Table 2.
Summary of Impact of ADDs on Medication Errors
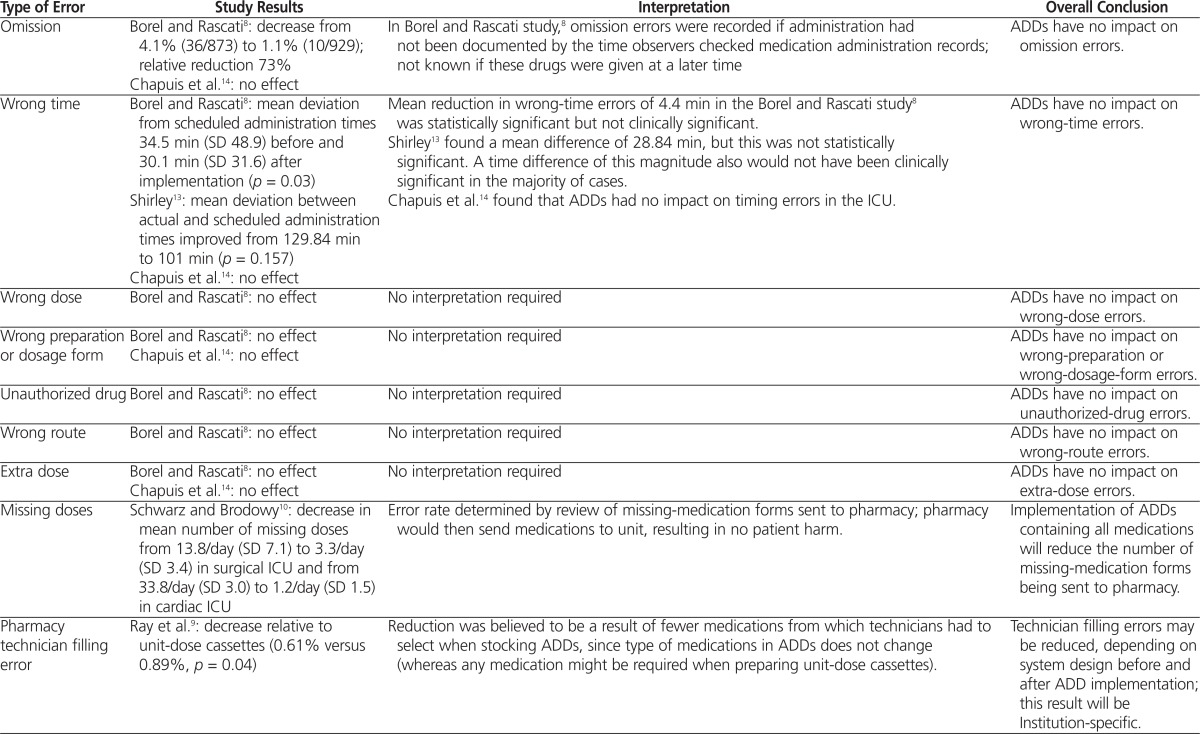
| Type of Error | Study Results | Interpretation | Overall Conclusion |
|---|---|---|---|
| Omission | Borel and Rascati8: decrease from 4.1% (36/873) to 1.1% (10/929); relative reduction 73% Chapuis et al.14: no effect |
In Borel and Rascati study,8 omission errors were recorded if administration had not been documented by the time observers checked medication administration records; not known if these drugs were given at a later time | ADDs have no impact on omission errors. |
| Wrong time | Borel and Rascati8: mean deviation from scheduled administration times 34.5 min (SD 48.9) before and 30.1 min (SD 31.6) after implementation (p = 0.03) Shirley13: mean deviation between actual and scheduled administration times improved from 129.84 min to 101 min (p = 0.157) Chapuis et al.14: no effect |
Mean reduction in wrong-time errors of 4.4 min in the Borel and Rascati study8 was statistically significant but not clinically significant. Shirley13 found a mean difference of 28.84 min, but this was not statistically significant. A time difference of this magnitude also would not have been clinically significant in the majority of cases. Chapuis et al.14 found that ADDs had no impact on timing errors in the ICU. |
ADDs have no impact on wrong-time errors. |
| Wrong dose | Borel and Rascati8: no effect | No interpretation required | ADDs have no impact on wrong-dose errors. |
| Wrong preparation or dosage form | Borel and Rascati8: no effect Chapuis et al.14: no effect |
No interpretation required | ADDs have no impact on wrong-preparation or wrong-dosage-form errors. |
| Unauthorized drug | Borel and Rascati8: no effect | No interpretation required | ADDs have no impact on unauthorized-drug errors. |
| Wrong route | Borel and Rascati8: no effect | No interpretation required | ADDs have no impact on wrong-route errors. |
| Extra dose | Borel and Rascati8: no effect Chapuis et al.14: no effect |
No interpretation required | ADDs have no impact on extra-dose errors. |
| Missing doses | Schwarz and Brodowy10: decrease in mean number of missing doses from 13.8/day (SD 7.1) to 3.3/day (SD 3.4) in surgical ICU and from 33.8/day (SD 3.0) to 1.2/day (SD 1.5) in cardiac ICU | Error rate determined by review of missing-medication forms sent to pharmacy; pharmacy would then send medications to unit, resulting in no patient harm. | Implementation of ADDs containing all medications will reduce the number of missing-medication forms being sent to pharmacy. |
| Pharmacy technician filling error | Ray et al.9: decrease relative to unit-dose cassettes (0.61% versus 0.89%, p = 0.04) | Reduction was believed to be a result of fewer medications from which technicians had to select when stocking ADDs, since type of medications in ADDs does not change (whereas any medication might be required when preparing unit-dose cassettes). | Technician filling errors may be reduced, depending on system design before and after ADD implementation; this result will be Institution-specific. |
| Preparation error | Chapuis et al.14: decrease from 3.8% to 0.5% (p = 0.017) in a medical ICU | During direct observation, Chapuis et al.14 found a reduction in errors related to the preparation of medications after implementation of ADDs. Exact definition of preparation errors was not given, but there is no reason that ADDs should influence nurses’ preparation of medications, especially given that the same study showed no difference in picking errors. | Inconclusive |
| Storage error | Chapuis et al.14: decrease by 14.4% (p < 0.01) | This was the only study that assessed storage errors; although it was conducted in the ICU, there is no reason to think this benefit would not be seen in other patient care units. | The use of ADDs will reduce storage errors. |
ADD = automated dispensing device, ICU = intensive care unit, SD = standard deviation.
