action plan to combat antimicrobial resistance. Available at: www.cdc.gov/drugresistance/actionplan/actionPlan.html. Accessed January 26, 2014
- 31.Head Start Program Fact Sheet Fiscal Year 2012. Available at: http://eclkc.ohs.acf.hhs. gov/hslc/mr/factsheets/2012-hs-program-factsheet.html. Accessed January 26, 2014
- 32.Herman AD, Mayer GG. Reducing the use of emergency medical resources among Head Start families: a pilot study. J Community Health. 2004;29(3):197–208 [DOI] [PubMed] [Google Scholar]
- 33.Stockwell MS, Catallozzi M, Meyer D, Rodriguez C, Martinez E, Larson E. Improving care of upper respiratory infections among Latino Early Head Start parents. J Immigr Minor Health. 2010;12(6):925–931 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Larson EL, Ferng YH, Wong-McLoughlin J, Wang S, Haber M, Morse SS. Impact of non-pharmaceutical interventions on URIs and influenza in crowded, urban households. Public Health Rep. 2010;125(2):178–191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Curriculum HEAL. Columbia University Department of Pediatrics’ Community Pediatrics. Available at: www.communityped.org/ under Publications; Other; HEAL Curriculum. Available at: www.communityped.org. Accessed January 25, 2014
- 36.Meyer D, Martinez E, Mauricio R, Ip M. Bridging the communication gap between providers and patients by addressing health literacy in an urban immigrant community. CES4Health, 2013. Available at: www.ces4health.info/find-products/search-results.aspx. Accessed January 26, 2014
- 37.Community Pediatrics Program, Columbia University Department of Pediatrics at Morgan Stanley Children’s Hospital of NewYork-Presbyterian. The quick guide to home remedies: caring for the children of the Washington Heights and Inwood communities. Available at: www.columbia.edu/itc/hs/medical/residency/peds/new_ compeds_site/pdfs_new/quick_guideto_homeremedies2-20-08.pdf. Accessed January 26, 2014
- 38.Baker DW, Williams MV, Parker RM, Gazmararian JA, Nurss J. Development of a brief test to measure functional health literacy. Patient Educ Couns. 1999;38(1):33–42 [DOI] [PubMed] [Google Scholar]
- 39.Weiss BD, Mays MZ, Martz W, et al. Quick assessment of literacy in primary care: the newest vital sign. Ann Fam Med. 2005;3(6):514–522 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Food and Drug Administration. FDA releases recommendations regarding use of over-the-counter cough and cold products. January 17, 2008. Available at: www.fda.gov/newsevents/newsroom/pressannouncements/2008/ucm116839.htm. Accessed January 26, 2014
- 41.Herman A, Jackson P. Empowering low-income parents with skills to reduce excess pediatric emergency room and clinic visits through a tailored low literacy training intervention. J Health Commun. 2010;15(8):895–910 [DOI] [PubMed] [Google Scholar]
- 42.Doobinin KA, Heidt-Davis PE, Gross TK, Isaacman DJ. Nonurgent pediatric emergency department visits: care-seeking behavior and parental knowledge of insurance. Pediatr Emerg Care. 2003;19(1):10–14 [DOI] [PubMed] [Google Scholar]
- 43.Stanley R, Zimmerman J, Hashikawa C, Clark SJ. Appropriateness of children’s nonurgent visits to selected Michigan emergency departments. Pediatr Emerg Care. 2007;23(8):532–536 [DOI] [PubMed] [Google Scholar]
- 44.Stockwell MS, Findley SE, Irigoyen M, Martinez RA, Sonnett M. Change in parental reasons for use of an urban pediatric emergency department in the past decade. Pediatr Emerg Care. 2010;26(3):181–185 [DOI] [PubMed] [Google Scholar]
- 45.Sempere-Selva T, Peiro S, Sendra-Pina P, Martinez-Espin C, Lopez-Aguilera I. Inappropriate use of an accident and emergency department: magnitude, associated factors, and reasons—an approach with explicit criteria. Ann Emerg Med. 2001;37(6):568–579 [DOI] [PubMed] [Google Scholar]
- 46.Goepp JG, Chin NP, Massad J, Edwards LA. Pediatric emergency department outreach: solving medical problems or revealing community solutions? J Health Care Poor Underserved. 2004;15(4):522–529 [DOI] [PubMed] [Google Scholar]
- 47.Food and Drug Administration. FDA issues final guidance for liquid OTC drug products with dispensing devices. May 4, 2011. Available at: www.fda.gov/NewsEvents/ Newsroom/PressAnnouncements/default.htm. Accessed January 26, 2014
- 48.Food and Drug Administration. FDA: don’t buy drugs marketed as antimicrobial dietary supplements. May 13, 2011. Available at: www.fda.gov/NewsEvents/Newsroom/ PressAnnouncements/default.htm. Accessed January 26, 2014
- 49.Graham RE, Ahn AC, Davis RB, O’Connor BB, Eisenberg DM, Phillips RS. Use of complementary and alternative medical therapies among racial and ethnic minority adults: results from the 2002 National Health Interview Survey. J Natl Med Assoc. 2005;97(4):535–545 [PMC free article] [PubMed] [Google Scholar]
- 50.Khine H, Weiss D, Graber N, Hoffman RS, Esteban-Cruciani N, Avner JR. A cluster of children with seizures caused by camphor poisoning. Pediatrics. 2009;123(5):1269–1272 [DOI] [PubMed] [Google Scholar]
- 51.Ize-Ludlow D, Ragone S, Bernstein JN, Bruck IS, Duchowny M, Garcia Pena BM. Chemical composition of Chinese star anise (Illicium verum) and neurotoxicity in infants. JAMA. 2004;291(5):562–563 [DOI] [PubMed] [Google Scholar]
- 52.Lead poisoning associated with ayurvedic medications—five states, 2000–2003. MMWR Morb Mortal Wkly Rep. 2004;53(26):582–584 [PMC free article] [PubMed] [Google Scholar]
- 53.Dunn-Navarra AM, Stockwell MS, Meyer D, Larson E. Parental health literacy, knowledge and beliefs regarding upper respiratory infections (URI) in an urban Latino immigrant population. J Urban Health. 2012;89(5):848–860 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Stockwell MS, Catallozzi M, Meyer D, Rodriguez C, Martinez E, Larson E. Improving care of upper respiratory infections among Latino Early Head Start parents. J Immigr Minor Health. 2010;12(6):925–931 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


