Abstract
Objective
Use classification tree analysis with lagged predictors to determine empirically derived cut-points for identifying adolescent girls at risk for future onset of threshold, subthreshold, and partial eating disorders and test for interactions between risk factors that may implicate qualitatively distinct risk pathways.
Method
Data were drawn from a prospective study of 496 adolescent girls who completed diagnostic interviews and surveys annually for 8 years.
Results
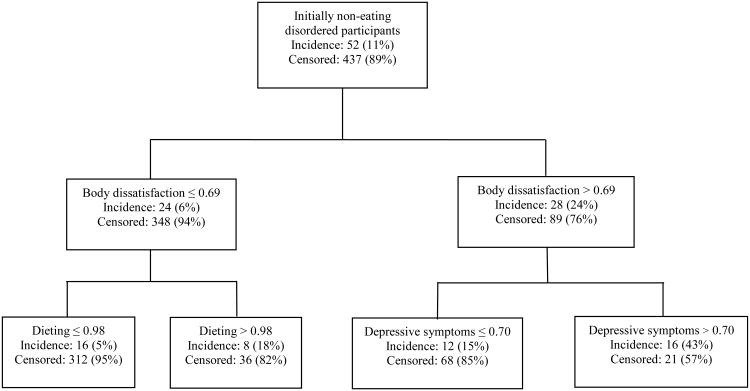
Body dissatisfaction emerged as the most potent predictor; adolescent girls in the upper 24% of body dissatisfaction showed a 4.0-fold increased incidence of eating disorder onset (24% vs. 6%). Among participants in the high body dissatisfaction branch, those in the upper 32% of depressive symptoms showed a 2.9-fold increased incidence of onset (43% vs. 15%). Among participants in the low body dissatisfaction branch, those in the upper 12% of dieting showed a 3.6-fold increased incidence onset (18% vs. 5%).
Conclusion
This three-way interaction suggests a body dissatisfaction pathway to eating disorder onset that is amplified by depressive symptoms, as well as a pathway characterized by self-reported dieting among young women who are more satisfied with their bodies. It may be possible to increase the effectiveness of prevention programs by targeting each of these qualitatively distinct risk groups, rather than only individuals with a single risk factor.
Keywords: risk factors, prospective, longitudinal, pathways, eating disorders
Threshold and subthreshold anorexia nervosa, bulimia nervosa, binge eating disorder, and purging disorder show a chronic course and result in functional impairment, emotional distress, and medical problems (Hudson, Hiripi, Pope, & Kessler, 2007; Milos, Spindler, Schnyder, & Fairburn, 2005; Stice, Marti, Shaw, & Jaconis, 2009; Striegel-Moore, Seeley, & Lewinsohn, 2003). Because eating disorders are so pernicious, it is important to offer prevention programs that reduce risk for these conditions. Selected prevention programs targeting individuals at high risk for eating disorders produce significantly larger effects than universal prevention programs targeting unselected populations (Stice, Shaw, & Marti, 2007). Thus, it is vital to examine scales that identify youth at high risk for onset of eating disorders for selective prevention programs.
Few studies have examined risk factors that predict future onset of threshold, subthreshold, or partial eating disorders. It is important to include subthreshold and partial eating disorders because they are more prevalent than threshold eating disorders (Favaro, Ferrara, & Santonastaso, 2003; Stice, et al., 2009) and most individuals who present for eating disorder treatment do not meet criteria for threshold eating disorders (Fisher, Schneider, Burns, Symons, & Mandel, 2001). Adolescent females reporting social pressure to be thin and body image preoccupation have shown a higher risk for onset of threshold or subthreshold bulimia nervosa or binge eating disorder (McKnight, 2003), those reporting weight and shape concerns and negative affectivity have shown a higher risk for future onset of threshold or subthreshold bulimia nervosa (Killen et al., 1996), those reporting elevated stress have shown increased risk for future onset of binge eating disorder (Striegel-Moore et al., 2007), and those reporting elevated dietary restraint have shown elevated risk for onset of threshold or subthreshold bulimia nervosa (Stice, Davis, Miller, & Marti, 2008). It is arguably more important to identify youth at elevated risk for any eating disorder because prevention programs should ideally target all eating disorders, rather than just one type of eating disorder. Elevated dietary restraint has been found to increase risk for onset of any eating disorder (Fairburn, Cooper, Doll, & Davies, 2005; Patton, Selzer, Coffey, Carlin, & Wolfe, 1999; Santonastaso, Friederici, & Favaro, 1999).
Even fewer studies have investigated optimal cut-points on screening measures (Fairburn, et al., 2005; McKnight, 2003) and no prospective studies have used analytic procedures that can identify interactions between risk factors that may reflect qualitatively distinct risk pathways, which is important because certain etiologic theories posit that there are multiple risk pathways to the development of eating disorders (Stice, 2001; Thompson, Heinberg, Altabe, & Tantleff-Dunn, 1999). If there are qualitatively distinct vulnerability groups, it may be possible to improve the yield of prevention efforts by targeting different risk factors for these distinct vulnerability groups. Thus, the aim of this report was to use classification tree analysis (CTA) to determine empirically derived cut-points for identifying adolescent girls at risk for future onset of threshold, subthreshold, and partial eating disorders and test for interactions between risk factors that might suggest qualitatively distinct risk pathways. CTA identifies empirically determined cut-points for continuous measures that allow optimal identification of groups at elevated risk for onset of a pathological condition (Hsiao, Bartko, & Potter, 1989). We used 1-year lagged predictors, rather than baseline values of predictors, as elevated risk factors that are more proximal to onset of eating disorders should have greater predictive power. This too is a novel contribution to the literature.
The dual pathway model of eating pathology (Stice, 2001) guided our selection of risk factors examined herein. This model posits that perceived pressure to be thin from family, peers, and the media and internalization of the thin beauty ideal produces body dissatisfaction. This body dissatisfaction theoretically promotes unhealthy dieting behaviors that may progress to anorexia nervosa. Further, individuals may think dietary restriction for circumscribed periods permits them to binge eat but not gain weight, which might promote a cycle of acute restriction punctuated by overeating. Body dissatisfaction may also produce negative affect given the importance of appearance in western culture. Negative affect, in turn, might lead people to binge eating to provide comfort and distraction from negative emotions. In support, perceived pressure to be thin and thin-ideal internalization increased risk for future onset of bulimic symptoms and any eating disorder, body dissatisfaction predicted future onset of bulimic symptoms and threshold or subthreshold bulimia nervosa, and dieting and negative affect predicted future onset of bulimic symptoms, threshold or subthreshold bulimia nervosa, or any eating disorder in previous studies (Fairburn, et al., 2005; Favaro, et al., 2003; Field, Camargo, Taylor, Berkey, & Colditz, 1999; Killen, et al., 1996; McKnight, 2003; Patton, et al., 1999; Santonastaso, et al., 1999; Stice & Agras, 1998).
To address this aim we followed a cohort of females from early adolescence to young adulthood because data available when this study was initiated suggested eating disorders typically emerge during this period (Stice, et al., 2009). We focused on females because they are at much higher risk for onset of eating pathology than males (Hudson, et al., 2007). We improved upon certain limitations of past studies by using structured diagnostic interviews, minimizing attrition, and using a large sample.
Method
Participants and Procedures
Participants were 496 middle school girls (M age = 13.5, SD = 0.7) recruited from four public schools from the Austin Independent School District (n=409) and four smaller private schools (n=87) in Austin Texas. The sample was composed of 2% Asian/Pacific Islanders, 7% African Americans, 68% Caucasians, 18% Hispanics, 1% Native Americans, and 4% other/mixed and average parental education was 29% high school graduate or less, 23% some college, 33% college graduate, and 15% graduate degree, which was also representative of the sampling frame (Stice, et al., 2009).
The study was described as an investigation of adolescent mental and physical health. An informed consent letter and self-addressed return envelope were sent to parents of public and private middle school students, resulting in a participation rate of 56%, similar to recruitment rates observed in other similar longitudinal studies (Striegel-Moore, et al., 2003). Participants completed a survey and an interview at baseline and at seven annual follow-ups. Trained female assessors conducted diagnostic interviews. Assessors had to demonstrate an inter-rater agreement (κ> .80) with the project manager using tape-recorded interviews before collecting data. The University of Texas at Austin Institutional Review Board research ethics review board approved this study.
Measures
Perceived sociocultural pressure to be thinfrom family, friends, dating partners, and the media was assessed with the Perceived Sociocultural Pressure Scale (Stice & Bearman, 2001). Response options ranged from 1 = none to 5 = a lot and items were averaged for this scale and those below. This scale has shown internal consistency (α = .88), 2-week test-retest reliability (r = .93), and predictive validity for future onset of bulimic symptoms (Stice, Presnell, & Spangler, 2002)(α = .85 at T1).
Thin-ideal internalization was assessed with the Ideal-Body Stereotype Scale-Revised (Stice, Marti, Spoor, Presnell, & Shaw, 2008), which assesses agreement with statements concerning what attractive women look like. Response options ranged from 1 = strongly disagree to 5 = strongly agree. This scale has shown internal consistency (α = .89), 2-week test-retest reliability (r = .80), sensitivity to detecting effects of an eating disorder prevention program that focuses on reducing thin-ideal internalization, and predictive validity for future bulimic symptom onset (Stice, Marti, et al., 2008). (α = .81 at T1).
Body dissatisfaction was assessed with 9 items from the Satisfaction and Dissatisfaction with Body Parts Scale (Berscheid, Walster, & Bohrnstedt, 1973) that measured satisfaction with body parts that are often of concern to girls and women (e.g., waist, thighs). Response options ranged from 1 = extremely satisfied to 5 = extremely dissatisfied. This scale has shown internal consistency (α = .94), 3-week test-retest reliability (r = .90), sensitivity to detecting effects from an eating disorder prevention program, and predictive validity for future onset of bulimic symptoms (Stice, Marti, et al., 2008). (α = .94 at T1).
Dieting was assessed with the Dutch Restrained Eating Scale (van Strien, Frijters, Van Staveren, & Defares, 1986) that measures the frequency of dieting behaviors. Response options ranged from 1 = never to 5 = always. This scale has shown internal consistency (α = .95), 2-week test-retest reliability (r = .82), sensitivity to detecting effects of eating disorder prevention programs, and predictive validity for future onset of bulimia nervosa (Stice, Davis, et al., 2008; Stice, Shaw, Burton, & Wade, 2006; van Strien, et al., 1986) (α = .91 at T1), but does not correlate with objectively measured caloric intake (Stice, Sysko, Roberto, & Allison, 2010).
Negative affectivity was assessed with Buss and Plomin's (Buss & Plomin, 1984) Emotionality Scale, which measures agreement with statements regarding tendencies to become affectively distressed. Response options ranged from 1 = never true of me to 5 = always true of me. This scale showed internal consistency (α= .80 at T1), predictive validity for onset of bulimic symptoms, and convergent validity with alternative measures of emotionality (Patrick, Curtin, & Tellegen, 2002).
Depressive symptoms
An adapted version of the Schedule for Affective Disorders and Schizophrenia for School-Age Children (K-SADS) (Puig-Antich & Chambers, 1983), a semi-structured diagnostic interview, assessed DSM-IV major depression symptoms. Participants reported the peak severity of each symptom during the past year using response options ranging from 1 = not at all to 4 = severe symptoms. This interview has shown internal consistency (M α = .81), 1-week test-retest reliability (r = .86) inter-rater agreement (r = .87), and sensitivity to detecting effects of a depression prevention program for the symptom composite (Nolen-Hoeksema, Stice, Wade, & Bohon, 2007; Stice, Rohde, Gau, & Wade, 2011).
Eating pathology
The Eating Disorder Diagnostic Interview (Stice, Marti, et al., 2008) (EDDI), a semi-structured interview adapted from the Eating Disorder Examination (EDE) (Fairburn & Cooper, 1993), assessed DSM-IV eating disorders over the past 12-months at each assessment. Responses were used to determine whether participants met criteria for threshold, subthreshold, or partial eating disorders at any time during follow-up. We used DSM-IV criteria for threshold anorexia nervosa, bulimia nervosa, and binge eating disorder (American Psychiatric Assn, 1994). For subthreshold and partial eating disorder diagnoses, we used the definitions developed for an early report on the descriptive course of eating pathology in this sample (Stice, et al., 2009). For subthreshold anorexia nervosa we required participants to have a body mass index (BMI=m/kg2) that is no greater than 90% of that expected for age and gender, and to report a definite fear of weight gain more than 25% of the days for 3 months, that weight and shape were definitely an aspect of self-evaluation, and missing at least 1 period in a 3-month time frame. Height and weight were directly assessed in the 3324 diagnostic interviews conducted in person, but were based on self-report for the 534 diagnostic interviews over the phone because subjects had moved from the Austin area (13.8% of all interviews). For subthreshold bulimia nervosa we required participants to report at least 2 uncontrollable binge eating episodes and at least 2 compensatory behavior episodes (e.g., self-induced vomiting, laxatives use, fasting) per month for 3 months and that weight and shape was definitely an aspect of self-evaluation. For subthreshold binge eating disorder we required that participants report uncontrollable binge eating episodes on at least 2 days per month for 6 months, less than 1 compensatory behavior per month on average, marked distress about binge eating, and binge eating was characterized by 3 or more of the following: rapid eating, eating until uncomfortably full, eating large amounts when not physically hungry, eating alone because of embarrassment, feeling disgusted, depressed, or guilty after overeating. For purging disorder we required that participants report at least 8 episodes of self-induced vomiting or diuretic/laxative use for weight control purposes per month for 3 months, less than 1 uncontrollable binge eating episode on average per month during this period, and weight and shape was definitely an aspect of self-evaluation. Diagnoses for threshold, subthreshold, and partial eating disorders showed test-retest reliability (κ = .96) and inter-rater agreement (κ = .86) for a subset of participants in this study (Stice, et al., 2009), as well as sensitivity to detecting effects of eating disorder prevention programs (Stice, Marti, et al., 2008).
Incidence during the 8-year follow-up was 3 for anorexia nervosa, 3 for subthreshold anorexia nervosa, 6 for bulimia nervosa, 26 for subthreshold bulimia nervosa, 5 for binge eating disorder, 21 for subthreshold binge eating disorder, and 22 for purging disorder. Because subthreshold and threshold cases did not differ on impairment (i.e., mental health treatment, functional impairment, and emotional distress) and because both subthreshold and threshold cases differed from non-eating disorder participants on the same impairment measures (Stice, et al., 2009), we combined threshold and subthreshold cases for analyses. Please note that participants were not excluded from the study if they developed an eating disorder, although referral information was provided to those who developed full threshold eating disorders.
Statistical Methods
We estimated recursive partitioning conditional inference trees using Party Package software in R (Hothorn, Hornik, & Zeileis, 2006). A Bonferroni correction was used to establish a stopping criterion. A classification tree was used to predict the survival time to onset of any eating disorder (n = 52) using Kaplan Meier curves. The model contained the following independent variables: perceived sociocultural pressure, thin ideal internalization, body dissatisfaction, dieting, negative affectivity, and depressive symptoms. We used z-transformed versions of the variables so that the interpretation of split values was consistent across variables on different scales. We excluded seven participants from this model because they met criteria for an eating disorder at baseline (3 met criteria for subthreshold BN, 2 met criteria for threshold BN, and 2 met criteria for subhreshold BED), resulting in a sample of 489 participants for this model. Each of the independent variables was lagged so that it reflected the value of the independent variable at the wave prior to eating disorder onset. For participants who did not show eating disorder onset, the values of the independent variables were drawn from the second-to-last assessment for which they provided data. Thus, all independent variables were lagged by 1 year for all participants. The correlations among the independent variables at baseline are shown in Table 1. We computed odds ratios for all splits on the trees where the numerator represented the odds of disorder onset for the branch with the higher incidence and the denominator represented the group with the lower incidence. Confidence intervals were generated using the PropCIs package written for R (Scherer, 2010).
Table 1. Bivariate relations among the risk factors at baseline.
| Perceived pressure to be thin | Thin ideal internalization | Body dissatisfaction | Dietary restraint | Negative affectivity | Depressive Symptoms | |
|---|---|---|---|---|---|---|
| Perceived pressure to be thin | ||||||
| Thin ideal internalization | .28*** | |||||
| Body dissatisfaction | .53*** | .16*** | ||||
| Dietary restraint | .58*** | .26*** | .50*** | |||
| Negative affectivity | .29*** | .18*** | .31*** | .19*** | ||
| Depressive Symptoms | .30*** | .12** | .42*** | .29*** | .46*** |
Results
With respect to attrition, the percentages of participants missing self-report and diagnostic interview data from were 0% (N=496), 1% (N=491), 3% (N=481), 3% (N=481), 2% (N=486), 3% (N=481), 4% (N=476), and 6% (N=466) for each of the eight annual assessments. It should be noted that we were sometimes able to collect data from participants who did not provide data at an earlier assessment. Attrition was not significantly correlated with any of the variables examined herein.
Variables that showed significant relations to risk for onset of any eating disorder over the 7-year follow-up are depicted in Figure 1. The first split in the sample was on body dissatisfaction, indicating that this was the risk factor with the greatest predictive potency in identifying youth at risk for onset of any eating disorder. Participants in the upper 24% of body dissatisfaction showed a 4.0-fold increase in incidence for disorder onset relative to those with lower dissatisfaction scores (incidence: 24% vs. 6%; OR = 4.56, 95% CI = 2.53, 8.22). Among participants in the high body dissatisfaction branch, those in the upper 32% of depressive symptoms showed a 2.9-fold increase in incidence for any eating disorder onset relative to those with lower scores (incidence: 43% vs. 15%; OR = 4.32, 95% CI = 1.78, 10.49). Among participants in the low body dissatisfaction branch, those in the upper 12% of dieting showed a 3.6-fold increase in incidence for any eating disorder onset relative to those with lower dieting scores (incidence: 18% vs. 5%; OR = 4.33, 95% CI = 1.77, 10.65).
Figure 1. Classification tree for risk factors predicting onset of any eating disorder.
Discussion
The objective was to use CTA to determine empirically derived cut-points for identifying adolescent girls at risk for future onset of threshold, subthreshold, and partial eating disorders and test for interactions between risk factors suggestive of qualitatively distinct risk pathways, with the hope that this would allow clinicians to identify youth at greatest risk for eating pathology, which can be a challenge because of the low incidence of these conditions, and to design prevention programs that target key vulnerability factors. These results are novel because no prospective study has investigated risk factors for onset of any eating disorder during the entire period of adolescence or tested for interactions among risk factors. In addition, CTA is particularly useful because it delineates specific cut-points for identifying youth at risk for eating disorder onset for inclusion in selected prevention programs.
Body dissatisfaction was the strongest predictor of risk for onset of any eating disorder; 24% of adolescent girls in the upper 24% of body dissatisfaction showed onset of any eating disorder versus 6% of those with less body dissatisfaction. This risk was further amplified by elevated depressive symptoms, suggesting an interaction between these two risk factors. Among young girls with body dissatisfaction, 43% showed onset of any eating disorder if they were in the top 32% of depressive symptoms, versus 15% among girls with lower depressive symptoms. Among participants with low body dissatisfaction, the 12% who reported the highest dieting behaviors also showed high risk for eating disorder onset; 18% showed any eating disorder onset versus 5% among those with lower body dissatisfaction and self-reported dieting. The interaction between body dissatisfaction, depressive symptoms, and lower self-reported dieting suggests a body dissatisfaction pathway to eating disorder onset that is amplified by depressive symptoms, as well as a pathway characterized by self-reported dieting in the absence of high body dissatisfaction. As such, these results might be considered an example of equifinality, in which there are qualitatively distinct etiologic pathways to pathology (Von Bertalanffy, 1933). Interestingly, the fact that body dissatisfaction emerged in the first split and then depressive symptoms and dieting emerged as the most potent splits at the next level seems to provide support for the dual-pathway model of eating pathology (Stice, 2001).
Study limitations should be considered when interpreting these findings. First, because CTA is an exploratory data analytic technique, results should be considered provisional until replicated in an independent sample. Fortunately, the use of a strict Bonferroni correction should have effectively guarded against chance findings. Second, all of the predictors examined in this study were based on adolescent reports (from surveys or interviews). Third, a relative small number of participants showed onset of certain eating disorders and even fewer showed onset of threshold variants of these eating disorders (e.g., only 6 participants showed onset threshold/subthreshold anorexia nervosa), which is why the model focused on predicting onset of any eating disorder. Thus, results should be generalized with care to specific eating disorders, particularly specific threshold eating disorders. Fourth, we investigated a small subset of putative risk factors for eating pathology that were drawn from a single etiologic model for bulimic spectrum eating disorders. Therefore, results identify common risk factors for eating disorders, rather than disorder-specific risk factors. Considerably larger prospective studies will be necessary to identify disorder-specific risk factors for these eating disorders. Fifth, because the sample contained only females, results cannot be generalized to males. Finally, as is the case with all longitudinal research, it is possible that some unmeasured variable explains the observed prospective effects.
The findings suggest that a brief body dissatisfaction scale is the most sensitive method of identifying adolescent females at risk for onset of any eating disorder. This finding lends support to eating disorder prevention programs that target young women with body image or weight concerns (Stice, Marti, et al., 2008; Taylor et al., 2006), suggesting it would be best to target adolescent girls in the upper quartile of body dissatisfaction when implementing selective eating disorder prevention programs. Yet the present findings suggest it would also be useful to target young women who report elevated depressive symptoms and dieting for eating disorder prevention programs. As well, the present data imply that if prevention programs reduced depressive symptoms and dieting, they might be even more effective. In line with this, one cognitive behavioral depressive prevention program that effectively reduces depressive symptoms was found to also decrease eating disorder symptoms among adolescent girls (Burton, Stice, Bearman, & Rohde, 2007). However, prevention programs that have sought to reduce dieting behaviors have not produced significantly greater reductions in eating disorder symptoms than observed in controls (Bacon et al., 2002; Wadden et al., 2004).
It will be important to investigate additional risk factors that may elucidate other pathways to eating pathology. Further, because there is always a possibility that some omitted third variable explains any prospective effects observed in longitudinal studies, it will be vital to conduct randomized prevention trials that reduce suspected risk factors in order to provide an experimental test of the relation between these risk factors and these eating pathologies. It is hoped that additional large prospective risk factors studies coupled with prevention programs targeting the implicated risk factors will shed additional light on the etiologic processes that give rise to these pernicious disorders and permit the development of more effective preventive and treatment interventions.
>Classification tree analysis identifies distinct pathways for eating disorders. >We determine cut-points for identifying adolescents at risk for eating disorders. >Body dissatisfaction pathway to eating disorder onset emerged. >Risk increased with depressive symptoms. >Self-reported dieting is primary risk factor for second pathway.
Acknowledgments
Eric Stice was responsible for study design and contributed to data analysis and manuscript writing and revisions. Nathan Marti contributed to data analysis and manuscript writing and revisions. Shelley Durant contributed to manuscript writing and revisions.
This study was supported by a career award (MH01708) and a research grant (MH/DK61957) from the National Institutes of Health.
Thanks go to project research assistants Sarah Kate Bearman, Cara Bohan, Emily Burton, Melissa Fisher, Lisa Groesz, Katherine Presnell, Jenn Tristan, Natalie McKee, and Katy Whitenton, a multitude of undergraduate volunteers, the Austin Independent School District, and the participants who made this study possible.
Footnotes
The authors of this manuscript have no conflicts of interest, including financial interests relevant to the subject of this manuscript.
Exploratory analyses investigated whether this set of risk factors predicted onset of (a) threshold/subthreshold bulimia nervosa (n=27), (b) threshold/subthreshold binge eating disorder (n=21), and purging disorder (n=21).Results indicated that sociocultural pressure to be thin and body dissatisfaction emerged as predictors of onset of bulimic pathology, sociocultural pressure for thinness emerged a the sole predictor for onset of threshold/subthreshold binge eating disorder, and body dissatisfaction, thin-ideal internalization, and dietary restraint emerged as predictors of onset of purging disorder. These exploratory results suggest more similarity than differences in terms of risk factors, among the limited set of factors investigated herein.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- American Psychiatric Assn. Diagnostic and statistical manual of mental disorders. 4th. Arlington, VA, US: American Psychiatric Publishing, Inc; 1994. [Google Scholar]
- Bacon L, Keim N, Van Loan M, Derricote M, Gale B, Kazaks A, et al. Evaluating a″ non-diet'wellness intervention for improvement of metabolic fitness, psychological well-being and eating and activity behaviors. International Journal of Obesity. 2002 doi: 10.1038/sj.ijo.0802012. [DOI] [PubMed] [Google Scholar]
- Berscheid E, Walster E, Bohrnstedt G. The happy American body: A survey report. Psychology Today. 1973;7(6):119–131. [Google Scholar]
- Burton E, Stice E, Bearman SK, Rohde P. Experimental test of the affect-regulation theory of bulimic symptoms and substance use: a randomized trial. Int J Eat Disord. 2007;40(1):27–36. doi: 10.1002/eat.20292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buss AH, Plomin R. Temperament: Early developing personality traits. L. Erlbaum Associates; 1984. [Google Scholar]
- Fairburn CG, Cooper Z. Binge eating: Nature, assessment, and treatment. 12th. New York, NY, US: Guilford Press; 1993. The Eating Disorder Examination; pp. 317–360. [Google Scholar]
- Fairburn CG, Cooper Z, Doll HA, Davies BA. Identifying Dieters Who Will Develop an Eating Disorder: A Prospective, Population-Based Study. Am J Psychiatry. 2005;162(12):2249–2255. doi: 10.1176/appi.ajp.162.12.2249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Favaro A, Ferrara S, Santonastaso P. The spectrum of eating disorders in young women: a prevalence study in a general population sample. Psychosom Med. 2003;65(4):701–708. doi: 10.1097/01.psy.0000073871.67679.d8. [DOI] [PubMed] [Google Scholar]
- Field AE, Camargo CA, Jr, Taylor CB, Berkey CS, Colditz GA. Relation of peer and media influences to the development of purging behaviors among preadolescent and adolescent girls. Arch Pediatr Adolesc Med. 1999;153(11):1184–1189. doi: 10.1001/archpedi.153.11.1184. [DOI] [PubMed] [Google Scholar]
- Fisher M, Schneider M, Burns J, Symons H, Mandel FS. Differences between adolescents and young adults at presentation to an eating disorders program. Journal of Adolescent Health. 2001;28(3):222–227. doi: 10.1016/s1054-139x(00)00182-8. [DOI] [PubMed] [Google Scholar]
- Hothorn T, Hornik K, Zeileis A. Unbiased recursive partitioning. Journal of Computational and Graphical Statistics. 2006;15(3):651–674. [Google Scholar]
- Hsiao JK, Bartko JJ, Potter WZ. Diagnosing diagnoses: Receiver operating characteristic methods and psychiatry. Archives of General Psychiatry. 1989;46(7):664–667. doi: 10.1001/archpsyc.1989.01810070090014. [DOI] [PubMed] [Google Scholar]
- Hudson JI, Hiripi E, Pope HG, Jr, Kessler RC. The prevalence and correlates of eating disorders in the National Comorbidity Survey Replication. Biol Psychiatry. 2007;61(3):348–358. doi: 10.1016/j.biopsych.2006.03.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Killen JD, Taylor CB, Hayward C, Haydel KF, Wilson DM, Hammer L, et al. Weight concerns influence the development of eating disorders: a 4-year prospective study. J Consult Clin Psychol. 1996;64(5):936–940. doi: 10.1037//0022-006x.64.5.936. [DOI] [PubMed] [Google Scholar]
- McKnight I. Risk factors for the onset of eating disorders in adolescent girls: Results of the McKnight longitudinal risk factor study. The American Journal of Psychiatry. 2003;160(2):248–254. doi: 10.1176/ajp.160.2.248. [DOI] [PubMed] [Google Scholar]
- Milos G, Spindler A, Schnyder U, Fairburn CG. Instability of eating disorder diagnoses: prospective study. The British Journal of Psychiatry. 2005;187(6):573–578. doi: 10.1192/bjp.187.6.573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nolen-Hoeksema S, Stice E, Wade E, Bohon C. Reciprocal relations between rumination and bulimic, substance abuse, and depressive symptoms in female adolescents. J Abnorm Psychol. 2007;116(1):198–207. doi: 10.1037/0021-843X.116.1.198. [DOI] [PubMed] [Google Scholar]
- Patrick CJ, Curtin JJ, Tellegen A. Development and validation of a brief form of the Multidimensional Personality Questionnaire. Psychological Assessment. 2002;14(2):150. doi: 10.1037//1040-3590.14.2.150. [DOI] [PubMed] [Google Scholar]
- Patton GC, Selzer R, Coffey C, Carlin JB, Wolfe R. Onset of adolescent eating disorders: population based cohort study over 3 years. BMJ. 1999;318(7186):765–768. doi: 10.1136/bmj.318.7186.765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Puig-Antich J, Chambers W. Schedule for affective disorders and schizophrenia for school-age children (6ñ18 years) Pittsburgh: Western Psychiatric Institute; 1983. [Google Scholar]
- Santonastaso P, Friederici S, Favaro A. Full and partial syndromes in eating disorders: A 1-year prospective study of risk factors among female students. Psychopathology. 1999;32(1):50–56. doi: 10.1159/000029067. [DOI] [PubMed] [Google Scholar]
- Scherer R. 2 PropCIs-package. Computes confidence intervals for single proportions, for. 2010;15(1):2. [Google Scholar]
- Stice E. A prospective test of the dual-pathway model of bulimic pathology: mediating effects of dieting and negative affect. J Abnorm Psychol. 2001;110(1):124–135. doi: 10.1037//0021-843x.110.1.124. [DOI] [PubMed] [Google Scholar]
- Stice E, Agras WS. Predicting onset and cessation of bulimic behaviors during adolescence: A longitudinal grouping analysis. Behavior Therapy. 1998;29(2):257–276. [Google Scholar]
- Stice E, Bearman SK. Body-image and eating disturbances prospectively predict increases in depressive symptoms in adolescent girls: a growth curve analysis. Dev Psychol. 2001;37(5):597–607. doi: 10.1037//0012-1649.37.5.597. [DOI] [PubMed] [Google Scholar]
- Stice E, Davis K, Miller NP, Marti CN. Fasting increases risk for onset of binge eating and bulimic pathology: a 5-year prospective study. J Abnorm Psychol. 2008;117(4):941–946. doi: 10.1037/a0013644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E, Marti CN, Shaw H, Jaconis M. An 8-year longitudinal study of the natural history of threshold, subthreshold, and partial eating disorders from a community sample of adolescents. J Abnorm Psychol. 2009;118(3):587–597. doi: 10.1037/a0016481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E, Marti CN, Spoor S, Presnell K, Shaw H. Dissonance and healthy weight eating disorder prevention programs: long-term effects from a randomized efficacy trial. J Consult Clin Psychol. 2008;76(2):329–340. doi: 10.1037/0022-006X.76.2.329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E, Presnell K, Spangler D. Risk Factors for Binge Eating Onset in Adolescent Girls: A 2 Year Prospective Investigation. Health Psychology. 2002;21(2):131–138. [PubMed] [Google Scholar]
- Stice E, Rohde P, Gau J, Wade E. Efficacy trial of a brief cognitive-behavioral depression prevention program for high-risk adolescents: Effects at 1- and 2-year follow-up. Journal of Consulting and Clinical Psychology. 2011 doi: 10.1037/a0020544. On-line advance publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E, Shaw H, Burton E, Wade E. Dissonance and healthy weight eating disorder prevention programs: A randomized efficacy trial. Journal of Consulting and Clinical Psychology. 2006;74:263–275. doi: 10.1037/0022-006X.74.2.263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E, Shaw H, Marti CN. A meta-analytic review of eating disorder prevention programs: encouraging findings. Annu Rev Clin Psychol. 2007;3:207–231. doi: 10.1146/annurev.clinpsy.3.022806.091447. [DOI] [PubMed] [Google Scholar]
- Stice E, Sysko R, Roberto CA, Allison S. Are dietary restraint scales valid measures of dietary restriction? Additional objective behavioral and biological data suggest not. Appetite. 2010;54(2):331–339. doi: 10.1016/j.appet.2009.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Striegel-Moore RH, Dohm F, Kraemer H, Schreiber GB, Taylor CB, Daniels S. Risk factors for binge-eating disorders: an exploratory study. Int J Eat Disord. 2007;40(suppl 6):481–487. doi: 10.1002/eat.20400. [DOI] [PubMed] [Google Scholar]
- Striegel-Moore RH, Seeley JR, Lewinsohn PM. Psychosocial adjustment in young adulthood of women who experienced an eating disorder during adolescence. Journal of the American Academy of Child & Adolescent Psychiatry. 2003;42(5):587–593. doi: 10.1097/01.CHI.0000046838.90931.44. [DOI] [PubMed] [Google Scholar]
- Taylor CB, Bryson S, Luce KH, Cunning D, Doyle AC, Abascal LB, et al. Prevention of eating disorders in at-risk college-age women. Archives of General Psychiatry. 2006;63(8):881. doi: 10.1001/archpsyc.63.8.881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson J, Heinberg LJ, Altabe M, Tantleff-Dunn S. Exacting Beauty: theory, assessment and treatment of body image disturbance. Washington, DC: American Psychological Association; 1999. [Google Scholar]
- van Strien T, Frijters JE, Van Staveren WA, Defares PB. The predictive validity of the Dutch Restrained Eating Scale. International Journal of Eating Disorders. 1986;5(4):747–755. [Google Scholar]
- Von Bertalanffy L. Modern theories of development: An introduction to theoretical biology 1933 [Google Scholar]
- Wadden TA, Foster GD, Sarwer DB, Anderson DA, Gladis M, Sanderson RS, et al. Dieting and the development of eating disorders in obese women: results of a randomized controlled trial. The American journal of clinical nutrition. 2004;80(3):560. doi: 10.1093/ajcn/80.3.560. [DOI] [PubMed] [Google Scholar]